Why does pericarditis occur?
The following are the main causes of pericarditis:
- Infectious agents: viruses, bacteria, fungi and even parasites. The inflammatory process in the pericardium is triggered by the influence of exo- and endotoxins released by microorganisms.
- Autoimmune connective tissue diseases such as lupus erythematosus or scleroderma. At the same time, the body synthesizes antibodies to its own cells, which damage connective tissue and cause systemic inflammation.
- Heart diseases. The result of serious damage to the heart muscle is the spread of the pathological process to the surrounding pericardium. This can occur with transmural myocardial infarction, infectious or reactive myocarditis.
- Damage to other organs, such as the kidneys, can lead to pericarditis. In cases of serious impairment of excretory function and the formation of renal failure, deposition of metabolic products in the serous cavities, including the pleura and pericardium, is observed.
- Penetrating pericardial injuries that disrupt the integrity of the pericardial layers.
- Metastatic tumors that cause pericardial carcinomatosis.
- The causes of pericarditis are varied, and, therefore, treatment approaches depend on what caused the inflammation. But in the absence of timely diagnosis and correction of this condition, the outcome is always the same. The result of chronic pericarditis is cardiac tamponade, which leads to the death of the patient.
At CELT you can consult a cardiologist.
- Initial consultation – 3,500
- Repeated consultation – 2,300
Make an appointment
Prevention
There are two types of preventive measures:
- Primary. It is aimed at comprehensively strengthening the immune system by maintaining a healthy and active lifestyle, hardening procedures and timely treatment of foci of infection (caries, sinusitis, and so on).
- Secondary. After completing the course of treatment and discharge, the patient is registered with a dispensary for constant monitoring and prevention of relapses. A change in work regime is necessary, since a person needs to work in a comfortable environment with a minimum amount of physical activity.
What are the types of pericarditis?
According to the pathophysiological mechanism, pericarditis is divided into:
- exudative pericarditis (when inflammatory fluid accumulates in the cavity - exudate);
- adhesive pericarditis (when “dry” inflammation predominates and adhesions form);
- constrictive pericarditis (when compression of the heart occurs and calcification of the pericardial walls).
This division is very arbitrary, because at different stages of the pathological process the type of inflammation can transform. And the formation of areas of calcification is the outcome of any pericarditis in the absence of adequate therapy.
Symptoms of pericarditis
The onset of pericarditis, symptoms and first signs are quite characteristic. The main reason to see a doctor is chest pain. The pain syndrome in this disease can be quite pronounced and persistent. But there are times when fever comes first in severity. Its combination with shortness of breath and chest pain is often mistaken for pneumonia.
The pain syndrome in this cardiac pathology can radiate, as with angina pectoris, to the left arm and shoulder blade. But the hallmark of pain with pericarditis is the lack of connection with physical activity. The pain is almost constant and intensifies when changing body position or taking a deep breath.
In addition to pain, pericarditis is always accompanied by additional symptoms: general weakness, increased body temperature, shortness of breath with little physical exertion, interruptions in heart function, and decreased blood pressure. Unlike angina, nitrate-based medications do not provide relief.
If you notice similar symptoms in yourself or your loved ones, you need to urgently consult a doctor, because the price of delay can be human life. Only a professional cardiologist, having examined the patient and prescribed an immediate instrumental examination, will be able to accurately diagnose and recommend adequate treatment.
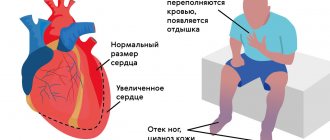
Otherwise, if medications are not prescribed in a timely manner, a terrible complication inevitably arises - cardiac tamponade. With tamponade, a large amount of exudate accumulates in the pericardial cavity. The consequence is that the heart muscle is literally compressed and cannot fully contract.
The result of such compression is acute cardiovascular failure, cardiac arrest and death of the patient. In this case, the usual methods of resuscitation rarely have a positive effect, and only the release of the pericardium from the excess amount of exudative fluid can make the heart beat again.
Inflammatory heart diseases
Infections and the heart Tamara Dmitrievna Tyabut, Professor of the Department of Cardiology and Rheumatology of Bel MAPO, Doctor of Medical Sciences
Year of Health.
