Plasma transfusion
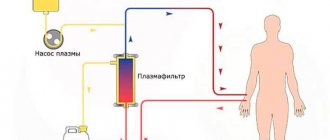
The plasmapheresis procedure can be performed by two main methods: discrete and hardware. As a result, doctors can prepare several types of plasma for subsequent transfusion:
- Native plasma
, which is isolated from donor canned blood. Thus, from 500 ml of preserved blood, 250–300 ml of native plasma are obtained. - Plasma obtained by automatic plasmapheresis
using a special installation.
For transfusion, fresh frozen plasma of the same blood group is used. Initially, doctors adhere to a dosage of 10–20 ml/kg. The decision on subsequent transfusions is made based on the patient’s clinical condition and the results of blood coagulation studies. However, do not underestimate the importance of blood plasma.
Plasma transfusion - indications and contraindications
Like any medical procedure, plasma transfusion has its indications and contraindications. Doctors always take them into account before prescribing a transfusion of hemostatic solutions. Among the situations when a blood plasma transfusion may be required, the indications include the following:
- Replenishment of the volume of plasma hemostasis factors in DIC complicated by the development of shock.
- Replenishing the volume of plasma hemostasis factors in acute massive blood loss.
- Reduced synthesis of plasma coagulation factors caused by liver diseases.
- Overdose of direct anticoagulants.
- Plasmapheresis for thrombocytopenic purpura, severe poisoning, sepsis.
- Coagulopathy caused by a deficiency of plasma physiological anticoagulants.
Plasmapheresis is not recommended:
- as a replenishment of blood volume;
- for parenteral nutrition;
- persons with a burdened transfusion history;
- with congestive heart failure.
Blood plasma transfusion - side effects
When prescribing such a procedure, doctors know the dangers of plasma transfusion, so they take appropriate measures to prevent complications. Among the common transfusion complications it is necessary to highlight:
- febrile non-hemolytic reactions;
- acute hemolytic reaction caused by AB0 incompatibility;
- overload of the circulatory system;
- allergic reactions;
- post-transfusion purpura;
- infections.
How to get plasma?
Plasma is obtained from the blood using centrifugation. The method allows you to separate plasma from cellular elements using a special apparatus without damaging them . The blood cells are returned to the donor.
The plasma donation procedure has a number of advantages over simple blood donation:
- The volume of blood loss is less, which means less harm is caused to health.
- Blood can be donated for plasma again after 2 weeks.
There are restrictions on plasma donation. Thus, a donor can donate plasma no more than 12 times per year.
Plasma donation takes no more than 40 minutes.
Plasma is the source of such important material as blood serum. Serum is the same plasma, but without fibrinogen, but with the same set of antibodies. They are the ones who fight pathogens of various diseases. Immunoglobulins contribute to the rapid development of passive immunity.
To obtain blood serum, sterile blood is placed in an incubator for 1 hour. Next, the resulting blood clot is peeled off the walls of the test tube and placed in the refrigerator for 24 hours. The resulting liquid is added to a sterile vessel using a Pasteur pipette.
Blood plasma: composition and functions
Blood plasma is a viscous, homogeneous liquid of light yellow color. It makes up about 55-60% of the total blood volume. It contains blood cells in the form of a suspension. Plasma is usually clear, but may be slightly cloudy after eating a fatty meal. Consists of water and mineral and organic elements dissolved in it.
Plasma composition and functions of its elements
Most of the plasma is water, its amount is approximately 92% of the total volume. In addition to water, it includes the following substances:
- proteins;
- glucose;
- amino acids;
- fat and fat-like substances;
- hormones;
- enzymes;
- minerals (chlorine, sodium ions).
About 8% of the volume is proteins, which are the main part of plasma. It contains several types of proteins, the main ones being:
- albumins – 4-5%;
- globulins – about 3%;
- fibrinogen (belongs to globulins) – about 0.4%.
Other proteins
In addition to the above, plasma also contains other proteins:
- complement (immune proteins);
- transferrin;
- thyroxine-binding globulin;
- prothrombin;
- C-reactive protein;
- haptoglobin.
You can also read: Total protein in the blood
Non-protein components
In addition, blood plasma includes non-protein substances:
- organic nitrogen-containing: amino acid nitrogen, urea nitrogen, low molecular weight peptides, creatine, creatinine, indican. Bilirubin;
- organic nitrogen-free: carbohydrates, lipids, glucose, lactate, cholesterol, ketones, pyruvic acid, minerals;
- inorganic: sodium, calcium, magnesium, potassium cations, chlorine anions, iodine.
The ions in the plasma regulate the pH balance and maintain the normal state of cells.
Functions of proteins
Proteins have several purposes:
- homeostasis;
- ensuring the stability of the immune system;
- maintaining the aggregate state of the blood;
- nutrient transfer;
- participation in the process of blood clotting.
Plasma functions
Blood plasma performs many functions, including:
- transportation of blood cells, nutrients, metabolic products;
- binding of liquid media located outside the circulatory system;
- making contact with body tissues through extravascular fluids, thereby achieving hemostasis.
Donor plasma saves many lives
Use of donor plasma
In our time, transfusions often require not whole blood, but its components and plasma. Therefore, blood transfusion centers often donate blood for plasma.
It is obtained from whole blood by centrifugation, that is, the liquid part is separated from the formed elements using a machine, after which the blood cells are returned to the donor. The procedure lasts about 40 minutes.
The difference from donating whole blood is that blood loss is much less, and you can donate plasma again after two weeks, but no more than 12 times during the year.
To obtain it, place sterile blood in a thermostat for an hour. Then the resulting clot is peeled off from the wall of the test tube and kept in the refrigerator for a day.
After this, using a Pasteur pipette, the settled whey is poured into a sterile container.
Conclusion
Blood plasma is its liquid component, which has a very complex composition. Plasma performs important functions in the body.
In addition, donor plasma is used for transfusion and preparation of therapeutic serum, which is used for the prevention and treatment of infections, as well as for diagnostic purposes to identify microorganisms obtained during analysis. It is considered more effective than vaccines.
Immunoglobulins contained in serum immediately neutralize harmful microorganisms and their metabolic products, and passive immunity is formed faster.
Composition and objectives of non-protein compounds in plasma
Plasma contains:
- Organic compounds based on nitrogen. Representatives: uric acid, bilirubin, creatine. An increase in the amount of nitrogen signals the development of azotomy. This condition occurs due to problems with the excretion of metabolic products in the urine or due to the active destruction of protein and the entry of large amounts of nitrogenous substances into the body. The latter case is typical for diabetes, fasting, and burns.
- Organic compounds that do not contain nitrogen. This includes cholesterol, glucose, lactic acid. Lipids also keep them company. All these components must be monitored, as they are necessary to maintain full functioning.
- Inorganic substances (Ca, Mg). Na and Cl ions are responsible for maintaining a constant pH of the blood. They also monitor osmotic pressure. Ca ions take part in muscle contraction and stimulate the sensitivity of nerve cells.
Blood plasma composition
Albumen
Albumin in plasma blood is the main component (more than 50%). It has a small molecular weight. The place of formation of this protein is the liver.
Purpose of albumin:
- Transports fatty acids, bilirubin, drugs, hormones.
- Takes part in metabolism and protein formation.
- Reserves amino acids.
- Forms oncotic pressure.
Doctors judge the condition of the liver by the amount of albumin. If the albumin content in plasma is reduced, this indicates the development of pathology. Low levels of this plasma protein in children increase the risk of developing jaundice.
Globulins
Globulins are represented by large molecular compounds. They are produced by the liver, spleen, and thymus.
