Features of acute myocardial infarction and its symptoms
Acute myocardial infarction is the death of a section of the heart muscle caused by a circulatory disorder. Heart attack is one of the main causes of disability and mortality among adults.
Causes and mechanisms of vascular incompetence of the heart
A heart attack can be considered an acute form of coronary heart disease or its complication.
The peculiarities of the heart - constant contractions of the myocardium - determine a very high level of metabolic processes in its cells, high consumption of oxygen and nutrients. This mode of activity requires an uninterrupted flow of highly oxygenated (oxygen-rich) blood, which is provided by an extensive network of cardiac vessels starting from the aorta in the form of coronary (coronary) arteries.
The downside to the effectiveness of the heart muscle is its high sensitivity to oxygen starvation. If there is a malnutrition in the myocardium, pathological phenomena develop that very quickly become irreversible.
If the lack of blood flow is not critical, reversible ischemia (anemia) of the heart muscle occurs, which is manifested by anginal pain in the chest. When the flow of blood to a certain area is completely stopped, a cascade of pathological processes develops - the accumulation of toxic metabolic products that are not excreted, the transition to an anaerobic (oxygen-free) mode of operation using the internal energy reserves of cells.
The body's own reserves of energy carriers (glucose and ATP) are very quickly (in about 20 minutes) depleted, and the bloodless section of the heart muscle dies. This is myocardial infarction - necrosis, the size of which depends on the level of vessel occlusion (large or small branch), the rate of onset of ischemia (with gradual cessation of blood supply, partial adaptation is possible), the patient’s age and many other factors. For example, acute transmural myocardial infarction (with necrosis of the entire thickness of the heart muscle), which has a very severe course, develops when a large branch of a coronary vessel is occluded (blocked).
Among the causes of impaired blood supply to the myocardium, the most common is a block of the lumen of the vessel by an atherosclerotic plaque or thrombus (these phenomena can be combined) . In addition, a sharp spasm of the coronary arteries is possible under the influence of physical (cold) or chemical (poisons, drugs) factors. Severe anemia, in which there is a sharp decrease in the content of hemoglobin in the blood, and, consequently, its ability to transport oxygen, can also cause myocardial ischemia. Inconsistency of blood supply with increased needs occurs with sudden hypertrophy of the heart muscle - cardiomyopathy.
Predisposing factors for the development of heart attack
Some diseases and pathological conditions are increased risk factors for the development of acute myocardial ischemia. These include:
- Diabetes.
- Hypertonic disease.
- Coronary heart disease (CHD), manifested by attacks of angina (especially its unstable forms).
- Increased levels of cholesterol and some fractions of lipoproteins in the blood.
- Excessive body weight.
- Smoking.
- Alcohol abuse.
- Errors in diet (high consumption of salt, animal fats).
- Cardiac arrhythmia.
- Prolonged stressful situations.
- Age over 60 years (although in recent years there has been a “rejuvenation” of heart attacks).
- Male gender (after 70 years, the number of men and women suffering from a heart attack equalizes).
Classification of ischemic myocardial injury
There are different criteria for classifying a heart attack. Some of them:
- The size of the damage zone is large-focal and small-focal.
- According to the depth of damage to the heart muscle - transmural (throughout the entire thickness of the heart wall), intramural (necrosis in the thickness of the wall), subendocardial (damage to the inner layer), subepicardial (outer layer).
- According to topography - left ventricular (anterior wall, posterior and lateral walls, interventricular septum), right ventricular.
Symptoms of a heart attack
In the development of the pathological process, several periods are distinguished, each of which has its own duration and symptoms.
The pre-infarction period can last from several minutes to months. It is characterized by an increase in the frequency of angina attacks and an increase in their intensity.
The most acute period , in which ischemia and necrosis of the heart muscle develops, lasts up to several hours. It may have a typical or atypical course.
The painful, or anginal, variant is typical (about 90% of all cases). It is characterized by high-intensity pain behind the sternum of a burning or pressing nature, which can radiate (give) to the left limbs, jaw, and neck. There may be fear of death, sweating, pale or reddened facial skin, and shortness of breath. The severity of pain depends on the size of the affected area - large-focal infarction causes more severe symptoms than small-focal infarction. The pain is not relieved by taking nitroglycerin.
Atypical variants can occur in the asthmatic type (have symptoms of an attack of bronchial asthma), abdominal (with symptoms of an acute abdomen), arrhythmic (in the form of an attack of cardiac arrhythmia), cerebral (with impaired consciousness, dizziness, paralysis, visual impairment).
The acute period lasts about 10 days. The necrosis zone is finally formed and delimited, absorption of decay products and scar formation begins. The pain syndrome disappears or decreases. Possible increase in temperature, hypotension and heart failure.
