Who, if not pharmacists and pharmacists, should know that ethanol is a typical representative of monohydric alcohols, capable of entering into various chemical reactions. It interacts with alkali metals, magnesium, aluminum, carboxylic, inorganic acids and many other substances, including medicinal ones. According to some data, up to 25% of visits to the emergency room are associated with various adverse reactions between alcohol and drugs [1]. And it is quite natural that such widespread unfavorable events have become fertile ground for various speculations. On the eve of a series of holidays, it’s time to find answers to the most controversial questions about interactions between drugs and alcohol, as well as dispel the myths associated with it.
Thesis No. 1: Alcohol is incompatible with any antibiotics
Status: Myth
Indeed, a number of antimicrobial agents block acetaldehydrogenase, delaying the enzymatic biotransformation of ethanol at the stage of extremely toxic acetaldehyde. Its accumulation in the body contributes to the development of intoxication, which is accompanied by severe sensations. In fact, these drugs work in the same way as the famous disulfiram, used to treat alcohol addiction, which simply causes poisoning of the body. Its typical symptoms are difficulty breathing, tachycardia, nausea and vomiting, low blood pressure, fever or chills.
However, only a few antimicrobial drugs act in this way, in particular: cefamandole, cefoperazone, chloramphenicol, griseofulvin, isoniazid, metronidazole, ornidazole, nitrofurantoin and sulfamethoxazole.
All other antimicrobials do not have strict restrictions when combined with ethanol, but this does not mean that their combination helps to effectively fight infection.
Low blood pressure from a hangover
A hangover often manifests itself in the form of low blood pressure. The human body, saturated with toxic ethanol, launches a system for removing its decay products. This occurs through the sweat glands, with urination and vomiting. Dehydration occurs. As a rule, a person in this state sleeps for a long time, waking up, feeling overwhelmed and weak. Experiences unbearable thirst. This is a dangerous condition. A sharp drop in blood pressure can trigger cardiac arrest. Treating a hangover at home does not require taking serious medications. To stabilize the condition it is necessary:
- Open the windows or go outside - the brain needs oxygen.
- Replenish the lack of fluid.
- Drink Enterosgel, activated or white carbon. Take the medicine according to the instructions.
- Take a warm bath, thereby restoring blood circulation in the peripheral vessels of the extremities to normal levels.
Remember - if your condition worsens, you should urgently call emergency help.
Order alcoholism treatment
We work around the clock, experienced doctors, 100% anonymous.
Thesis No. 2: Alcohol and non-steroidal anti-inflammatory drugs are incompatible
Status: True
NSAIDs are one of the most popular painkillers. In the United States alone, this group accounts for 70 million prescriptions and 30 billion over-the-counter sales per year [2]. They are also used to relieve headaches due to alcohol intoxication. At the same time, most NSAIDs contribute to the development of gastropathy and increase the risk of gastrointestinal bleeding. Alcohol increases the severity of GI side effects of NSAIDs, increasing the risk of bleeding, which has been proven in clinical studies [3].
In addition, when acetylsalicylic acid, ibuprofen and indomethacin are taken simultaneously with ethanol, the duration of bleeding increases - an indicator that reflects the elasticity of blood vessels and their ability to contract during injury [3]. This feature further increases the risk of bleeding. Therefore, when dispensing oral and parenteral NSAIDs during the New Year holidays, it would be a good idea to remind visitors about possible drug interactions with alcohol.
What adverse events can the Sputnik V vaccine cause (GamCovidVac)
15-20% of vaccinated people experience a flu-like syndrome (headache or muscle pain, malaise) or pain at the injection site. Serious adverse events following GamCovidVac vaccination are rare. 0.001% had a severe anaphylactic reaction. This is one person per hundred thousand vaccinated.
Vaccination has been going on at GMS Clinic since January 2021; more than 5 thousand people have been vaccinated; adverse events were observed in less than 15%. More often observed: rise in body temperature, pain at the injection site, rise in blood pressure. Most of these events were not considered serious, so patients were able to successfully receive the second component of the vaccine. Once I had a severe allergic reaction. This patient was not given the second component. The symptoms went away safely, but for further vaccination this patient will most likely be recommended a different drug.
Adverse reactions usually subside within three days after vaccination. Their intensity and duration depend on various factors and indicate the reaction of the immune system. Common and harmless adverse events include:
- temperature (if it does not cause discomfort, you don’t have to take anything);
- muscle pain;
- weakness;
- headache;
- local reaction: redness and swelling at the injection site.
Adverse events such as increased body temperature or local manifestations at the injection site usually disappear after a maximum of three days. If side effects are very bothersome, you can take a non-steroidal anti-inflammatory drug (NSAID), such as paracetamol or ibuprofen. You can apply a cool compress to the injection site.
Any medicine, including vaccines, can cause allergic reactions. Not a single manufacturer, unless he is a charlatan, will forget to indicate the possibility of an allergic reaction in the instructions for use of the drug. Also, any food product, any molecule heavier than salt, can cause an allergic reaction. If you suspect an allergy, you should consult a doctor.