There are several types of globulins:
- α – globulins. They interact with thyroxine and bilirubin, binding them. Catalyze the formation of proteins. Responsible for transporting hormones, vitamins, lipids.
- β – globulins. These proteins bind vitamins, Fe, and cholesterol. They transport Fe and Zn cations, steroid hormones, sterols, and phospholipids.
- γ – globulins. Antibodies or immunoglobulins bind histamine and take part in protective immune reactions. They are produced by the liver, lymph tissue, bone marrow and spleen.
There are 5 classes of γ-globulins:
- IgG (about 80% of all antibodies). It is characterized by high avidity (antibody to antigen ratio). Can penetrate the placental barrier.
- IgM is the first immunoglobulin that is formed in the unborn baby. The protein has high avidity. It is the first to be detected in the blood after vaccination.
- IgA.
- IgD.
- IgE.
Fibrinogen is a soluble plasma protein. It is synthesized by the liver. Under the influence of thrombin, the protein is converted into fibrin, an insoluble form of fibrinogen. Thanks to fibrin, a blood clot forms in places where the integrity of the vessels has been compromised.
Other proteins and functions
Minor fractions of plasma proteins after globulins and albumins:
- Prothrombin,
- Transferrin,
- immune proteins,
- C-reactive protein,
- Thyroxine binding globulin,
- Haptoglobin.
The tasks of these and other plasma proteins boil down to:
- Maintaining homeostasis and aggregative state of blood,
- Controlling immune reactions
- Transport of nutrients
- Activation of the blood clotting process.
Harmful or useful
There are different, often directly opposite, opinions about whether donating blood plasma is harmful. Some are convinced that such an activity definitely harms our body and strongly advise against resorting to it. Others, on the contrary, believe that donating it brings benefits to the donor. Modern medical scientists have convincingly proven that such a procedure poses absolutely no threat to the health of the person donating plasma, being completely harmless. Moreover, after donating plasma, the work of protective functions and immunity is activated, so experienced doctors often prescribe plasma donation to patients as a medicinal and health-improving procedure.
Preparation and process
Plasma donation requires mandatory compliance with a number of rules and requirements. Anyone who wants to take it must know that there are strict restrictions and even prohibitions in this process. For example, plasma cannot be taken from a person if he is sick:
- AIDS;
- Syphilis;
- Hepatitis;
- Suffering from alcoholism or drug addiction, mental or other illnesses.
The center where blood transfusions are also not allowed to do this in case of problems with diabetes mellitus, abnormal blood pressure, or signs of severe myopia. Temporary restrictions apply to those who have recently undergone tooth extraction, surgery or vaccination, during the menstrual process, are homosexual, illegal migrants, etc. These and other norms have determined in practice a special algorithm for the admission procedure. First, a potential donor's blood must be taken for analysis to determine whether there are any viruses in it and how much hemoglobin it contains. The patient is required to honestly fill out the questionnaire, and only after that he can be admitted to the procedure. Before this, he should avoid taking:
- Salty, spicy and fatty foods;
- Any medications;
- Alcohol (at least a week before the test day).
After plasma collection, which can be either automatic or manual, the patient is usually required to stay in the blood collection center hospital for another two hours. Good health to you!
Blood functions
How many liters of blood a person has is determined in accordance with his individual characteristics and the functions performed by the fluid. Blood constantly moves through the system, which includes large and small vessels. They supply fluid to all organs and tissues in the human body.
Red cells deliver oxygen to tissues as hemoglobin binds to its molecules. Platelets are involved in the coagulation process during bleeding. With their help, a blood clot is formed at the site of injury. Thanks to leukocytes, protection is provided from the effects of negative external and internal factors.
Fibrinogen
Acts as a special protein. It is produced in the liver. The main task is to ensure normal blood clotting. The process takes place in several stages.
- As soon as the body needs to close a wound, a gap in the tissues, the synthesis of special substances-factors begins. These include fibrinogen.
- Once the amount of a substance reaches a certain value, it is subject to breakdown. A special compound called thrombin is involved.
- Fibrinogen is destroyed and breaks down into sticky components. The so-called threads.
- After the factor has precipitated, it adheres to the site of the lesion, platelets, ensuring normal coagulation. A blood clot forms and covers the wound surface. It then forms a hard scab.
The process occurs whenever a lesion is formed. If there is not enough fibrinogen, coagulopathies begin. Normal clotting is disrupted. The blood becomes too thin.
Amino acids
They act as a kind of building material for the cells of the body. They are also part of their walls, ensuring normal conductivity of the cytoplasmic membrane. And at the same time its strength and elasticity.
- Fats. Lipids, like amino acids, are the main building materials. The key one is cholesterol, which is well known to everyone.
- Glucose. Acts as a nutrient. Works as a special stock. Because during splitting a large amount of energy is released. As a rule, during the production of donor material, glucose is not removed; it remains in place.
- Hormones. Those that are produced in the patient's body. They act as a kind of mediators, substances that transmit signals to tissues and entire systems. This is their main task.
- Minerals. Iodine, iron, chlorine, dozens of other substances. Both in the form of a complete compound that does not enter into simple reactions, and in the form of charged ions. It is the latter that maintain normal blood acidity and participate in the functioning of cells and cytoplasmic membranes.
All substances perform two main functions. If we talk about the issue in general.
Which ones exactly:
- Ensuring proper metabolism.
- Maintaining a state of homeostasis. When the body is in balance, works correctly and is stable in relation to itself.
A deficiency or excess of any compound immediately results in disorders. In this case, treatment is required.
Albumen
The compound is synthesized in the liver. If we talk about concentration, then protein accounts for up to 50% of the total amount of substances in plasma.
Albumin performs several important functions:
- Transportation. Transferring connections from place to place. If compared with the liquid fraction itself, the mechanism here will be somewhat different. Albumin binds substances, personally participating in transfer. This is not a purely mechanical action.
Thanks to this ability, it can transport drugs, hormones and all important compounds, chemically active structures.
- Metabolism. Without albumin there can be no normal metabolism. Including energy.
- Regulation of local pressure. We are talking about an indicator in which foreign substances freely pass into the cells. If there is not enough protein, disruptions in the functioning of the entire body begin. Since albumin regulates both metabolism and local pressure at the molecular level. All deviations become noticeable immediately.
- Protein synthesis. Albumin in some cases acts as a building material. When it is processed, other substances are formed. The process is constant and proceeds almost without interruption.
- Preservation of amino acids. Reservation. In this situation, albumin acts as a kind of bank. For the time being, until amino acids are needed.
Albumin is one of the most important proteins in liquid connective tissue. It works both as transport and as a storehouse of important substances. And in some cases it performs tasks related to the synthesis of other chemical molecular structures.
Blood cells - structure and functions
Each of the variants of biological fluid components is designed for specific tasks. All types of blood cells interact and come from identical “progenitors,” but their functions are different, as is their structure. These characteristics are also important when testing biological fluids, because any violations of the parameters indicate pathological conditions in the body.
Red blood cells - structure and functions
Red blood cells are “containers” of hemoglobin. This is a special pigmented protein that gives biological fluid a rich color.
It is important to study what red blood cells look like and what they are made of; their structure and functions are closely related. Hemoglobin, the filler of red cells, simply includes 2 parts: heme - a core with iron atoms, and globin - a protein helix
Externally, red blood cells resemble a flat biconcave cake. This form provides the ability to effectively capture oxygen in the alveoli of the lungs and transport it. The cells are very small (up to 10 microns) and elastic, due to which they move easily even in the thinnest vessels and capillaries. Red blood cells are highly specialized and perform the following functions:
- respiratory;
- nutrient transfer;
- adsorption of toxins;
- blood clotting (indirect);
- storage of antigens.
