Many people have heard about the features and terrible consequences of myocardial infarction, including death, and most of us have had relatives or friends suffer from this disease. Speaking about the attack itself, the mind immediately associates with its main symptoms: pain in the chest (stabbing, burning, aching, cutting nature), which radiates to the shoulder or under the shoulder blade, shortness of breath, rapid heartbeat, dizziness, profuse sweating, loss of consciousness.
But as it turned out, doctors repeatedly record cases where these characteristic symptoms do not appear and a person, without realizing it, suffers a heart attack on his legs.
This phenomenon is also called an atypical form of the disease. As a rule, it is revealed that the patient suffered a heart attack on his legs - randomly, for example, in a cardiogram during an annual medical examination.
Sign up for a consultation
Mechanism of development of acute coronary syndrome
Myocardial infarction, which, along with an episode of unstable angina, is included in the concept of acute coronary syndrome, is an exacerbation of coronary heart disease. During myocardial infarction, necrosis of the heart muscle develops due to acute disruption of the blood supply. In most cases, this occurs as a result of atherothrombosis, in which the coronary vessels are partially or completely blocked by a blood clot. The disease is manifested by sudden intense pain in the chest, tachycardia, “cold sweat”, pallor of the skin and a number of other symptoms.
The goal of treating an acute heart attack is to quickly restore blood supply. However, even after blood flow is established, therapy cannot be stopped, since coronary atherosclerosis, which became the foundation for the development of acute coronary syndrome, is chronic.
Treatment of myocardial infarction
Myocardial infarction
- an emergency disease in cardiology and serves as an indication for immediate hospitalization in intensive care.
The number one task for doctors is to restore blood flow
in a thrombosed vessel. They achieve this in different ways. The priority and most effective is surgical intervention - angioplasty with stenting of the affected area of the artery or coronary artery bypass grafting. In parallel, medications are used that inhibit the development of a blood clot - disaggregants (aspirin, clopidogrel) and anticoagulants (heparin), and if immediate surgery is not possible, thrombolytics - drugs that dissolve the blood clot (alteplase, prourokinase).
Pain relief
carried out with narcotic analgesics, neuroleptics, intravenous infusions of nitroglycerin.
The size of the necrosis zone can be reduced by reducing myocardial oxygen consumption by using beta-blockers (metoprolol, bisoprolol, atenolol), ACE inhibitors (enalapril, lisinopril, ramipril), and oxygen therapy.
For arrhythmias
antiarrhythmics are used (magnesium, lidocaine, amiodarone), atropine for bradycardia. Anxiolytics and sedatives are prescribed to ensure psycho-emotional peace of the patient.
Strict bed rest
in the early stages of treatment and fractional meals, limited in volume and calorie content.
Early consequences of myocardial infarction1
Starting from the first hours after a heart attack and up to 3-4 days, early consequences of a heart attack may develop, including:
- acute left ventricular failure, which occurs when the contractility of the heart decreases. When it occurs, shortness of breath, tachycardia, and cough appear;
- cardiogenic shock. This is a severe complication of acute coronary syndrome, developing as a result of a significant deterioration in the contractility of the heart muscle due to extensive necrosis;
- disturbances of cardiac rhythm and conduction are observed in 90% of patients with acute MI.
- Attacks of early post-infarction angina (PSA). PSC is the occurrence or increase in frequency of angina attacks 24 hours and up to 8 weeks after the development of MI.
- pericarditis is an inflammatory process that develops in the outer lining of the heart, the pericardium. It occurs in the first or third day of the disease and can manifest itself as pain in the heart area, which changes with a change in body position, and an increase in body temperature.
In 15-20% of heart attack cases, thinning and bulging of the heart wall occurs, most often of the left ventricle. This condition is called cardiac aneurysm. As a rule, it develops with extensive damage to the heart muscle. Factors predisposing to the development of cardiac aneurysm also include violation of the regime from the first days of the disease, concomitant arterial hypertension and some others.
A special group consists of thromboembolic consequences, in which the lumen of the vessels is completely or partially blocked by blood clots. This often occurs against the background of concomitant varicose veins, blood coagulation disorders and prolonged bed rest.
