Myocardial infarction
Diabetes
Atherosclerosis
8074 16 February
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Myocardial infarction: causes, symptoms, diagnosis and treatment methods.
Definition
Myocardial infarction (MI) is the necrosis of an area of the heart muscle due to insufficient blood supply with the development of a characteristic clinical picture.
Causes of myocardial infarction
The heart is a hollow muscular organ shaped like a cone. The walls of the heart consist of three layers. The inner layer - the endocardium - lines the cavities of the heart from the inside, and its outgrowths form the heart valves. The middle layer, the myocardium, consists of cardiac muscle tissue. The outer layer is the pericardium. The human heart has four chambers: two atria and two ventricles. The right atrium receives blood from the tissues of the heart itself and all parts of the body (through the superior and inferior vena cava). Four pulmonary veins flow into the left atrium, carrying arterial blood from the lungs. The pulmonary trunk emerges from the right ventricle, through which venous blood enters the lungs. The aorta emerges from the left ventricle, carrying arterial blood to the vessels of the systemic circulation. Oxygen is delivered to the myocardium of the heart through the coronary arteries.
The heart is very sensitive to lack of blood supply (oxygen deficiency). In the case of blockage of a large coronary artery and in the absence of effective alternative blood circulation through other vessels, within 30 minutes the death of cardiomyocytes (muscle cells of the heart) begins in the affected area.
Poor circulation due to atherosclerotic lesions of the coronary arteries in 97-98% of cases is of primary importance in the occurrence of myocardial infarction.
Atherosclerosis can affect either one coronary artery or all three. The degree and extent of narrowing of the artery can vary. When blood pressure increases, the sclerotic inner layer of the vessel (endothelium) is easily damaged, blood penetrates into the plaque, the blood clotting process is activated and a blood clot is formed, which can partially or completely block the vessel.
Where a blood clot can form:
- at the site of rupture of a vulnerable (unstable) atherosclerotic plaque;
- on a defect (erosion) of the endothelium of the coronary artery, not necessarily localized on the surface of the atherosclerotic plaque;
- at the site of hemodynamically insignificant narrowing of the coronary artery.
Coronary artery thrombosis occurs with complete or incomplete parietal occlusion. A thrombus located proximally (closer to the center) in the coronary artery tends to be transported with the blood flow more distally (closer to the vessel wall) and lead to the formation of small foci of necrosis and/or contribute to the expansion of the main area of necrosis.
Great importance in the development of myocardial infarction is attached to the development of spasm of the coronary arteries both with atherosclerosis and with unchanged vessels.
Developing myocardial necrosis can be of various sizes, and necrosis passing through all layers of the heart (transmural) can cause myocardial rupture.
The formation of foci of necrosis in the myocardium is accompanied by changes in the size, shape and thickness of the heart wall, and the remaining myocardium experiences increased stress and undergoes hypertrophy with an increase in volume and mass.
Concomitant conditions such as anemia, inflammation, infection, fever, metabolic or endocrine disorders (in particular, hyperthyroidism) can provoke or aggravate myocardial ischemia.
Risk factors for developing myocardial infarction include:
- hyperlipidemia (violation of the normal ratio of blood lipids);
- smoking,
- diabetes,
- arterial hypertension,
- abdominal obesity,
- psychosocial reasons (stress, depression, etc.),
- low physical activity,
- unbalanced diet and alcohol consumption.
Recurrent myocardial infarction occurs within 28 days of the initial myocardial infarction.
If myocardial infarction develops at a later date, they speak of recurrent myocardial infarction. Classification of myocardial infarction
I. Acute myocardial infarction.
- Acute transmural infarction of the anterior myocardial wall.
- Acute transmural infarction of the lower myocardial wall.
- Acute transmural myocardial infarction of other specified locations.
- Acute transmural myocardial infarction of unspecified localization.
- Acute myocardial infarction, unspecified.
II. Repeated myocardial infarction.
- Repeated infarction of the anterior myocardial wall.
- Repeated infarction of the lower myocardial wall.
- Repeated myocardial infarction of another specified location.
- Repeated myocardial infarction of unspecified localization.
III. Some current complications of acute myocardial infarction.
- Hemopericardium.