Leukocytes - structure and functions
White blood cells are classified into two large groups - agranulocytes (non-granular) and granulocytes (granular). They differ in the structure of their nuclei, the tasks they perform, and their ability to interact with foreign microorganisms and organelles. The first type is divided into monocytes and lymphocytes. The second group includes the following types of leukocytes:
- neutrophilic;
- basophilic;
- eosinophilic.
Simplified structure of leukocytes - nucleus, body and pseudopods. The cell visually resembles a ball of lint. The pseudopods provide the leukocyte with maximum mobility, the ability to penetrate any membrane and overcome vascular walls. This is necessary to perform leukocyte functions:
- protection against infections, foreign bodies, foreign protein structures;
- provocation of inflammation;
- ensuring the functioning of the immune system;
- regulation of allergic reactions;
- response to parasitic infestations;
- destruction of cancer cells.
Platelets - structure and functions
These blood cells have unique properties
As with red blood cells, it is important to consider what platelets contain; their structure and functions also depend on each other. Cells do not have a nucleus, but a large number of granules are present
When a platelet is activated against the background of damage, it changes its spherical shape and flattens, turning into a plate with processes. The number of such “branches” reaches 10 pieces, their length can exceed the diameter of the cell by 5-10 times. Thanks to the processes, platelets attach to the “hole” site and to each other, forming a plug necessary for healing.
The structure of the described elements is schematic:
- Glycocalyx.
Layer above the membrane with an open system of tubules. The glycocalyx triggers the platelet flattening mechanism and its activation. - Membrane.
Contains lysosomes that interact with blood clotting factors. - Matrix or gel zone.
It contains mitochondria that secrete specific granules. - Organelles.
This area is a collection of different granules responsible for the blood clotting process.
https://youtube.com/watch?v=iDc5eRa1ias%250D
Functions and tasks of plasma
Why does the human body need plasma?
Its functions are varied, but basically they come down to 3 main ones:
- Transporting blood cells and nutrients.
- Establishing communication between all body fluids that are located outside the circulatory system. This function is possible due to the ability of plasma to penetrate the vascular walls.
- Providing hemostasis. This involves controlling the fluid that stops bleeding and removing the resulting blood clot.
Diseases affecting plasma properties
In medicine, there are several diseases that can affect the composition of plasma. All of them pose a threat to human health and life.
The main ones are:
- Hemophilia. This is a hereditary pathology when there is a lack of protein, which is responsible for coagulation.
- Blood poisoning or sepsis. A phenomenon that occurs due to infection entering directly into the bloodstream.
- DIC syndrome. A pathological condition caused by shock, sepsis, severe injuries. It is characterized by blood clotting disorders, which simultaneously lead to bleeding and the formation of blood clots in small vessels.
- Deep venous thrombosis. With the disease, the formation of blood clots in the deep veins (mainly in the lower extremities) is observed.
- Hypercoagulation. Patients are diagnosed with excessive blood clotting. The viscosity of the latter increases.
Plasma test or Wasserman reaction is a study that detects the presence of antibodies in plasma to Treponema pallidum. Based on this reaction, syphilis is calculated, as well as the effectiveness of its treatment.
Human diseases that affect the composition and characteristics of plasma in the blood are extremely dangerous.
There is a list of diseases:
- Blood sepsis occurs when an infection enters directly into the circulatory system.
- Hemophilia in children and adults is a genetic deficiency of a protein responsible for clotting.
- Hypercoagulant state - clotting too quickly. In this case, blood viscosity increases and patients are prescribed drugs to thin it.
- Deep vein thrombosis is the formation of blood clots in the deep veins.
- DIC syndrome is the simultaneous occurrence of blood clots and bleeding.
Plasma is the liquid component of blood with a complex composition. It itself performs a number of functions, without which the life of the human body would be impossible.
For medical purposes, plasma in the blood is often more effective than a vaccine, since the immunoglobulins that make it up reactively destroy microorganisms.
How many liters of blood are there in a person?
5.5 liters is exactly the amount of blood in the body of an adult. 50 billion - this is the number of blood cells contained in 1 liter of blood - physically it is even impossible to imagine! One drop contains 300 thousand red cells. If you mentally combine these cells into a chain, without changing their actual size, then this chain can turn around the globe four times.
Despite their microscopic size, cells are capable of occupying a truly enormous area. For example, if these cells are covered with carpet, then its total area will be 4090 meters2. Since almost a quarter of the blood feeds the lungs all the time, this means that about 1000 meters2 of the surface of the blood cells comes into contact with air. Every second, the air sacs of our lungs pass through about 2 billion cells of this red liquid.
Since the air on the plain is under high pressure, the oxygen content in it is less than in the highlands. Therefore, where a person lives directly affects how many blood cells there are - the higher a person lives, the more of them he has. People living in the mountainous regions of Switzerland have 50 percent more blood cells than people living in London.
Blood plasma donation procedure
Those who plan to become donors very often experience psychological stress before the first donation, because they have no idea how donors donate plasma and what happens in the process. We will tell you in detail about what happens before the procedure, during plasma donation and after the donation.
Arriving at the clinic or blood transfusion center, the donor goes to the reception desk. At the initial appointment, they give him a card with basic information.
Then a preliminary medical examination is performed. It includes a general blood test, testing for antibodies to HIV, hepatitis, syphilis, identifying blood type, Rhesus and Kell antigen.
After the tests are completed, the donor is sent to a physician, who will review the test results, measure blood pressure and temperature, and decide whether the donor is eligible to donate plasma. After this, the doctor will briefly tell you how blood plasma is donated and answer all your questions.
After this, the donor proceeds directly to donating plasma. The procedure is carried out in a lying position, blood is drawn from one arm, it enters a special centrifuge, where it is divided into individual components: platelets and red blood cells are separated from the plasma cells themselves. Blood cells separated from the plasma are transferred to the second arm.
Donation lasts from 40 minutes to an hour, after completion it is recommended to lie down for a while, do not make sudden movements, drink a glass of strong sweet tea to restore strength. You should not leave the clinic for half an hour in case problems such as dizziness or loss of consciousness arise.
After donating plasma, a bandage is applied that cannot be removed for about two or three hours to prevent bleeding.
For two days after donation, it is better to avoid physical activity, hard work, and not to go to the gym.
Plasma proteins as laboratory indicators
In laboratory conditions, to determine the concentration of plasma proteins, you can work with plasma (blood is taken into a test tube with an anticoagulant) or test serum collected in a dry container. Serum proteins are no different from plasma proteins, with the exception of fibrinogen, which, as is known, is absent in blood serum and which, without an anticoagulant, is used to form a clot. The main proteins change their digital values in the blood during various pathological processes.
An increase in albumin concentration in serum (plasma) is a rare phenomenon that occurs with dehydration or with excessive intake (intravenous administration) of high concentrations of albumin. A decrease in albumin levels may indicate depleted liver function, kidney problems, or disorders in the gastrointestinal tract.
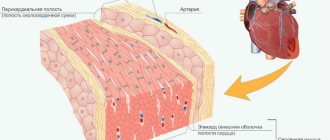
An increase or decrease in protein fractions is characteristic of a number of pathological processes, for example, acute-phase proteins alpha-1- and alpha-2-globulins, increasing their values, may indicate an acute inflammatory process localized in the respiratory organs (bronchi, lungs), affecting the excretory system ( kidneys) or heart muscle (myocardial infarction).
