Experienced hypertensive patients, as a rule, are adapted to living with high blood pressure (BP) levels and are usually well aware of what they need to take to maintain optimal blood pressure values for themselves.
They also know what they should not do so as not to provoke a sharp rise in pressure upward. And the most disciplined ones measure their blood pressure every morning and record the readings in a diary before taking their antihypertensive pills.
If, with grade 2–3 hypertension, it is possible to keep blood pressure at 140/150 at 90/100 mmHg in this way. Art., which means that this is a relatively stable course of hypertension. But if one day a hypertensive patient suddenly has a blood pressure of 120 over 100, what does this mean? Does such a collapse in the systolic indicator indicate victory over hypertension or is this a new round of pathology fraught with unknown dangers?
What does pressure 120 per 100 mm Hg mean? Art.?
To figure out whether such indicators are optimal for a person accustomed to high blood pressure, consider a pressure of 120 to 100 for each value separately.
- Systolic reading 120 mmHg. Art. for a patient suffering from hypertension, this cannot be called the norm, since his body, in particular, the circulatory system has already adapted to function at higher values, which means that 120 mm in this case is low blood pressure.
- Diastolic reading 100 mmHg. Art. for most hypertensive patients it is quite tolerable, although elevated relative to the classical norm.
- The difference between systolic and diastolic blood pressure (pulse pressure) is 20 mm, that is, less than 25% of systolic blood pressure, which means there are serious disturbances in the functioning of the vascular system.
Why could such an imbalance in the indicators arise? What does a pressure of 120 to 100 mean - is this a variant of the norm or is it still low blood pressure? In a specific case, only the “upper” systolic pressure can be considered low, which indicates insufficiency of cardiac output (actually, systole).
Why did the diastolic indicator remain at an elevated level, and not decrease synchronously with the upper blood pressure? A high level of diastolic pressure indicates increased resistance of the peripheral vessels of the bloodstream, which means a narrowing of the capillaries. The reason for this condition may lie in the ordinary “clogging” of small vessels with cholesterol.
When asked what a pressure of 120 over 100 means, we can answer that a person has signs of insufficient cardiac output against the background of increased capillary resistance.
Prevention
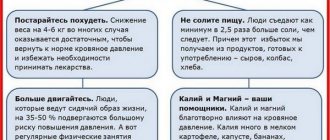
To avoid an increase in diastolic pressure and the development of hypertension, adhere to the following rules:
- Increase your level of physical activity if you have a sedentary lifestyle.
- Reduce your salt intake in pure form, as well as in prepared foods (fast food, takeaway, sauces).
- Don't overload your body, give it a rest, walk in the fresh air or do calm, favorite things.
- Reduce your stress levels.
- Cigarettes and booze are your worst enemies, forget about them.
- Give up coffee.
- Distribute your meals, make a meal schedule, and don’t overeat.
- Get rid of excess weight.
The circulatory system will quickly return to normal if you follow these tips. Without pills, you can eliminate hypertension in the initial stages, the main thing is to constantly measure your blood pressure to control it, and lead a healthy lifestyle.
Why is the heart rate high?
An increased pulse is considered to be an attribute of arterial hypertension, but even with a pressure of 120 per 100, a pulse of 100 or even 120 beats per minute is not uncommon, but rather the rule. Increased heart rate is explained by the heart's attempt to compensate for insufficient cardiac output.
If a compensatory response in the form of an accelerated heartbeat is observed at a pressure of 120 over 100 (pulse 120), it means that the body is trying to prevent a vascular or cerebral catastrophe. But despite the efforts of the cardiovascular system to restore normal blood circulation by increasing the heart rate, this condition cannot be called harmless.
Causes
What are the reasons for its occurrence? The abuse of drinks containing caffeine and some other natural causes have already been mentioned above. However, this is not a complete list and cardiologists supplement it:
- pathological processes that occur in the body;
- chronic lack of sleep;
- frequent stress;
- constant overwork;
- vegetative-vascular dystonia;
- poor environment;
- overweight;
- sedentary lifestyle.