Due to impaired blood supply, acute coronary syndrome can be complicated by gastrointestinal problems, such as erosions and acute ulcers of the gastrointestinal tract. Mental disorders may also occur - depression, psychosis. They are facilitated by old age and concomitant diseases of the nervous system.
Types and symptoms of their manifestation
There are six types of atypical forms of the disease:
- arrhythmic;
- asthmatic;
- abdominal;
- collaptoid;
- erased;
- cerebral.
Each of these varieties manifests itself differently, and the symptoms of the attack often do not even resemble such a serious disease, which results in a heart attack on the legs.
In the event of an arrhythmic attack, a disturbance in the rhythm of the heartbeat occurs, and cases of cardiac arrest are common.
The asthmatic form is manifested by a strong attack of coughing, reaching the point of suffocation, and no pain in the cardiac region (or radiating under the shoulder blade) is observed.
An abdominal attack is characterized by sharp pain in the abdomen, which intensifies with slight pressure on the pancreas. Very often the attack is accompanied by bloating, as well as nausea and vomiting.
A collaptoid attack is characterized by a sharp decrease in blood pressure, accompanied by dizziness and often fainting.
The most asymptomatic type is the erased type (the most common case of a heart attack on the legs). In this case, there is only mild weakness or sweating, and less often – discomfort in the chest (in the form of mild pain of an undetermined nature).
call me back
The cerebral variety is distinguished by symptoms characteristic of cerebrovascular accident: speech becomes slurred, nausea and vomiting appear, some clouding of consciousness appears, and weakness in the limbs.
Considering the obvious insidiousness of the disease, it should be treated with great caution, avoiding the consequences that a heart attack on the legs may bring; any symptoms - characteristic or uncharacteristic (characteristic of the atypical form) - should be a signal to consult a doctor.
Important! Every 5th of those who suffered a heart attack does not know about it, and in every 4th patient this disease is not recognized.
Late consequences of a heart attack
At the end of the acute period of the disease, so-called late consequences may develop. These include complications that appear 10 days after the manifestation of MI and later:
- post-infarction Dressler syndrome occurs 2-6 weeks after the manifestation of myocardial infarction and is manifested by inflammation of the pericardium, pleura, alveoli, joints and other pathological changes;
- thromboendocarditis with thromboembolic syndrome (the appearance of a wall thrombus in the heart cavity, on the heart valves);
- late post-infarction angina, which is characterized by the occurrence or increase in frequency of angina attacks. Its frequency ranges from 20 to 60%.
Some patients who have suffered an acute myocardial infarction are at high risk for developing repeated complications of coronary heart disease and, above all, recurrent myocardial infarction and unstable angina. This is due to the fact that in patients with acute coronary syndrome, along with the presence of an atherosclerotic plaque, which was complicated by a rupture and blocked the lumen of the coronary artery, there are plaques in other arteries. They can be the cause of repeated episodes of cardiovascular events, the probability of which is very high.
Prevention of myocardial infarction
Prevention of coronary artery disease and its extreme expression - myocardial infarction - comes down to influencing modifiable risk factors, namely: physical activity, nutrition, body weight, bad habits, blood glucose and cholesterol levels, blood pressure.
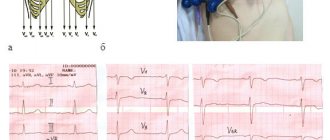
After a heart attack, it is important to regularly independently measure blood pressure and heart rate, systematically undergo ECG and EchoCG diagnostics, and take daily medications to prevent the progression of heart dysfunction and recurrence of the disease.