A special place in the diagnosis of various conditions is given to the gamma globulin (immunoglobulin) fraction. Determining antibodies helps to recognize not only an infectious disease, but also to differentiate its stage. The reader can obtain more detailed information about changes in the values of various proteins (proteinogram) in a separate material on globulins.
Deviations from the norm of fibrinogen manifest themselves as disturbances in the hemocoagulation system, therefore this protein is the most important laboratory indicator of blood coagulation abilities (coagulogram, hemostasiogram).
As for other proteins important for the human body, when examining serum, using certain techniques, you can find almost any that are interesting for diagnosing diseases. For example, by calculating the concentration of transferrin (beta-globulin, an acute-phase protein) in the sample and considering it not only as a “vehicle” (although this is probably the first thing), the doctor will know the degree of protein binding of ferric iron released by red blood cells, After all, Fe3+, as is known, when present in a free state in the body, gives a pronounced toxic effect.
The study of serum to determine the content of ceruloplasmin (acute phase protein, metalloglycoprotein, copper transporter) helps diagnose such a severe pathology as Konovalov-Wilson disease (hepatocerebral degeneration).
Thus, by examining plasma (serum), it is possible to determine the content of both those proteins that are vital and those that appear in a blood test as an indicator of a pathological process (for example, C-reactive protein).
The essence of the method
The method is based on the ability to artificially separate blood into elements and return the necessary components back to the patient’s body. A group of techniques is used.
Centifugation. Classic, common option. It is used if it is impossible to return the plasma. Accordingly, we are mainly talking about serious illnesses and intoxications. Including alcohol.
Saline and glucose move directly from the centrifuge in the opposite direction to restore normal blood concentration. Its volume. Otherwise, hypovolemia would occur.
Filtration. Since plasma contains the most toxins, life-threatening substances, the blood is automatically passed through a special membrane, hence the name - membrane plasmapheresis. The formed cells are too large to be transported through, only plasma passes through.
Further, everything depends on the concentration of toxins and toxic substances. If they cannot be removed, then the liquid fraction is replaced by artificial solutions. This avoids hypovolemia.
- The third method is based on more thorough cleaning of the liquid connective tissue. A system (cascade) of filters for plasma filtration is used. We are talking about the so-called double plasmapheresis. After complete treatment, the blood is returned to the patient's body. This method is only suitable if it can be purified and filtered.
- Cryo-plasmapheresis. The method involves 2 key stages. The first is blood processing. Dividing it into two main components. The plasma is frozen at a low temperature. No more than -30. Then, during the second “iteration,” the liquid fraction is heated to positive values and injected back into the body.
Attention:
Cryo-technique is risky, which is why it is used relatively rarely. Although it is superior in effectiveness to all previous ones, especially in cases of severe poisoning.
Blood plasma: composition and functions
Blood plasma is a viscous, homogeneous liquid of light yellow color. It makes up about 55-60% of the total blood volume. It contains blood cells in the form of a suspension. Plasma is usually clear, but may be slightly cloudy after eating a fatty meal. Consists of water and mineral and organic elements dissolved in it.
Plasma composition and functions of its elements
Most of the plasma is water, its amount is approximately 92% of the total volume. In addition to water, it includes the following substances:
- proteins;
- glucose;
- amino acids;
- fat and fat-like substances;
- hormones;
- enzymes;
- minerals (chlorine, sodium ions).
About 8% of the volume is proteins, which are the main part of plasma. It contains several types of proteins, the main ones being:
- albumins – 4-5%;
- globulins – about 3%;
- fibrinogen (belongs to globulins) – about 0.4%.
Other proteins
In addition to the above, plasma also contains other proteins:
- complement (immune proteins);
- transferrin;
- thyroxine-binding globulin;
- prothrombin;
- C-reactive protein;
- haptoglobin.
You can also read: Total protein in the blood
Non-protein components
In addition, blood plasma includes non-protein substances:
- organic nitrogen-containing: amino acid nitrogen, urea nitrogen, low molecular weight peptides, creatine, creatinine, indican. Bilirubin;
- organic nitrogen-free: carbohydrates, lipids, glucose, lactate, cholesterol, ketones, pyruvic acid, minerals;
- inorganic: sodium, calcium, magnesium, potassium cations, chlorine anions, iodine.
The ions in the plasma regulate the pH balance and maintain the normal state of cells.
Functions of proteins
Proteins have several purposes:
- homeostasis;
- ensuring the stability of the immune system;
- maintaining the aggregate state of the blood;
- nutrient transfer;
- participation in the process of blood clotting.
Use of donor plasma
In our time, transfusions often require not whole blood, but its components and plasma. Therefore, blood transfusion centers often donate blood for plasma.
It is obtained from whole blood by centrifugation, that is, the liquid part is separated from the formed elements using a machine, after which the blood cells are returned to the donor. The procedure lasts about 40 minutes.
The difference from donating whole blood is that blood loss is much less, and you can donate plasma again after two weeks, but no more than 12 times during the year.
Blood serum is obtained from plasma, which is used for medicinal purposes. It differs from plasma in that it does not contain fibrinogen, but contains all the antibodies that can resist pathogens.
To obtain it, place sterile blood in a thermostat for an hour. Then the resulting clot is peeled off from the wall of the test tube and kept in the refrigerator for a day.
After this, using a Pasteur pipette, the settled whey is poured into a sterile container.
Conclusion
Blood plasma is its liquid component, which has a very complex composition. Plasma performs important functions in the body.
In addition, donor plasma is used for transfusion and preparation of therapeutic serum, which is used for the prevention and treatment of infections, as well as for diagnostic purposes to identify microorganisms obtained during analysis. It is considered more effective than vaccines.
Immunoglobulins contained in serum immediately neutralize harmful microorganisms and their metabolic products, and passive immunity is formed faster.
All about plasma
Plasma is a liquid formed by water and dry substances. It makes up the bulk of the blood - about 60%. Thanks to plasma, blood has a liquid state. Although according to physical indicators (density) plasma is heavier than water.
Macroscopically, plasma is a transparent (sometimes cloudy) homogeneous liquid of light yellow color. It collects in the upper part of the vessels when the formed elements settle. Histological analysis shows that plasma is the intercellular substance of the liquid part of the blood.
Plasma becomes cloudy after a person consumes fatty foods.
What is dry plasma?
The occurrence of any malfunction or disorder in our body leads to the fact that, in the presence of these factors, it requires special treatment and blood transfusion. Both plasma after the fraction and a certain part of the blood may be required, with the help of which the lost fluid is completely restored.
Most often, the occurrence of such situations is associated with vascular insufficiency, which occurs in the following cases:
- Severe blood loss.
- A state of shock that occurs after receiving a severe burn.
- Shock that occurs after injuries with tissue ruptures.
In this case, dry plasma acts as a substitute. Before introducing it into the human body, dry plasma is first dissolved in water. Only doctors know the exact concentration, who carefully monitor it before administering it intravenously to a person. Despite the fact that dry plasma, once it enters the body, is capable of restoring lost blood volumes, there is a risk that after its administration a person will develop hepatitis.
To ensure that after the procedure the patient does not become infected with the hepatitis virus, specialists develop and compile various techniques, the use of which significantly increases the chances of successful treatment. For example, if it is stored at room temperature or if it has been heat sterilized to preserve substances such as lithium or insulin, then the chances of contracting hepatitis are significantly reduced. It should be noted that today, in order to reduce the number of infected patients, in medical practice only blood plasma that has been sterilized is used, and it must also have a certain concentration.