Moreover, blood pressure can be affected by:
- Times of Day;
- mood;
- narcotic substances;
- medicines;
- eating heavy food before bed;
- uncomfortable body position during sleep.
What is the danger?
Why is a noticeable decrease in blood pressure dangerous for hypertensive patients? Isn’t antihypertensive therapy aimed at lowering blood pressure?
- A sharp drop in blood pressure in hypertensive patients is a clear sign of deterioration in perfusion, that is, cerebral circulation, which means that the process of cerebral ischemia has begun, which increases the risk of developing an ischemic stroke.
- There is also a cardiological danger with a pressure of 120 over 100. What kind of danger this is becomes clear when the pulse rises to 100 or 120 beats per minute. This means that the heart begins to pump blood at an increased rate, which is why the heart muscle undergoes additional stress and is depleted faster. The risk of developing a heart attack increases several times.
- In any case, a pressure of 120 to 100 indicates a loss of the body’s ability to compensate for the forces aimed at increased blood circulation, and therefore a decrease in vascular tone.
- Deterioration of vascular tone often causes orthostatic hypotension - a sharp drop in blood pressure when changing body position (from lying to sitting or standing), which can lead to fainting.
The reason for a significant decrease in blood pressure may be a decrease in BCC (circulating blood volume) due to internal bleeding, for example, with ulcers or cancer. This means that pressure of 120 over 100 cannot be ignored. What to do with such blood pressure values - you should consult a therapist or cardiologist.
The first signs of a stroke
Diagnostics and methods of correction
What to do if you suspect isolated diastolic hypertension? First of all, visit a specialist and undergo an examination. It includes the following methods of studying the body:
- Ultrasound of the heart, kidneys and thyroid gland;
- Dopplerography of cerebral vessels;
- ECG;
- laboratory blood tests for biochemistry.
If the presence of tumors in the kidneys is suspected, magnetic resonance imaging is performed. To identify problems with the endocrine system, it is recommended to donate blood for hormones, this is especially important for women during pregnancy and menopause. The goal of treatment is not to correct the condition when low blood pressure regularly increases, but to eliminate the cause.
Usually, after the underlying disease is cured, be it a pathology of the thyroid gland or the renal system, the pressure stabilizes on its own. What can you do if your blood pressure increases again? It is not recommended to take antihypertensive drugs on your own, because in this case both the lower and upper levels will drop at the same time.
Only the doctor decides whether there is a need to take medications and how to combine drugs with each other in order to maintain both tonometer indicators normal.
Among the drugs intended for the correction of isolated diastolic hypertension are:
- Diuretics are necessary to remove excess fluid from the body and eliminate swelling, which are always present in the complex therapy of hypertension. These are Veroshpiron, Triamterene, Furosemide, Hypothiazide.
- Alpha blockers are well tolerated and help stabilize blood pressure. These include Terazosin and Prazosin.
- Beta-blockers - stabilize the functioning of the heart muscle, reducing the number of contractions and affecting the nerve centers. The heart begins to function in an economical mode, and the pressure is restored. This group includes Bisoprolol, Atenolol, Metoprolol.
- ACE inhibitors – inhibit the production of angiotensin, a substance that increases blood pressure. This group includes the drugs Captopril, Fosinopril, Enalapril and their derivatives.
- Calcium antagonists - expand the lumens of the capillaries, due to which the pressure stabilizes. Verapamil and Nifedipine tablets are effective.
Therapy also includes taking sedatives if pressure surges are provoked by nervous tension and stress. The patient is prescribed herbal remedies - tincture of peony, motherwort, valerian, drugs Glycine, Nervohel, Valocordin, Corvalol, Persen.
What to do immediately?
If a visit to a doctor is not possible in the near future, and a person has a high pulse and blood pressure of 120 over 100, what should be done immediately to provide first aid?