Thesis #3: Alcohol should be avoided during treatment with antidepressants.
Status: True
It is not recommended to combine alcohol with all antidepressants, although the mechanism of drug-ethanol-drug interaction and the severity of the consequences vary. Thus, in combination with tricyclic blood pressure medications (amitriptyline, maprotiline), ethanol can contribute to hypersedation. It disrupts the metabolism of drugs of this group in the liver, which leads to an increase in their concentration in the blood. If, in addition, the alcohol consumer has a history of alcoholic liver disease, the risks increase even more, since in this case the breakdown of antidepressants slows down and, accordingly, their level in the bloodstream increases. Increasing the dose of tricyclic antidepressants in the blood, in turn, causes cardiac arrhythmias, convulsions, hallucinations and other severe consequences, including coma [3].
The combination of selective serotonin reuptake inhibitors and alcohol is much less dangerous. Drugs in this group generally have a higher safety profile than tricyclic antidepressants and are less likely to enter into drug interactions. However, despite the absence of documented reactions between them and ethanol, their use in combination is still not recommended. This is largely due to the fact that combining SSRIs with alcohol can exacerbate the disease [4]. In addition, it has been proven that when venlafaxine is combined with ethanol, memory and cognitive abilities may decrease [4].
When to see a doctor
After vaccination, it is better to wait half an hour rather than leave immediately. This is necessary to make sure there is no allergic reaction. If it becomes difficult to breathe, there is a feeling of a strong heartbeat, tinnitus, rash, dizziness, or swelling of the face begins, you need to contact the vaccination center for medical help.
You should also consult a doctor if after vaccination:
- headache, weakness or fever does not go away within three to four days;
- high fever is not brought down by medications;
- Redness and thickening at the injection site increases on the second or third day.
Thesis No. 4: If you have a headache from drinking alcohol, it is better to take paracetamol
Status: Myth
Paracetamol is metabolized by the CYP2E enzyme to form the hepatotoxic metabolite N-acetyl-p-benzoquinone imine. Normally, it is quickly inactivated by glutathione. When consuming alcoholic beverages, especially chronically, the activity of CYP2E1 increases, which leads to increased production of a toxic metabolite. In addition, during prolonged drinking, glutathione reserves are depleted, which is associated with the accumulation of a toxic metabolite in the blood and an increased risk of developing liver failure [5].
The likelihood of drug interactions between ethanol and paracetamol also increases when taking more than 4 grams of the drug per day. The American regulator FDA recommends that those who take more than 3 alcoholic units per day (remember, an alcoholic unit is 30 ml of 40% alcohol, 100 ml of wine or 250 ml of beer) consult a doctor before taking either paracetamol or over-the-counter analgesics [ 5]. During the New Year holidays, it is important for residents of the capital to draw the attention of consumers to the increased likelihood of hepatotoxic reactions when combining paracetamol and combination drugs containing it with alcohol.
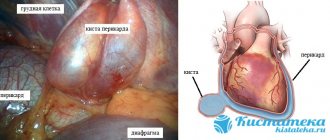
Content:
- How alcohol affects the heart
- What happens to the heart when taking high doses of alcohol?
- Screening for people with heart problems caused by alcohol
- Heart treatment for alcoholism
There is no need to believe that alcohol has a positive effect on the functioning of the cardiovascular system.
Talk about the need to drink a certain amount of vodka or good red wine every day is a banal myth. Most often they are invented by people who want to drink but have serious illnesses. Alcohol and the heart are incompatible concepts. As a result of drinking, nervous tissue is invariably damaged. Following this, ethanol attacks the heart muscle. Then the addict develops alcoholic cardiomyopathy. If left untreated, it can be fatal. Is it possible, knowing about such consequences, to talk about benefits?
Thesis No. 7: Alcohol should not be combined with certain antidiabetic drugs.
Status: True
In case of diabetes mellitus, drinking alcoholic beverages is generally extremely undesirable - this threatens a sharp drop in blood sugar levels and the development of hypoglycemia, which is associated with a violation of the release of carbohydrates stored in liver cells against the background of alcohol intoxication. The risks of hypoglycemia in diabetic patients who drink alcohol are further increased due to possible drug interactions between ethanol and some sulfonylureas, in particular glipizide [3].
Combining alcoholic beverages with the first-line drug for the treatment of type 2 diabetes mellitus, metformin, can lead to increased levels of lactic acid in the blood and the development of lactic acidosis. The likelihood of its occurrence increases with a low-calorie diet, poor nutrition and liver failure. Therefore, metformin is incompatible with alcohol in both alcoholic beverages and alcohol-containing medications [3].
Insulin also interacts with ethanol. Alcohol can enhance or weaken the hypoglycemic effect of the drug, which can lead to the development of hypo- or hyperglycemia and, accordingly, worsening disease control [7].
Antihypertensive drugs and alcohol - compatibility of substances, consequences of use
Currently, hypertension is a very common disease. And treatment of hypertension involves long-term use of antihypertensive drugs. Of course, taking pills coincides with holidays and celebrations. And therefore, people have a natural question: is it possible to take antihypertensive drugs with alcohol?