How to determine a person's blood volume?
For this purpose, a certain amount of a contrast agent, usually a harmless dye, is injected into the blood. After it is distributed throughout the riverbed, a fence is made to determine its concentration.
Another way is to inject radioactive isotopes and count the number of red blood cells that contain them. The amount of blood is determined by the level of its radioactivity.
Blood transfusion is used to normalize blood volume in the body.
Globulins
The remaining plasma proteins are classified as globulins, which are large in molecular weight. They are produced in the liver and in the organs of the immune system. Main types:
- alpha globulins,
- beta globulins,
- gamma globulins.
Alpha globulins bind bilirubin and thyroxine, activate the production of proteins, transport hormones, lipids, vitamins, and microelements.
Beta globulins bind cholesterol, iron, vitamins, transport steroid hormones, phospholipids, sterols, zinc and iron cations.
Gamma globulins bind histamine and participate in immunological reactions, which is why they are called antibodies, or immunoglobulins. There are five classes of immunoglobulins: IgG, IgM, IgA, IgD, IgE. Produced in the spleen, liver, lymph nodes, and bone marrow. They differ from each other in biological properties and structure. They have different abilities to bind antigens, activate immune proteins, have different avidity (rate of binding to antigen and strength) and ability to pass through the placenta. Approximately 80% of all immunoglobulins are IgG, which have high avidity and are the only ones that can cross the placenta. IgM is synthesized first in the fetus. They are also the first to appear in the blood serum after most vaccinations. They have high avidity.
Blood composition
Fibrinogen is a soluble protein that is produced in the liver. Under the influence of thrombin, it is converted into insoluble fibrin, due to which a blood clot is formed at the site of vessel damage.
Chapter 14. BLOOD BIOCHEMISTRY
In sports practice, blood tests are used to assess the impact of training and competitive loads on the athlete’s body, to assess the athlete’s functional state and his health. The information obtained from blood testing helps the coach manage the training process. Therefore, a specialist in the field of physical education must have the necessary understanding of the chemical composition of blood and its changes under the influence of physical activity of various types.
General characteristics of blood
A person's blood volume is about 5 liters, which is approximately 1/13 of the volume or weight of the body.
By its structure, blood is a liquid tissue and, like any tissue, consists of cells and intercellular fluid.
Blood cells are called formed elements
.
These include red cells (erythrocytes),
white cells
(leukocytes)
and blood platelets
(platelets).
Cells account for about 45% of blood volume.
The liquid part of the blood is called plasma
.
Plasma volume is approximately 55% of blood volume. Blood plasma from which the fibrinogen protein has been removed is called serum
.
Biological functions of blood
The main functions of blood are the following:
1. Transport function
. This function is due to the fact that blood constantly moves through the blood vessels and transports substances dissolved in it. There are three types of this function.
Trophic function
.
With the blood, substances necessary to ensure metabolism in them (energy sources, building material for synthesis, vitamins, salts, etc.) are delivered to all organs.
Respiratory function
. Blood is involved in the transfer of oxygen from the lungs to the tissues and the transfer of carbon dioxide from the tissues to the lungs.
Excretory function (excretory).
With the help of blood, the final products of metabolism are transported from tissue cells to the excretory organs with their subsequent removal from the body.
2. Protective function
. This function, first of all, is to provide immunity - protecting the body from foreign molecules and cells. The protective function also includes the ability of blood to clot. In this case, the body is protected from blood loss.
3. Regulatory function
. Blood is involved in ensuring a constant body temperature, maintaining a constant pH and osmotic pressure. With the help of blood, hormones - metabolic regulators - are transferred.
All of these functions are aimed at maintaining the constancy of the internal environment of the body - homeostasis
(constancy of the chemical composition, acidity, osmotic pressure, temperature, etc. in the cells of the body).
Chemical composition of blood plasma.
The chemical composition of blood plasma at rest is relatively constant. The main components of plasma are as follows:
Water - 90%
Proteins - 6-8%
Other organic
substances - about 2%
Minerals - about 1%
Blood plasma proteins
are divided into two fractions:
albumins
and
globulins
. The ratio between albumins and globulins is called the “albumin-globulin coefficient” and is equal to 1.5 – 2. Performing physical activity is initially accompanied by an increase in this coefficient, and with very long work it decreases.
Albumin
– low molecular weight proteins with a molecular weight of about 70 thousand. Yes. They perform two main functions.
Firstly, due to their good solubility in water, these proteins perform a transport function, carrying various water-insoluble substances (for example, fats, fatty acids, some hormones, etc.) through the bloodstream.
Secondly, due to their high hydrophilicity, albumins have significant hydration (water)
membrane and therefore retain water in the bloodstream.
Water retention in the bloodstream is necessary due to the fact that the water content in the blood plasma is higher than in the surrounding tissues, and water, due to diffusion, tends to leave the blood vessels into the tissues. Therefore, with a significant decrease in albumin in the blood (during fasting, loss of proteins in the urine due to kidney disease),
edema occurs.
Globulins
– these are high-molecular proteins with a molecular weight of about 300 thousand. Yes. Like albumins, globulins also perform a transport function and promote water retention in the bloodstream, but in this they are significantly inferior to albumins. However, globulins
There are also very important functions. Thus, some globulins are enzymes and accelerate chemical reactions that occur directly in the bloodstream. Another function of globulins is their participation in blood clotting and in providing immunity (protective function).
Most plasma proteins are synthesized in the liver.
Other organic substances (except proteins)
usually divided into two groups:
nitrogenous
and
nitrogen-free
.
Nitrogen compounds
- These are intermediate and final products of the metabolism of proteins and nucleic acids.
Intermediate products of protein metabolism in blood plasma include low molecular weight peptides
,
amino acids
, and
creatine
.
The end products of protein metabolism are, first of all, urea (its concentration in the blood plasma is quite high - 3.3-6.6 mmol/l),
bilirubin (
the end product of heme breakdown
) and
creatinine (the end product of creatine phosphate breakdown).
Among the intermediate products of nucleic acid metabolism in blood plasma, nucleotides
,
nucleosides
,
nitrogenous bases
.
The end product of the breakdown of nucleic acids is uric acid
, which is always found in small concentrations in the blood.
To assess the content of non-protein nitrogenous compounds in the blood, the “
non-protein nitrogen ”
.
Non-protein nitrogen includes the nitrogen of low molecular weight (non-protein)
compounds, mainly those listed above, which remain in the plasma or serum after the removal of proteins. Therefore, this indicator is also called “residual nitrogen”. An increase in residual nitrogen in the blood is observed with kidney disease, as well as with prolonged muscular work.
To nitrogen-free substances
blood plasma includes
carbohydrates
and
lipids
, as well as intermediate products of their metabolism.
The main carbohydrate in plasma is glucose
.
Its concentration in a healthy person at rest and in a fasting state fluctuates in a narrow range from 3.9 to 6.1 mmol/l (or 70-110 mg%).
Glucose enters the blood as a result of absorption from the intestine during the digestion of dietary carbohydrates, as well as during the mobilization of liver glycogen.
In addition to glucose, plasma also contains small amounts of other monosaccharides - fructose
,
galactose, ribose
,
deoxyribose
, etc. Intermediate products of carbohydrate metabolism in plasma are represented
by pyruvic
and
lactic
acids.
At rest, the content of lactic acid (lactate)
is low - 1-2 mmol/l.
Under the influence of physical activity, and especially intense physical activity, the concentration of lactate in the blood increases sharply (even tens of times!).