Stages of treatment and rehabilitation
| Period | Treatment methods | Features of care |
| Rehabilitation (up to 28 days) | The patient is transferred to the infarction department and then to a cardiology sanatorium. The patient is prescribed medications that normalize blood circulation and strengthen the heart muscle. | The nurse teaches the ward how to sit down and stand up correctly and helps restore self-care skills. |
| Rehabilitation (up to 28 days) | The patient is transferred to the infarction department and then to a cardiology sanatorium. The patient is prescribed medications that normalize blood circulation and strengthen the heart muscle. | The nurse teaches the ward how to sit down and stand up correctly and helps restore self-care skills. |
| Outpatient (up to 1 year) | The patient is seen by a doctor in a clinic or boarding house, takes medications to prevent a heart attack, and does physical therapy. | The caregiver’s task is to help the recovering person adjust his diet and daily routine to avoid a relapse. |
Rehabilitation of patients who have suffered an acute myocardial infarction affects all aspects of the patient's life. In addition to medication and physiotherapeutic treatment, it includes moderate physical activity and work with emotions.
Specifics of care in the acute period
This is the most important step in the treatment of myocardial infarction. Any physical activity, anxiety, or skipping medications can lead to irreversible consequences. Since the patient after a myocardial infarction must strictly adhere to bed rest, he finds himself completely helpless and needs round-the-clock care.
The nurse should:
- feed him and give him medicine on time,
- periodically measure blood pressure and pulse,
- maintain body hygiene,
- change underwear and bed linen,
- turn over several times a day to prevent bedsores and thrombosis,
- provide psychological support.
A patient with myocardial infarction is prescribed diet No. 10. It does not contain products that cause gas and limits salt intake. The patient receives food in small portions 5-6 times a day. The last dose should be at least 3 hours before bedtime.
To prevent diaper rash from occurring on the skin, the patient should be dressed in light but warm clothing that allows air to pass through and removes moisture from the body.
In the acute period, many patients are characterized by a strong fear of death, a hypochondriacal or hysterical reaction, which negatively affects health and prevents the body from recovering. If these conditions are not corrected in a timely manner, changes in the psyche can become entrenched in character. The nurse helps the patient cope with the fear of death, focuses his attention on improvements and positive prognoses, monitors the adequacy of reactions and immediately informs the doctor if the patient shows signs of psychosis.
Rehabilitation conditions for patients who have suffered a myocardial infarction
Bed rest in the acute period is due to the need to reduce the load on the heart muscle and reduce its need for oxygen. However, prolonged refusal to move increases the risk of congestion in the lungs and the formation of blood clots, impairs the functioning of the digestive system, and causes muscle weakness. To avoid this, the patient is given moderate physical activity as he recovers.
If the acute period passes without complications, the patient is allowed to sit down, stand up, and go to the toilet independently. The nurse helps perform movements smoothly, without sudden effort, and makes sure that the patient does not become ill. It measures your heart rate before and after physical activity. After about 2 weeks, short walks around the hospital grounds are allowed.
The transition from one activity level to the next is permitted after an intermediate diagnosis. The patient's blood pressure is measured, a cardiogram is taken, and individual exercise tolerance is checked. Light exercise should be done in bed before getting up to prepare the cardiovascular system after sleep for daytime activity.
After discharge from the hospital, the patient is recommended to undergo rehabilitation in a sanatorium or boarding house. Here a therapeutic diet is prepared for him, rich in potassium and maintaining a balance of proteins, fats, and carbohydrates. Benefits for the patient:
- lean meat,
- fish,
- fresh vegetables and fruits,
- whole grain cereals,
- eggs,
- greenery,
- cottage cheese,
- potato.
Upon admission to the rehabilitation department, the patient takes exercise tests. The results show the functioning of the cardiovascular and respiratory systems. Based on them, a system of exercises is developed in a gentle or training mode. The patient is recommended to engage in physical therapy 3-4 times a day with a gradual increase in load. The exercise therapy complex may include:
- general strengthening workout,
- balance exercises,
- exercises with ball and stick,
- walking at a calm and fast pace,
- swimming,
- exercise classes,
- breathing exercises.
The duration of classes is 10-25 minutes. At the rehabilitation stage, patients who have suffered a myocardial infarction no longer require physical care, but still need psychological support. Many of them do not adequately assess their capabilities and either avoid the required load or increase it excessively. The nurse’s task during this period is to monitor compliance with the recommended schedule of activities and rest, work with the negative emotions of the ward and help him adapt to normal life.