The subacute period (about two months) is the stage of scar formation and thickening. There is no pain syndrome, the condition is gradually improving. Well-being in this period is largely determined by the nature and extent of changes that have occurred in the heart muscle.
The post-infarction period , or rehabilitation (up to six months), is characterized by the absence of clinical and laboratory signs of a heart attack (changes on the ECG remain - they will remain for life), however, in this phase, the development of heart failure, angina pectoris and recurrent heart attack is possible.
Complications of myocardial infarction
Acute myocardial ischemia, being a serious condition in itself, can be further aggravated by the addition of complications.
The most common complications:
- Heart rhythm disturbances (paroxysmal tachycardia, extrasystole, atrial fibrillation). A situation such as the appearance of ventricular fibrillation with the transition to fibrillation can cause the death of the patient.
- Heart failure is associated with a disruption in the activity of the left ventricle in pumping blood through the vessels. It can lead to pulmonary edema, cardiogenic shock and death due to a sharp drop in pressure and cessation of renal filtration.
- Pulmonary embolism can lead to pneumonia, pulmonary infarction, and death.
- Cardiac tamponade can occur when the heart muscle ruptures in the area of the infarction and blood leaks into the pericardial cavity. The condition is life-threatening and requires immediate attention.
- Acute cardiac aneurysm is a bulging area of scar tissue with extensive damage to the myocardium. In the future, it can cause the development of heart failure.
- Thromboendocarditis is the deposition of fibrin on the inner surface of the heart. Its separation can cause a stroke, mesenteric thrombosis (closure of a branch of the vessel feeding the intestine) with subsequent necrosis of a section of the intestine, and kidney damage.
- Post-infarction syndrome is the general name for long-term complications (pericarditis, pleurisy, arthralgia).
Diagnosis of heart attack
In the diagnosis of a heart attack, data from anamnesis (circumstances of the course of the disease and previous life, ascertained by interviewing the patient and his relatives), laboratory and instrumental research methods are important.
Anamnesis
Past attacks of chest pain of varying frequency and intensity, as well as risk factors (smoking, stress, chronic diseases) are identified. During examination, it is possible to identify excess weight, indirect signs of high blood pressure (capillary network on the face), etc. Substernal pain lasting more than 20 minutes is considered one of the diagnostic criteria for a heart attack.
Laboratory methods
Laboratory research methods for a heart attack reveal the following changes:
- Blood clinic. Leukocytosis (increased number of leukocytes), increased ESR.
- Biochemistry of blood. Increased activity of the enzymes AlT, AST, LDH, creatine kinase, myoglobin, which is an indicator of damage to the heart muscle. Changes in the level of electrolytes and iron are possible.
Instrumental research methods
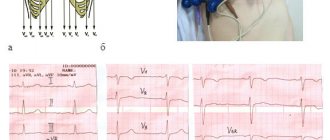
- ECG – characteristic signs of a heart attack (negative T wave, pathological QRS complex, etc.). Taking a cardiogram in different leads helps determine the location of the necrotic focus (for example, the anterior or posterior wall of the left ventricle, etc.).
- EchoCG – local (limited) violation of contractility of the affected ventricle.
- Coronary angiography reveals narrowing or blockage of the vessel supplying the myocardium. It should be noted that when carrying out this research method, it can also be used to provide assistance (after supplying a contrast agent through the same catheter, a drug is injected into the vessel or an expander stent is installed).
Treatment of myocardial infarction
Emergency care (performed directly during a painful attack and then in a specialized clinic):
- Providing the patient with complete rest.
- Give sublingual (under the tongue) nitroglycerin and Corvalol orally.
- Immediate transportation for further treatment to the cardiac intensive care unit (preferably on specialized resuscitation transport).
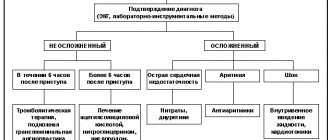
Specialized treatment
- Relief of pain syndrome (narcotic analgesics and antipsychotics are used).
- Dissolution of a blood clot located in a coronary vessel by introducing special thrombolytic agents (streptase, cabinase). The method is very effective, but has a time limit - assistance must be provided within the first hour after the attack; subsequently, the percentage of saved myocardial mass rapidly decreases.
- Antiarrhythmic drugs.
- Improving metabolic processes in the heart muscle.
- Reducing the volume of circulating blood to reduce the load on the heart.
- Surgical methods of treatment - balloon angioplasty of the coronary vessels, insertion of a stent (tubular spacer), coronary artery bypass grafting (providing bypass blood flow by placing a shunt on the damaged vessel).
- Anticoagulants (heparin, aspirin) to reduce blood clotting and prevent thrombosis.