Lipids are represented in blood plasma by fat
,
fatty acids
,
phospholipids
and
cholesterol
. Due to its insolubility in water, everything
lipids are associated with plasma proteins: fatty acids with albumin, fat, phospholipids and cholesterol with globulins. , ketone bodies are always present in plasma
.
Minerals
are in the blood plasma in the form of cations
(Na+, K+, Ca2+, Mg2+, etc.)
and anions
(Cl-, HCO3-, H2PO4-, HPO42-, SO42_, J-, etc.).
Plasma contains the most sodium, potassium, chlorides, and bicarbonates. Deviations in the mineral composition of blood plasma can be observed in various diseases and in cases of significant water loss due to sweating during physical work.
The content of the main blood components is presented in table. 6.
Table 6. Main blood components
| Component | Concentration in traditional units | Concentration in SI units |
| B e l k i | ||
| Total protein | 6-8 % | 60-80 g/l |
| Albumin | 3,5- 4,5 % | 35-45 g/l |
| Globulins | 2,5 — 3,5 % | 25-35 g/l |
| Hemoglobin in men and women | 13,5-18 % 12-16 % | 2.1-2.8 mmol/l 1.9-2.5 mmol/l |
| Fibrinogen | 200-450 mg% | 2-4.5 g/l |
| Non-protein nitrogenous substances | ||
| Residual nitrogen | 20-35 mg% | 14-25 mmol/l |
| Urea | 20-40 mg% | 3.3-6.6 mmol/l |
| Creatine | 0.2-1 mg% | 15-75 µmol/l |
| Creatinine | 0.5-1.2 mg% | 44-106 µmol/l |
| Uric acid | 2-7 mg% | 0.12-0.42 mmol/l |
| Bilirubin | 0.5-1 mg% | 8.5-17 µmol/l |
| Nitrogen-free substances | ||
| Glucose (on an empty stomach) | 70-110 mg% | 3.9-6.1 mmol/l |
| Fructose | 0.1-0.5 mg% | 5.5-28 µmol/l |
| Lactate tarterial blood venous blood | 3-7 mg% 5-20 mg% | 0.33-0.78 mmol/l 0.55-2.2 mmol/l |
| Ketone bodies | 0.5-2.5 mg% | 5-25 mg/l |
| General lipids | 350-800 mg% | 3.5-8 g/l |
| Triglycerides | 50-150 mg% | 0.5-1.5 g/l |
| Cholesterol | 150-300 mg% | 4-7.8 mmol/l |
| Minerals | ||
| Sodium plasma red blood cells | 290-350 mg% 31-50 mg% | 125-150 mmol/l 13.4-21.7 mmol/l |
| Potassium plasma red blood cells | 15-20 mg% 310-370 mg% | 3.8-5.1 mmol/l 79.3-99.7 mmol/l |
| Chlorides | 340-370 mg% | 96-104 mmol/l |
| Calcium | 9-11 mg% | 2.2-2.7 mmol/l |
Red cells (erythrocytes))
Red blood cells make up the bulk of blood cells. In 1 mm3 (µl [1]
)
blood usually contains 4-5 million red cells.
Red blood cells are formed in the red bone marrow, function in the bloodstream and are destroyed mainly in the spleen and liver. The life cycle of these cells is 110-120 days. Red blood cells are biconcave cells lacking nuclei, ribosomes and mitochondria. In this regard, processes such as protein synthesis and tissue respiration do not occur in them. The main source of energy for red blood cells is the anaerobic breakdown of glucose (glycolysis).
The main component of red cells is the protein hemoglobin
.
It accounts for 30% of the mass of the red blood cell or 90% of the dry residue of these cells. In its structure, hemoglobin is a chromoprotein. Its molecule has a quaternary structure and consists of four subunits
.
Each subunit contains one polypeptide
and one
heme
.
The subunits differ from each other only in the structure of the polypeptides. Heme is a complex cyclic structure of four pyrrole rings containing a divalent iron
(Fe2+) in the center:
The main function of red blood cells is respiratory
.
oxygen
is transferred from the lungs to the tissues and
carbon dioxide
from the tissues to the lungs.
In the capillaries of the lungs, the partial pressure of oxygen is about 100 mmHg. Art. (partial pressure is the part of the total pressure of a mixture of gases attributable to an individual gas from this mixture. For example, at an atmospheric pressure of 760 mm Hg, the share of oxygen is 152 mm Hg, i.e. 1/5 of the part, so air usually contains 20% oxygen).
At this pressure, almost all hemoglobin binds to oxygen:
Hb + O2 ¾® HbO2
Hemoglobin Oxyhemoglobin
Oxygen attaches directly to the iron atom that is part of the heme, and only divalent (reduced)
iron.
Therefore, various oxidizing agents (for example, nitrates, nitrites, etc.),
converting iron from divalent to trivalent
(oxidized),
disrupt the respiratory function of the blood.
The resulting complex of hemoglobin with oxygen is oxyhemoglobin
It is transported through the bloodstream to various organs. Due to the consumption of oxygen by tissues, its partial pressure here is much lower than in the lungs. At low partial pressure, oxyhemoglobin dissociates:
HbO2 ¾® Hb + O2
The degree of decomposition of oxyhemoglobin depends on the magnitude of the partial pressure of oxygen: the lower the partial pressure, the more oxygen is split off from oxyhemoglobin. For example, in muscles at rest the partial pressure of oxygen is approximately 45 mmHg. Art. At this pressure, only about 25% of oxygenated hemo-
globin. When working at moderate power, the partial pressure of oxygen in the muscles is approximately 35 mmHg. Art. and about 50% of oxyhemoglobin is already degraded. When performing intense exercise, the partial pressure of oxygen in the muscles decreases to 15-20 mmHg. Art., which causes a deeper dissociation of oxyhemoglobin (by 75% or more). This nature of the dependence of the dissociation of oxyhemoglobin on the partial pressure of oxygen makes it possible to significantly increase the supply of oxygen to muscles when performing physical work.
Increased dissociation of oxyhemoglobin is also observed with increasing body temperature and increasing blood acidity (for example, when large amounts of lactic acid enter the blood during intense muscular work),
which also contributes to a better supply of oxygen to tissues.
In general, a person who does not perform physical work uses 400-500 liters of oxygen per day. With high physical activity, oxygen consumption increases significantly.
Transport of carbon dioxide
carried out from the tissues of all organs, where its formation occurs in the process of catabolism, into the lungs, from which it is released into the external environment.
Most carbon dioxide is carried in the blood in the form of salts called bicarbonates
potassium and sodium.
The conversion of CO2 into bicarbonates occurs in red blood cells with the participation of hemoglobin. (KHCO3)
accumulate in red blood cells and sodium bicarbonates
(NaHCO3) accumulate in blood plasma.
With the blood flow, the resulting bicarbonates enter the lungs and are converted there again into carbon dioxide, which is removed from the lungs with
exhaled air. This transformation also occurs in red blood cells, but with the participation of oxyhemoglobin, which occurs in the capillaries of the lungs due to the addition of oxygen to hemoglobin (see above).
The biological meaning of this mechanism for the transfer of carbon dioxide in the blood is that potassium and sodium bicarbonates are highly soluble in water, and therefore they can be present in significantly larger quantities in red blood cells and plasma compared to carbon dioxide.
A small portion of CO2 can be carried in the blood physically dissolved and also in a complex with hemoglobin called carbhemoglobin
.
At rest, 350-450 liters of CO2 are formed and released from the body per day. Performing physical activity leads to an increase in the formation and release of carbon dioxide.