- Atrial septal defect.
- Ventricular septal defect.
- Rupture of the heart wall without hemopericardium.
- Rupture of the tendinous chord.
- Rupture of the papillary muscle.
- Thrombosis of the atrium, atrial appendage and ventricle of the heart.
- Other current complications of acute myocardial infarction.
IV. Other forms of acute coronary heart disease.
- Coronary thrombosis not leading to myocardial infarction.
- Dressler's syndrome is post-infarction sclerosis.
- Other forms of acute coronary heart disease.
- Acute coronary heart disease, unspecified.
V. Previous myocardial infarction.
Symptoms of myocardial infarction
During myocardial infarction, as a result of circulatory disorders, metabolic products accumulate in the affected area of the heart, which irritate the receptors of the myocardium and coronary vessels, which is manifested by acute pain. A painful attack leads to the release of adrenaline and norepinephrine from the adrenal cortex.
Pain in the typical course of myocardial infarction is its main symptom. It arises behind the sternum, sometimes it can radiate to the left arm, left shoulder, throat, lower jaw, and to the epigastric region.
In intensity and duration, such pain significantly exceeds a regular angina attack. The pain is not relieved by taking nitroglycerin. The duration of the pain syndrome can vary - from 1 hour to several days. Sometimes myocardial infarction is accompanied by severe weakness, dizziness, headache, vomiting, and loss of consciousness. The patient looks pale, lips turn blue, and sweating occurs.
On the first day of myocardial infarction, tachycardia (rapid heartbeat), rhythm disturbance, and temperature rise to 37-38℃ may be recorded.
In 30% of cases, myocardial infarction in the first hours of its development may manifest itself atypically.
The following clinical options are distinguished:
- asthmatic - occurs as an attack of bronchial asthma (there is shortness of breath, difficulty breathing, a feeling of lack of air);
- gastralgic - characterized by pain in the stomach spreading to the retrosternal space, there may be belching, hiccups, nausea, repeated vomiting, bloating;
- arrhythmic - life-threatening heart rhythm disturbances occur;
- cerebral – characterized by impaired cerebral circulation (nausea, dizziness, impaired consciousness with the development of fainting are observed);
- asymptomatic - myocardial infarction without a typical pain attack. Due to non-compliance with bed rest and lack of proper treatment, the course is unfavorable.
Diagnosis of myocardial infarction
There are clear criteria for diagnosing myocardial infarction:
- clinical picture of myocardial infarction;
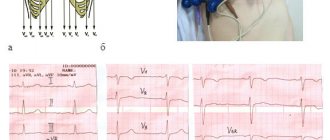
- picture of myocardial infarction according to ECG data;
- the presence of new areas of the myocardium with reduced blood circulation or impaired myocardial contractility according to instrumental studies;
- detection of coronary artery thrombosis according to angiography.
To confirm the diagnosis, the following laboratory tests are performed:
- determination of the level of biochemical markers of cardiomyocyte damage in the blood;
Reciprocal ST segment depression
ST segment depression in leads opposite the affected area, otherwise known as reciprocal depression, is a highly sensitive indicator of AMI. The pathogenesis of reciprocal changes remains unknown. Reciprocal changes have high sensitivity and a positive predictive value of up to 90% and are observed in approximately 70% of lower and up to 30% of infarcts involving the anterior wall of the LV, although, of course, their absence does not exclude the diagnosis of AMI [4, 5]. As a rule, ST segment depression is horizontal or oblique. The presence of reciprocal changes is especially important when there is doubt about the clinical significance of the recorded ST segment elevation. We especially note that reciprocal changes may be the only sign of AMI against the background of still unobvious ST segment elevation. Similar situations often occur in cases of myocardial infarction with damage to the lower wall. The presence of severe ST segment depression in the precordial leads against a background of normal heart rate or bradycardia in a patient with an ischemic painful attack strongly requires the exclusion of AMI.
ECG predictors of reperfusion
Pathogenetic therapy for AMI has the goal of restoring blood flow in the affected artery. Lack of restoration of blood flow (reperfusion) is the most powerful predictor of the development of LV systolic dysfunction and the risk of death after AMI. In the absence of reperfusion, 30-day mortality can reach 15% [14]. In turn, the resolution of ST segment elevation is an indicator of improved short-term (30-day) and long-term (one-year) prognosis [5]. Assessing ST segment resolution is also useful for deciding on further management of the patient.