Classification of antihypertensive drugs
The development of arterial hypertension is indicated when systolic blood pressure rises above 140 mmHg. High blood pressure leads to impaired blood supply to internal organs, especially the brain and heart. And this, in turn, is fraught with the development of such dangerous conditions as stroke and subarachnoid hemorrhage.
Antihypertensive drugs are prescribed to treat hypertension. These are different groups of drugs that lower blood pressure through various mechanisms of action. Thus, the following groups of antihypertensive drugs are distinguished:
- ACE inhibitors (Enalapril, Captopril);
- Diuretics (Hydrochlorothiazide, Furosemide);
- Angiotensin II receptor blockers (Losartan, Valsartan);
- Beta-blockers (Atenolol, Labetalol);
- Calcium antagonists (Verapamil, Amlodipine);
- Combination drugs (Captopres, Liprazide).
If arterial hypertension is detected, treatment begins with the administration of one drug in a minimum dosage; if necessary, the dose is gradually increased. When such a treatment regimen does not have the desired effect, then a combination of several antihypertensive drugs from different groups is prescribed.
Compatibility of blood pressure pills with alcohol
When prescribing antihypertensive drugs, doctors warn their patients against drinking alcoholic beverages. This limitation is due to the fact that alcohol enhances the hypotensive effect of the drug. It would seem that lowering blood pressure is a good thing? However, the use of antihypertensive drugs with alcohol leads to a sharp and severe decrease in blood pressure, and this is another undesirable extreme.
It is important to understand that a critical drop in pressure leads to disruption of the blood supply to internal organs, which means oxygen starvation of tissues develops. The brain is the first to suffer from a lack of oxygen.
Signs indicating the development of acute arterial hypotension are:
- Severe weakness;
- Cold extremities;
- Pale skin;
- Headache;
- Dizziness;
- Fainting.
The use of antihypertensive drugs with alcoholic beverages is especially dangerous for people suffering from coronary heart disease or vascular diseases of the brain . In such patients, a sudden and excessive decrease in blood pressure can lead to myocardial infarction or stroke.
What happens if you take alcohol with blood pressure pills?
So, alcohol enhances the hypotensive effect of antihypertensive drugs, which is fraught with serious consequences. Therefore, antihypertensive drugs should not be taken with alcoholic beverages. What to do in such a situation if an important celebration is coming up? First of all, you should never stop taking medications completely, as this can ultimately lead to a hypertensive crisis. It is worth consulting with your doctor on this issue; sometimes, as an exception, when treating arterial hypertension, drinking alcohol in small quantities is allowed.
Separately, it is worth mentioning the use of antihypertensive drugs for hangovers. Often, after a wild party, people wake up the next morning with high blood pressure. This is an extremely dangerous condition that can lead to hypertensive crisis or stroke. In such situations, it is imperative to reduce blood pressure with the help of antihypertensive drugs, despite the fact that a small amount of alcohol still remains in the blood.
Valeria Grigorova, doctor, medical columnist
2, total, today
Thesis No. 8: If you have a hangover, you can take regular “cold powders”
Status: Myth
Anti-cold combination drugs contain several components, and at least two of them can interact with ethanol. Firstly, most drugs in this group contain paracetamol, sometimes in a dose of 1000 g. When it is combined with alcohol, the risk of hepatotoxic reactions increases. Secondly, many anti-cold combination drugs contain 1st generation antihistamine components. Alcohol can potentiate their depressant effect on the central nervous system, promoting the development of hypersedation and drowsiness [3]. Therefore, drugs from this group should not be recommended as remedies to relieve hangover symptoms.
Sources
- Alcohol-medication interactions. Alberta Health Services. – [Electronic resource] – URL: https://www.albertahealthservices.ca/assets/healthinfo/AddictionsSubstanceAbuse/hi-asa-beyond-abcs-a... (Access date 12/09/2019).
- Alcohol-medication interactions. Alberta Health Services. – [Electronic resource] – URL: https://www.albertahealthservices.ca/assets/healthinfo/AddictionsSubstanceAbuse/hi-asa-beyond-abcs-a... (Access date 12/09/2019).
- Green GA Understanding NSAIDs: from aspirin to COX-2 //Clinical cornerstone. 2001; 3 (5): 50–59.
- Weathermon R., Crabb DW Alcohol and medication interactions //Alcohol research. 1999; 23 (1): 40.
- Adams WL Interactions between alcohol and other drugs //International journal of the addictions. 1995; 30 (13–14): 1903–1923.
- Noureldin M. et al. Drug-alcohol interactions: a review of three therapeutic classes //US Pharm. 2010; 35 (11): 29–40.
- Moore AA, Whiteman EJ, Ward KT Risks of combined alcohol/medication use in older adults //The American journal of geriatric pharmacotherapy. 2007; 5 (1): 64–74.
- According to GRLS data as of December 12, 2019.