White cells
(
leukocytes )
Unlike red cells, leukocytes are full-fledged cells with a large nucleus and mitochondria, and therefore such important biochemical processes as protein synthesis and tissue respiration occur in them.
At rest in a healthy person, 1 mm3 of blood contains 6-8 thousand leukocytes. In diseases, the number of white cells in the blood may decrease (leukopenia),
and increase
(leukocytosis).
Leukocytosis can also be observed in healthy people, for example, after eating or during muscular work
(myogenic leukocytosis).
With myogenic leukocytosis, the number of leukocytes in the blood can increase to 15-20 thousand/mm3 or more.
There are three types of leukocytes: lymphocytes
(25-26%),
monocytes
(6-7%) and
granulocytes
(67-70%).
Lymphocytes are formed in the lymph nodes and spleen, and monocytes and granulocytes are formed in the red bone marrow.
Leukocytes perform protective
function, participating in the provision of
immunity
.
In its most general form, immunity is the body’s defense against everything “foreign.” By “foreign” we mean various foreign high-molecular substances that have the specificity and uniqueness of their structure and, as a result, differ from the body’s own molecules.
Currently, there are two forms of immunity: specific
and
non-specific
. Specific immunity usually means immunity itself, and nonspecific immunity refers to various factors of nonspecific defense of the body.
The specific immune system includes the thymus
(thymus gland)
, spleen, lymph nodes,
lymphoid accumulations (in the nasopharynx, tonsils, appendix, etc.)
and
lymphocytes
. The basis of this system is lymphocytes.
Any foreign substance to which the body's immune system is capable of reacting is called an antigen.
.
All “foreign” proteins, nucleic acids, many polysaccharides and complex lipids have antigenic properties. Antigens can also be bacterial toxins and whole cells of microorganisms, or more precisely the macromolecules that make up them. In addition, low molecular weight compounds, such as steroids and some drugs, can also exhibit antigenic activity, provided they are previously bound to a carrier protein, for example, blood plasma albumin. (This is the basis for the detection of some doping drugs by the immunochemical method during doping control).
The antigen that enters the bloodstream is recognized by special leukocytes - T-lymphocytes, which then stimulate the transformation of another type of leukocyte - B-lymphocytes into plasma cells, which then synthesize special proteins - antibodies
or
immunoglobulins
. The larger the antigen molecule, the more different antibodies are formed in response to its entry into the body. Each antibody has two binding sites for interaction with a strictly defined antigen. Thus, each antigen causes the synthesis of strictly specific antibodies.
The resulting antibodies enter the blood plasma and bind there to the antigen molecule. The interaction of antibodies with antigen is carried out through the formation of non-covalent bonds between them. This interaction is analogous to the formation of an enzyme-substrate complex during enzymatic catalysis, with the binding site of the antibody corresponding to the active site of the enzyme. Since most antigens are high-molecular compounds, many antibodies simultaneously attach to the antigen.
antigen-antibody complex
further undergoes
phagocytosis
.
If the antigen is a foreign cell, then the antigen-antibody complex is exposed to enzymes in the blood plasma under the general name of the complement system .
This complex enzymatic system ultimately causes lysis of the foreign cell, i.e.
its destruction. The resulting lysis products are then also subject to phagocytosis
.
Since antibodies are formed in excess quantities in response to the arrival of antigen, a significant part of them remains for a long time in the blood plasma, in the g-globulin fraction. A healthy person’s blood contains a huge amount of different antibodies formed as a result of contact with many foreign substances and microorganisms. The presence of ready-made antibodies in the blood allows the body to quickly neutralize antigens newly entering the blood. Preventive vaccinations are based on this phenomenon.
Other forms of leukocytes are monocytes
and
granulocytes
participate in
phagocytosis
. Phagocytosis can be considered as a nonspecific protective reaction, aimed primarily at the destruction of microorganisms entering the body. During the process of phagocytosis, monocytes and granulocytes engulf bacteria, as well as large foreign molecules, and destroy them with their lysosomal enzymes. Phagocytosis is also accompanied by the formation of reactive oxygen species, the so-called free oxygen radicals, which, by oxidizing the lipoids of bacterial membranes, contribute to the destruction of microorganisms.
As noted above, antigen-antibody complexes are also subject to phagocytosis.
Nonspecific protection factors include skin and mucous barriers, bactericidal gastric juice, inflammation, enzymes (lysozyme, proteinases, peroxidases)
, antiviral protein - interferon, etc.
Regular sports and recreational physical education stimulate the immune system and nonspecific defense factors and thereby increase the body's resistance to the effects of adverse environmental factors, help reduce general and infectious morbidity, and increase life expectancy.
However, exceptionally high physical and emotional overloads characteristic of elite sports have an adverse effect on the immune system. Highly qualified athletes often experience an increased incidence of illness, especially during important competitions (it is at this time that physical and emotional stress reaches its limit!).
Excessive loads are very dangerous for a growing body. Numerous evidence suggests that the immune system of children and adolescents is more sensitive to such stress.
In this regard, the most important medical and biological task of modern sports is the correction of immunological disorders in highly qualified athletes through the use of various immunostimulating agents.
Blood platelets
(
platelets ).
Platelets are anucleate cells formed from the cytoplasm of megakaryocytes - bone marrow cells. The number of platelets in the blood is usually 200-400 thousand/mm3. The main biological function of these formed elements is participation in the process of blood clotting
.
Blood clotting
- a complex enzymatic process leading to the formation of a blood clot -
a thrombus
in order to prevent blood loss when blood vessels are damaged.
Blood clotting involves components of platelets, components of blood plasma, as well as substances entering the bloodstream from surrounding tissues. All substances involved in this process are called coagulation factors
.
By structure, all coagulation factors except two (Ca2+ ions and phospholipids)
are proteins and are synthesized in the liver, and vitamin K is involved in the synthesis of a number of factors.
Protein coagulation factors enter the bloodstream and circulate in it in an inactive form - in the form of proenzymes (enzyme precursors),
which, if a blood vessel is damaged, can become active enzymes and participate in the process of blood clotting. Thanks to the constant presence of proenzymes, the blood is always in a state of “readiness” to clot.
In its most simplified form, the process of blood clotting can be divided into three large stages.
At the first stage, which begins when the integrity of the blood vessel is disrupted, platelets very quickly (within seconds)
accumulate at the site of injury and, sticking together, form a kind of “plug” that limits bleeding.
In this case, some platelets are destroyed, and phospholipids (one of the coagulation factors) are released into the blood plasma.
At the same time, in the plasma, due to contact with the damaged surface of the vessel wall or with any foreign body
(for example, a needle, glass, knife blade, etc.),
another coagulation factor is activated -
contact factor
.
Next, with the participation of these factors, as well as some other coagulation participants, an active enzyme complex called prothrombinase
or
thrombokinase is formed.
This mechanism of activation of prothrombinase is called internal, since all participants in this process are contained in the blood. Active prothrombinase is also formed by an external mechanism. In this case, the participation of a coagulation factor that is absent in the blood itself is required. This factor is present in the tissues surrounding blood vessels and enters the bloodstream only when the vascular wall is damaged. The presence of two independent mechanisms for activating prothrombinase increases the reliability of the blood coagulation system.
prothrombin
(this is also a coagulation factor)
is converted into an active enzyme -
thrombin
.
The third stage begins with the effect of the resulting thrombin on the plasma protein - fibrinogen
.
Part of the molecule is split off from fibrinogen and fibrinogen is converted into a simpler protein - fibrin monomer
, the molecules of which spontaneously, very quickly, without the participation of any enzymes, undergo polymerization to form long chains called
fibrin polymer
.