Since an increased pulse poses a threat to the heart muscle and heart activity in general, it is advisable to first lower the pulse so as not to provoke the development of arrhythmia (atrial fibrillation).
To this end, the patient should:
- provide peace;
- free him from tight clothes;
- provide access to fresh air;
- You can wipe the patient's face and chest with a cool, damp towel.
The complexity of the situation lies in the fact that with reduced (for hypertensive) systolic pressure, diastolic blood pressure and pulse remain high. This means that any drugs containing caffeine benzoate will only aggravate the situation if they are used as “symptomatic therapy” - for example, to eliminate a headache. In this case, what to do if the pressure is 120 over 100, and the person clearly needs help?
If the patient's skin turns pale, chills are felt, dizziness and other obvious symptoms occur that indicate a further decrease in blood pressure, it is necessary to call an ambulance.
Is it possible to lower the lower indicator yourself?
No, you can’t do anything on your own. A selective influence specifically on diastolic pressure is necessary. Only a complex of antihypertensive drugs can help; in what combinations and dosages, the doctor will have to find out.
In general, even a cardiologist can do little at home. Hospitalization and selection of a therapeutic course under the supervision of a group of specialists are required.
Everything may take from 2 weeks to a month or a little more. As a rule, the main measures are carried out in the first 7 days, then the patient can go home. Other measures are taken during a systematic visit to the doctor.
Therefore, there is no need to be afraid of hospitalization. No one is kept in the hospital for a long time: it is not economically profitable and inappropriate in choosing therapy.
In case of further increase in lower pressure while the upper pressure remains unchanged, you should call an ambulance.
Attention:
Amateur activities are excluded. Incorrectly selected medications can provoke a sharp jump in blood pressure with disastrous results.
What medications can help?
If it is unknown for what reasons the pressure dropped to 120/100 and what this means, no matter what medications, the names of which are even well known to hypertensive patients, are taken, they cannot solve the problem of an impending cardiac or cerebral catastrophe. Here, a significant correction of the treatment received by the patient is necessary, which means the assistance of the attending physician. The only thing that can urgently help a patient if he feels unwell is to give him any sedative:
- Valocordin;
- Corvalol;
- tincture of motherwort or valerian.
Of course, a person in such a state must be protected from any unnecessary emotions and experiences, which means trying to calm him down, promising that a doctor will come and definitely help.
Examinations that need to be completed
Patients of this kind are managed by a cardiologist. If necessary, doctors of other profiles are involved: endocrinologist, neurologist and nephrologist. In tandem, they carry out diagnostic activities, each within the scope of their competence.
The general scheme looks like this:
- Anamnesis collection and oral assessment of patient complaints. Objectification of symptoms plays the greatest role; it is a kind of vector that guides doctors in the right direction.
- Blood pressure measurement. Using simple calculations, you can calculate the PD and determine how much it deviates from the norm.
- Daily monitoring. The change may be temporary, but if the process lasts more than 8 hours or almost a full day, there is no doubt about the pathogenicity of the origin.
- Heart rate assessment.
- Palpation of the kidneys. Possible only in thin patients.
- Ultrasound of internal organs.
- Blood tests (general, biochemistry, hormones of the adrenal cortex, pituitary gland, thyroid gland), urine (according to Zimnitsky, clinical).
- Electrocardiography, possibly with stress tests.
- Echocardiography.
- Study of brain rhythms. Encephalography.
Complexity is the key to early verification of the diagnosis, and therefore the determination of therapeutic tactics.
Symptoms
Ignoring the symptoms of high blood pressure can be very dangerous. Main features:
- heart rhythm pathologies, increased heart rate (pulse exceeds 100);
- difficulty breathing;
- dizziness;
- temperature changes (suddenly throws you into the heat, then into the cold);
- intense headache;
- weakness;
- fatigue;
- nosebleeds;
- blurred vision;
- nausea.