Quick transition Treatment of heart attack
Myocardial infarction (heart attack) is an acute, life-threatening condition caused by a decrease or complete cessation of blood supply to the heart as a result of blocking one of the coronary arteries with a blood clot (thrombus) and the development of one or more foci of necrosis in the heart muscle.
A heart attack is a clinical form of coronary heart disease (CHD), a disease characterized by impaired blood supply to the myocardium as a result of damage to the coronary arteries.
A patient with symptoms of myocardial infarction needs emergency pre-medical and medical care. Not only his successful recovery from a heart attack, but also his life depends on this.
A heart attack can occur at rest (rest or sleep), after intense physical activity, with increased activity in cold weather, after severe emotional or physiological stress (including various diseases).
General information about myocardial infarction
Myocardial infarction
ー this is the death of a section of the heart muscle, which occurs due to a lack of blood supply. As a rule, a heart attack does not develop suddenly; it is preceded by coronary heart disease or other pathology of the organ that leads to disruption of blood flow to the myocardium. Under conditions of oxygen and energy starvation, cells die. At the initial stage, this process is reversible; if blood flow is restored, the area of death can be limited and severe heart failure can be prevented.
Supporting rehabilitation results
Rehabilitation after myocardial infarction is a difficult, but positive and fruitful path. Once you pass it, there is no turning back. Only forward to an active and happy life! To do this, it is necessary to maintain the results obtained:
- lead a healthy lifestyle,
- exercise,
- follow a diet and take heart-supporting medications,
- be regularly monitored by specialists.
Classification of myocardial infarction
Depending on which part of the heart wall is damaged, the following types of heart attacks are distinguished:
- intramural ー the dying zone is located deep in the myocardium;
- transmural - affects the entire thickness of the wall;
- subendocardial - the lesion is located near the inner lining of the heart;
- subepicardial - near the outer sac of the heart.
According to the nature of the flow, they are distinguished:
- acute infarction (primary);
- recurrent, develops within 2 months after acute;
- repeated, develops later than 2 months after the first heart attack.
According to the nature of the symptoms:
- typical form, characterized by chest pain radiating to the left arm and left half of the body;
- atypical forms (abdominal ー abdominal pain, asthmatic ー accompanied by severe shortness of breath, cerebral ー with dizziness, confusion, edematous, peripheral ー pain in the arm, face, neck, painless, combined).
Mechanism of development and causes of myocardial infarction
The lion's share of heart attacks develops against the background of atherosclerotic damage to the coronary vessels and aorta (formation of cholesterol plaques in the wall of blood vessels). Other possible causes of circulatory disorders in the heart muscle are vasospasm and thrombosis. All this leads to the fact that the cells do not receive the required amount of oxygen and die.
The main causes of myocardial infarction:
- coronary heart disease, atherosclerosis;
- sudden physical activity or stress during ischemic heart disease;
- thrombosis of the coronary arteries.
Causes of impaired urine outflow from the kidney
Urological:
- Urolithiasis (kidney, ureteral stones)
- Malignant tumors (ureter, bladder, prostate)
- Benign prostate adenoma (BPH)
- Retroperitoneal fibrosis (Ormond's disease)
Non-urological:
- Spread of tumors from other locations to the ureters
- Hematological (lymphomas, lymphadenopathy)
- Iatrogenic (due to the fault of doctors, for example, during an operation in the pelvis there was damage to the ureter)
Myocardial infarction in children
It is believed that this pathology only affects older people, but this is not so. A heart attack can also occur in a child in the following cases:
- inflammation of the coronary arteries in infectious diseases, rheumatoid arthritis, lupus and other autoimmune pathologies;
- infectious and rheumatic endocarditis (after a sore throat, for example);
- abnormalities in the structure of heart vessels;
- heart injuries;
- pheochromocytoma - a tumor that constantly produces adrenaline;
- congenital heart defects;
- heart tumors.
Indications for referral to hospitalization
All patients referred by a cardiologist are accepted for treatment in the cardiology department of our clinic.
Planned hospitalization to the cardiology department is carried out for the following indications.
- Arterial hypertension stages 2-3, crisis course (not amenable to drug correction within 2 weeks).
- Symptomatic arterial hypertension, requiring clarification of the causes.
- Frequent (more than 3 times a week for 2 weeks) hypertensive crises with adequately prescribed treatment.
- Chronic ischemic heart disease in the stage of decompensation.
- Planned rehabilitation after cardiac surgery.
- Congenital and acquired heart defects that require examination in a hospital setting. Including before surgical treatment. Such patients are managed by cardiologists at our clinic with mandatory consultation with cardiac surgeons from leading cardiology centers in Moscow. Subsequently, they are transferred there for surgical treatment. After discharge, all patients should continue to be monitored by their primary care physician.
- Rhythm disturbances that are not life-threatening and require treatment adjustments.
- Preparation for setting pacemakers.
- Other non-emergency heart diseases requiring specialized diagnostic tests in a hospital setting
Hospitalization to the cardiology department is carried out if all necessary documents are available. As a rule, this is a referral from a doctor and (if necessary) a minimum set of tests.
Risk factors for myocardial infarction
The following factors lead to the development of atherosclerosis, ischemic heart disease and, as a consequence, heart attack:
- high blood cholesterol (due to poor diet or metabolic diseases);
- obesity;
- hypertonic disease;
- smoking;
- sedentary lifestyle;
- diabetes.