The resulting fibrin-polymer threads form the basis of a blood clot - a thrombus. First, a gelatinous clot is formed, which includes, in addition to fibrin-polymer threads, plasma and blood cells. Next, from the platelets included in this clot, special contractile proteins (such as muscle proteins) are released,
causing compression
(retraction)
of the blood clot.
As a result of these steps, a durable blood clot is formed, consisting of fibrin-polymer threads and blood cells. This thrombus is located in a damaged area of the vascular wall and prevents bleeding.
All stages of blood clotting occur with the participation of calcium ions.
In general, the blood clotting process takes 4-5 minutes.
Within a few days after the formation of a blood clot, after the integrity of the vascular wall is restored, the now no longer needed blood clot is reabsorbed. This process is called fibrinolysis
and is carried out by the breakdown of fibrin, which is part of the blood clot, under the action of the enzyme
plasmin (fibrinolysin).
This enzyme is formed in the blood plasma from its predecessor, the proenzyme plasminogen, under the influence of activators that are in the plasma or enter the bloodstream from surrounding tissues. Plasmin activation is also facilitated by the formation of fibrin polymer during blood coagulation.
Recently it has been found that the blood still contains anticoagulant
a system that limits the coagulation process to only the damaged area of the bloodstream and does not allow total coagulation of all blood.
Substances of plasma, platelets and surrounding tissues, which are collectively called anticoagulants, participate in the formation of the anticoagulant system.
According to the mechanism of action, most anticoagulants are specific inhibitors acting on coagulation factors.
The most active anticoagulants are antithrombins, which prevent the conversion of fibrinogen to fibrin. The most studied thrombin inhibitor is heparin
, which prevents blood clotting both in vivo and in vitro.
The anticoagulation system can also include the fibrinolysis system.
Acid-base balance of blood
At rest in a healthy person, the blood has a slightly alkaline reaction: pH of capillary blood (usually taken from a finger)
is approximately 7.4, the pH of venous blood is 7.36. The lower pH value of venous blood is explained by the higher content of carbon dioxide in it, which arises during the metabolic process.
The constancy of blood pH is ensured by buffer systems found in the blood. The main blood buffers are: bicarbonate
(H2CO3/NaHCO3),
phosphate
(NaH2PO4/Na2HPO4),
protein
and
hemoglobin
.
The hemoglobin system turned out to be the most powerful buffering system in the blood: it accounts for 3/4 of the total buffering capacity of the blood (see the chemistry course for the mechanism of buffering action).
In all blood buffer systems, basic (alkaline)
component, as a result of which they neutralize acids entering the blood much better than alkalis.
This feature of blood buffers is of great biological importance, since during metabolism, various acids are often formed as intermediate and final products (pyruvic and lactic acids - during the breakdown of carbohydrates; metabolites of the Krebs cycle and b-oxidation of fatty acids; ketone bodies, carbonic acid, etc. .).
All acids arising in the cells can enter the bloodstream and cause a pH shift to the acidic side. The presence of a large buffer capacity in relation to acids in blood buffers allows them to neutralize significant amounts of acidic products entering the blood, and thereby help maintain a constant level of acidity.
The total content in the blood of the main components of all buffer systems is designated by the term “
Alkaline blood reserve ”.
Most often, alkaline reserve is calculated by measuring the blood's ability to bind CO2. Normally in humans its value is 50-65 vol. %, i.e. Every 100 ml of blood can bind from 50 to 65 ml of carbon dioxide.
(kidneys, lungs, skin, intestines) also participate in maintaining a constant blood pH
These organs remove excess acids and bases from the blood.
Thanks to buffer systems and excretory organs, fluctuations in pH under physiological conditions are insignificant and not dangerous to the body.
However, in case of metabolic disorders (in diseases, when performing intense muscle loads)
The formation of acidic or alkaline substances in the body
(primarily acidic!) may sharply increase.
In these cases, the blood buffer systems and excretory organs are unable to prevent their accumulation in the bloodstream and maintain the pH value at a constant level.
Therefore, with excessive formation of various acids in the body, the acidity of the blood increases, and the pH value decreases. This phenomenon is called acidosis
.
With acidosis, blood pH can decrease to 7.0 - 6.8 units. (It should be remembered that a shift in pH by one unit corresponds to a change in acidity by a factor of 10).
A decrease in pH value below 6.8 is incompatible with life.
Accumulation of alkaline compounds in the blood may occur much less frequently, and the blood pH will increase. This phenomenon is called alkalosis
. The maximum increase in pH is 8.0.
Athletes often experience acidosis caused by the formation of large amounts of lactic acid (lactate) in the muscles during intense work.
Chapter 15. BIOCHEMISTRY OF KIDNEYS AND URINE
Urine, like blood, is often the object of biochemical studies conducted in athletes. Based on urine analysis, a coach can obtain the necessary information about the athlete’s functional state, about the biochemical changes that occur in the body when performing physical activity of various types. Since when taking blood for analysis, the athlete may become infected (for example, contracting hepatitis or AIDS)
, then recently urine testing has become increasingly preferable. Therefore, a coach or physical education teacher must have information about the mechanism of urine formation, its physical and chemical properties and chemical composition, and changes in urine parameters when performing training and competitive loads.
[1] 1 µl = 1·10-6 l
Blood plasma: composition, properties, functions, what it is needed for, plasma for transfusion
Z. Nelly Vladimirovna, laboratory diagnostics doctor at the Research Institute of Transfusiology and Medical Biotechnology, especially for SosudInfo.ru (about the authors)
Blood plasma is the first (liquid) component of the most valuable biological medium called blood. Blood plasma takes up up to 60% of the total blood volume. The second part (40 - 45%) of the fluid circulating through the bloodstream is taken up by formed elements: red blood cells, leukocytes, platelets.
The composition of blood plasma is unique. What's not there? Various proteins, vitamins, hormones, enzymes - in general, everything that ensures the life of the human body every second.
Briefly about the history of manipulation
In Moscow, since 1926, the National Medical Research Center of Hematology has been operating - the leading scientific center in Russia. It turns out that the first attempts at blood transfusion were recorded in the Middle Ages. The majority of them were not successful.
The reason for this can be attributed to the almost complete lack of scientific knowledge in the field of transfusiology and the impossibility of establishing group and Rh affiliation.
Transfusion of blood plasma in the event of antigen incompatibility is doomed to the death of the recipient, so today doctors have abandoned the practice of administering whole blood in favor of implanting its individual components. This method is considered safer and more effective.
Risks for the recipient
Even though a blood transfusion is somewhat similar to administering saline or medication by drip, the procedure is more complex.
Blood transfusion is a manipulation equivalent to the transplantation of biological living tissue.
Implanted materials, including blood, contain many different cellular components that carry foreign antigens, proteins, and molecules.
Any intervention carries risks that do not depend on the qualifications of the doctor or on preliminary preparation for the procedure. At the same time, at any stage of plasma transfusion (sample or direct infusion), a superficial attitude of medical staff towards work, haste or lack of a sufficient level of qualifications is unacceptable.
Main components
Like any concentrated solution, blood can be divided into a liquid part (plasma) and formed elements, which include red blood cells, platelets and leukocytes. Normally, the ratio between them is maintained at 4:6 (40-45% falls on the elements).
Doctors call this indicator “hematocrit”. Changes indicate increased blood density (more than 45%) due to loss of fluid through sweat, diarrhea, and massive burns. The opposite option is possible: blood thinning due to impaired synthesis and lack of formed elements, the introduction of a large volume of fluid.