Failure to resolve the ST segment within the first 90-120 minutes after thrombolytic administration should be a reason to consider angioplasty. A specific marker of reperfusion that has occurred is considered to be a reduction in ST segment elevation by more than 50-70% in the lead with maximum elevation, which is associated with the most favorable further prognosis. At the same time, a number of authors propose a criterion of 50% reduction in ST segment elevation after 60 minutes of reperfusion therapy as a predictor of a good prognosis in individuals with AMI [13]. Considering that the maximum effect from subsequent angioplasty after thrombolysis is achieved no later than 6-8 hours from the onset of AMI [14], reducing the time for assessing reperfusion has good reason.
Other ECG markers of reperfusion include T wave inversion within four hours of AMI onset. T wave inversion, which occurs within the first hours of reperfusion therapy, is a highly specific sign of restoration of blood flow. T wave inversion, which develops after more than four hours, is associated with natural ECG dynamics during AMI and does not indicate restoration of blood flow. Accelerated idioventricular rhythm 60-120 beats/min, late, paired, ventricular extrasystoles are also a highly specific marker of reperfusion. These rhythms are considered not dangerous and, as a rule, do not require antiarrhythmic therapy. Polymorphic ventricular tachycardia and ventricular fibrillation can also be associated with reperfusion, but are rare and more often a consequence of persistent coronary occlusion.
First aid
In order to promptly independently determine the possible development of the pathology in question, it is very important to pay attention to:
- intensity and nature of pain. a heart attack is characterized by squeezing, pressing, burning sensations;
- localization of pain. location of pain in the left side of the body, just behind the sternum, in the area of the shoulders, shoulder blades;
- irradiation of pain to the arm, side, neck.
But in order to really help a patient with an angina attack, the first thing that is very important to do is, of course, to call a medical team. The sooner doctors have the opportunity to begin their work, the greater the patient’s chances of surviving and avoiding the sad complications of the primary problem.
The first pre-medical treatment or simply assistance to the patient should be as follows:
- It is important for the patient to take a comfortable body position; he can be laid down or seated comfortably, allowed to lean back on the pillow;
- unbutton tight clothes;
- provide air flow, open windows;
- You can give the patient one tablet of nitroglycerin or aspirin.
Further actions should be carried out by the resuscitation team. Unfortunately, it is extremely difficult to teach people without medical education to perform chest compressions and artificial respiration, which may also be urgently needed by patients in such situations.
Typical course
To be able to avoid the most severe complications of a heart attack, it is advisable to know and remember the classic symptoms of the development of this pathology.
These symptoms usually include:
- sudden development of acute chest pain, with a burning, often pressing or squeezing character;
- irradiation of pain to the pericardial region (irradiation to the left side of the chest, left arm or under the left shoulder blade);
- situations when the described pain is accompanied by a panic attack, acute fear of death.
It is important to remember that the slightest suspicion of the development of myocardial infarction should force the patient to urgently consult a doctor to receive specialized treatment aimed at opening a narrowed, closed (stenotic) vessel to prevent the development of extensive necrosis of the heart muscles.
Although a heart attack is always an unexpected heart attack, it is not difficult to recognize. Its symptoms cannot be confused with any other disease. Do not forget that a heart attack is life-threatening. Timely help can save a person, but its absence will lead to death. An ambulance must be called as quickly as possible.
Expert advice
When the first signs of a heart attack appear, measures should be taken immediately.
I advise you to immediately call an ambulance, and while the doctor is on the way, provide the patient with complete rest, sit him down or put him in a position that will alleviate the condition as much as possible. Give Corvalol, Nitroglycerin, Aspirin, ventilate the room. The most dangerous period is the most acute period, which is usually manifested by very severe pain, shortness of breath, and rhythm disturbances. The patient’s life depends on the speed and correctness of the actions of the person nearby. When calling a doctor, it is best to describe the symptoms so that a specialized team can arrive to take an ECG, give oxygen, and administer medications to limit the area of necrosis.