Chronic diseases (we mentioned some of them above, let’s summarize them again)
- hypertonic disease
- obesity
- sleep apnea
- diabetes
- dyslipidemia
- exacerbation of any chronic disease: bronchial asthma, chronic pancreatitis, ulcerative colitis, etc.
- any acute (pneumonia, stroke, acute appendicitis) or chronic uncorrected pathology (anemia, i.e. reduced hemoglobin level, decompensation of diabetes mellitus)
- Oncological diseases are a tremendous stress for the patient. Used radiation therapy aimed at the chest organs increases the risk of developing atherosclerosis and plaque deposition in the vessels of the heart. A number of chemotherapy drugs increase blood viscosity and provoke thrombosis in the vessels of the heart
Conclusion eleven: it is necessary to undergo an annual examination in order to detect serious diseases in time and avoid their adverse consequences.
Symptoms of myocardial infarction
Myocardial cells do not die immediately, since hypoxia develops gradually; they “suffer” for 1-2 hours before final death. At this time, they can still be saved, so timely seeking help determines the further outcome.
Pre-infarction state
Warning signs of a heart attack may appear several hours or even days before the attack. By seeking medical help during this period, you can prevent a disaster.
Possible signs of an impending heart attack:
- the appearance of chest pain during physical activity, emotional stress;
- sensations of interruptions in heart function, dizziness, increased heart rate;
- increased frequency of angina attacks;
- Chest pain is not relieved by nitroglycerin tablets.
Important!
Among all registered myocardial infarctions, about 20% are fatal within the first hour of the attack. It is not the doctors or “neglected medicine” that are to blame for this; death occurs even before seeking help due to the fact that the patient himself and those around him cannot recognize the attack and hesitate to call an ambulance. Therefore, if your loved ones have an increased risk of developing a heart attack, study the symptoms and algorithm of actions in case of a heart attack.
Symptoms of acute myocardial infarction
Myocardial infarction is manifested by pain. The pain is localized in the chest, radiating to the left arm, shoulder, half of the face, and side. The nature of the pain is pressing, burning. During an attack, a person feels a lack of air, fear of death, cold sticky sweat appears, and the skin turns pale.
A distinctive feature of a heart attack from angina pectoris: with the first, the pain does not subside at rest or after taking nitroglycerin, lasting more than 20 minutes.
Duration of hospitalization by referral
The duration of hospitalization in the cardiology department by referral is determined by two important factors. This is the patient’s well-being and the nature of his illness. This fundamentally distinguishes us from government institutions, where treatment periods are determined by standards adopted by the Ministry of Health.
Sometimes the hospitalization period may increase due to the need for special research methods. They may be greatly needed in the future during dynamic monitoring of the patient by a cardiologist.
Make an appointment
Please enter your details
Diagnosis of myocardial infarction
After hospitalization, the patient undergoes the following diagnostic measures:
- ECG;
- clinical and biochemical blood test;
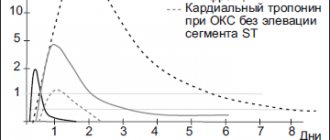
- blood test for creatine phosphokinase (CPK), lactate dehydrogenase (LDH), troponin;
- EchoCG (ultrasound of the heart);
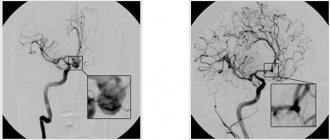
- coronary angiography.
These methods help confirm the diagnosis of a heart attack, clarify the location of the necrosis focus, and determine treatment tactics.
Forecast and prevention of heart attack
The greatest mortality from myocardial infarction is observed in the first day; therefore, if medical care was provided in a timely manner, the chances of recovery increase significantly. The overall prognosis depends on the area of damage to the heart muscle.
For prevention, you must follow these principles:
- quitting smoking and alcohol;
- proper, balanced nutrition;
- regular physical activity (check with your doctor);
- regular preventive visits to a cardiologist in the presence of diseases of the cardiovascular system.
Diagnosis and treatment of myocardial infarction and pre-infarction condition in Medical
When should you see a doctor?
A person needs to consult a cardiologist if symptoms of a cardiovascular system pathology appear (chest pain, dizziness, cough, shortness of breath, bluish skin, etc.). You should not self-medicate. Numerous methods of traditional medicine are permissible for use only after the doctor’s permission and after treatment of the acute period of the disease.
Drug treatment of myocardial infarction and pre-infarction condition
Patients in a pre-infarction state are prescribed drugs that improve blood supply to the heart muscle, anti-atherosclerotic agents, and vitamin-mineral complexes.
In the acute period of a heart attack, analgesics, anticoagulants (prevent blood clotting) and thrombolytics (dissolve an already formed blood clot) are indicated.
Surgery
It is possible to more effectively restore blood supply to the myocardium through surgical intervention, which must be carried out in the first hours of a heart attack, then the chances of successful healing are greatest.
Coronary artery bypass grafting
The method of operation is to create a bypass route for blood supply to the affected area of the myocardium. The aorta and coronary vessel beyond the blockage are connected using a section of vein taken from the patient's lower leg.
Coronary artery angioplasty
Narrowing of the artery can be relieved by inserting an instrument that widens the artery through the femoral vein. Next, a stent is installed, which fixes the shape of the vessel, preventing its narrowing and restoring blood flow.