The prognosis for a heart attack is always serious and depends on the volume of the affected myocardium, the localization of the necrotic focus (for example, if the conduction system of the heart is involved in the area of damage, the prognosis worsens), the patient’s age, concomitant diseases, timeliness of treatment, the presence of complications, etc. The percentage of residual effects and occurrence is high. disability.
After passing the acute period, patients are shown rehabilitation with a gradual increase in the level of stress. In the future, medical supervision and prophylactic use of antianginal drugs are necessary.
Prevention of a heart attack is the cessation of bad habits, the fight against excess weight, a balanced diet, work and rest, and timely treatment in case of angina pain.
Stages of development of transmural infarction
There are the following stages of pathology progression:
- Prodromal stage. It is accompanied by an attack of angina (myocardial ischemia, provoked by a decrease in the volume of the coronary arteries). It can last from half an hour to 30 days.
- Acute stage , which manifests itself in the form of obvious signs of an attack. It is characterized by pain, severe sweating, weakness, panic and the immediate formation of foci of necrosis. The stage begins 20 minutes after the ischemic attack, the total duration is from 4 to 6 hours). In acute transmural infarction of the lower part of the myocardial wall of the left ventricle, the pathology can occur without any pronounced symptoms. During the acute stage, the process of scar formation begins in areas affected by necrosis (from 10 to 12 days).
- Subacute stage, lasting up to 4.5 months. During this period, the manifestations of the attack gradually weaken, the heart adapts to new conditions.
- Post-infarction stage. At this stage, there are no signs of a heart attack, except in cases where complications progress.
A transmural type infarction is acute and lasts no more than 28 days from the moment of its first manifestation.
Additionally, we recommend reading the article about the stages of a heart attack.
REHABILITATION AT HOME
Using the recommendations of exercise therapy instructors, patients should regularly do a set of exercises at home. This includes morning exercises and walking. But we must not forget about self-monitoring (measure blood pressure, pulse). For hiking, it will be useful to purchase a pedometer - this way you will know the results of your training, and possibly your achievements. Do not forget about alternating loads and rest.
To quickly say goodbye to the disease, a person needs to forget that he is sick, believe in himself and his speedy and final recovery. Your loved ones should also work on this. A calm, friendly atmosphere should reign in the house. A person must feel necessary, useful, believe in his return to normal life, perhaps to his favorite job.
Some patients who suffered a heart attack belong to the 3rd and 4th functional class
. Their rehabilitation program differs from the program of the first two. Its goal is to provide the patient with such a level of activity that he can care for himself independently. Perhaps - do simple housework or work in an intellectual field (at home).
Physical rehabilitation of this group of patients takes place at home (physical therapy, massage, walks in the yard, slowly climbing a few steps up the stairs). But the patient must be visited periodically by a therapist and a cardiologist.
RECOMMENDATIONS FOR LFK
Classes at the hospital stage must be conducted by a physical therapy instructor. Although the complex for this group of patients is very gentle, the load still depends on the patient’s condition. Severe degrees require complete rest during the first week. With moderately severe patients, the instructor begins classes on the 2nd – 3rd day.
On the 4th – 5th day the patient is allowed to sit for some time on the bed with his legs dangling. From the 7th day you can take your first steps near the bed. After a couple of weeks, the doctor will allow the patient to “walk” around the ward. Go out into the hallway - from the 3rd week. With the help of an instructor, you can try to climb several steps. The number of steps and meters covered is growing every day (up to 500 - 1000 m). The patient is under the supervision of doctors or relatives, because his condition needs to be constantly assessed - by heart rate (heart rate - pulse) and blood pressure level. For reliability, these indicators are checked before the walk (half an hour) and after (half an hour).
If the treatment proceeds without complications, the patient, after an inpatient course, is sent to a cardiological sanatorium somewhere in the suburbs. There is no need for such a patient to travel long distances. There, as part of a 4-week rehabilitation course, he will receive:
- Drug treatment.
- Help from a psychotherapist.
- Diet food.
- Dosed physical activity.
Development mechanism
Approximately 9 out of 10 heart attacks progress against the background of atherosclerotic lesions of the coronary arteries. A protein-lipid tumor (atherosclerotic plaque) forms inside the wall of a large vessel through which blood flows to the heart (mainly to the coronary artery). This process develops as a result of impaired metabolism (for example, with an increased amount of cholesterol in the blood, hyperlipidemia).
Due to unstable blood pressure, the integrity of the inner wall of the vessel is compromised, while the contents of the plaque block part of its lumen, forming a barrier to full blood flow. This phenomenon is called fat embolism.
There is also another development scenario: red blood cells with platelets adhere to the damaged vessel wall, as a result of which a blood clot (thrombus) appears, which over time increases in size and blocks the lumen of the vessel.
Under such conditions, the heart muscle does not receive a sufficient volume of blood, which under normal conditions ensures its full functioning.