Where to go and what to do if symptoms appear
If the above symptoms appear, you should immediately call an ambulance, which will provide the necessary assistance and take the patient to a specialized clinic for further diagnosis and treatment. Before the doctors arrive, it is better for the patient to lie down and provide access to oxygen - unfasten the collar, open the window. For medications you need to take acetylsalicylic acid tablet. Nitroglycerin is recommended if a person has taken it previously, as the drug can sharply lower blood pressure.
In any case, if you have complaints from the cardiovascular system, you should contact a therapist or cardiologist. The clinic will conduct instrumental and laboratory tests: ECG, general clinical and biochemical blood tests, troponin tests, and angiography if necessary. The doctor will be able to assess the functioning of the heart, the presence of its pathologies, and also identify concomitant diseases and risk factors.
A microinfarction is easier to prevent than to cure. To do this, it is advisable to regularly visit your therapist and follow his instructions. The doctor can give recommendations on a healthy lifestyle, diet and exercise, and prescribe the necessary medications. To prevent blood clots, acetylsalicylic acid (Cardiomagnyl) drugs are often prescribed, which thin the blood and reduce the risk of myocardial infarction.
“You are cured, you can live as before”
This is a very common misconception among patients who were quickly put on their feet by doctors and did not realize how serious their illness was. “Now we can cure a person who has suffered such a deadly disease, so that he returns to work, lives an active life and does not feel sick,” explains Professor, Corresponding Member of the Russian Academy of Sciences Simon Matskeplishvili. “And here lies a great danger.” Because, having once suffered a heart attack, the patient often runs the risk of having another one if he behaves incorrectly.” The risk of a repeat disaster is from 10 to 20% in the first year.
How to reduce this risk? Continuity of treatment is extremely important. “A patient with a heart attack no longer spends a month in the hospital as before. He is discharged after a few days, feels fine and does not consider it necessary to follow our recommendations for continuing therapy,” says Professor Matskeplishvili. “It is especially difficult to convince that medications need to be taken long-term, often, for life.”
Features of rehabilitation
The most acute period usually lasts up to six hours from the moment of the attack, the acute period - up to seven days. Scarring takes 28 days. Rehabilitation after a heart attack takes place in several stages, requiring the patient to give up bad habits and review all the main aspects of life:
- lifestyle;
- physical activity;
- diet.
The psychological attitude is of great importance. The duration of rehabilitation at the inpatient and outpatient stages depends on the patient’s condition. The final stage has no deadline - it lasts a lifetime.
Factors influencing the development of heart attack
A heart attack is a multifactorial pathology, that is, it is caused by the action of many causes at once. There are also risk factors that are likely to increase the incidence. These factors need to be known in order to eliminate and thereby reduce the risk of developing a heart attack or, if it has already developed, a second attack.
It is impossible to suffer a heart attack on your legs; strict bed rest is necessary
Risk factors are:
- atherosclerotic changes in blood vessels - a cholesterol plaque in atherosclerosis can increase, blocking the lumen of the vessel so much that the tissue starves, first under load conditions, and over time at rest. It can also break off and cause an embolism;
- thromboembolism - dense blood clots can break off, enter the systemic circulation, and then clog the coronary vessels. An embolus can be fat, a foreign body, or an air bubble;
- high blood pressure – contributes to damage to the vascular wall;
- poor nutrition – abuse of foods high in trans fats and cholesterol;
- excess body weight;
- smoking and alcohol abuse;
- sedentary lifestyle;
- congenital deformation of the vessel wall.
Clinical manifestations in men are more pronounced, manifest earlier and persist longer; in women they are weaker, often completely absent; a heart attack is more easily tolerated, but this complicates its diagnosis.
Based on this list, disease prevention is built. For example, if an increased content of lipids (fats) is detected in the blood, then the menu should be adjusted. The same should be done for patients who are overweight. It is important to quit smoking and minimize alcohol intake. There should be no restriction on physical activity - refusal of heavy, exhausting work should not exclude walks in the fresh air and moderate physical activity. Patients at risk should carefully monitor their blood pressure and overall health.