Read it and pass it on to someone else Among the diverse pathologies of the heart, a considerable share is occupied by diseases that arise as a result of the negative impact of infectious agents on the heart. Infectious agents are a huge number of microorganisms found in the world around us. These include bacteria, spirochetes, rickettsia, protozoa, pathogenic fungi, and viruses. If in the last century the culprits of heart damage were mainly bacteria, then in recent years the importance of viral infections has increased. Infectious agents can have a direct damaging effect on the heart muscle - the myocardium, or cause certain negative changes in the immune system, which leads to disruption of its functions. The immune system is a set of cells, organs and tissues that carry out immune reactions, the main purpose of which is to protect the human body from the negative effects of environmental factors. Protection is carried out by recognizing foreign cells or substances that have entered the human body, neutralizing them or removing them from the body. The functions of the immune system are regulated by the nervous and endocrine systems. The variety of powerful stressors that accompany the life of a modern person leads to disruption of the functions of the immune system, and, consequently, weakens its protection from the effects of infectious agents. Therefore, quite often, infectious lesions of the heart occur against the background of excessive stress, mental trauma, negative events in a person’s life (conflict at work or in the family, illness of loved ones, job loss, divorce, death of a loved one, etc.). The body's protection from infections - bacterial, viral, fungal or parasitic - is carried out by two immune systems: innate, determined by genetic factors transmitted from parents, and acquired, formed during a person’s life. There are natural and artificial immunity. Natural immunity is formed as a result of the transfer from mother to fetus through the placenta or with milk of ready-made protective factors, as well as as a result of contact with a pathogen (after a previous illness or after latent contact without the appearance of symptoms of the disease). Prevention of infectious lesions begins with the conception of a child and continues after his birth - a healthy mother and breastfeeding are the best methods of prevention at this stage of a person’s life. After the birth of a child, artificial immunity, which is formed during preventive vaccinations, is also included in the protection. Compliance with the vaccination calendar is the basis of prevention in subsequent stages of a person’s life. Currently, vaccinations are carried out against the most common and severe infections, but there are a huge number of other microorganisms that have a damaging effect on the human body in general and the heart in particular. Winter has come, and with its arrival the number of colds increases. The most common colds include acute tonsillitis (tonsillitis), exacerbations of chronic tonsillitis, and pharyngitis. Tonsillitis is an inflammation of the pharyngeal tonsils, which belong to the secondary organs of the immune system. The cause of both acute and chronic tonsillitis is pathogenic microorganisms (bacteria, viruses and fungi), which, penetrating into the tonsil tissue, cause an inflammatory process and can have a general negative effect on the body in the form of intoxication. Acute and chronic processes in the tonsils occur differently. Manifestations of sore throat include severe pain in the throat when swallowing, enlargement of the submandibular and cervical lymph nodes, fever up to 39-40 degrees, headaches and muscle pain, and general weakness associated with intoxication. These symptoms require mandatory, early consultation with a doctor. Chronic tonsillitis and its exacerbations can be manifested by a slight increase in temperature, especially in the evening, a sore throat or slight sore throat, combined with increased fatigue, morning weakness, restless sleep, and loss of appetite, which ultimately reduces a person’s ability to work. This condition is called tonsillogenic intoxication. Very often, a patient, having been to see many specialists, leaves them without answering the question: “Why does he have an elevated temperature?” But the whole point is only in chronic inflammation of the tonsils, with the treatment of which these symptoms disappear. Many people endure exacerbations of tonsillitis “on their feet” and do not attach importance to its symptoms. And later they pay for it with the development of complications. There are several reasons for the occurrence of tonsillitis - structural features of the tonsils, impaired immunity, unfavorable environmental factors - hypothermia, viral colds. Among the factors that cause exacerbation of tonsillitis, there are social ones - poor quality nutrition, unfavorable environmental conditions, maximum employment in the workplace, stress, working conditions, living conditions, smoking, and medical - diseases of the ENT organs - pathology of the paranasal sinuses, individual structural features of the ENT organs (deviated nasal septum, enlarged nasal turbinates, diseases of the nasopharynx (adenoids, polyps), frequent respiratory diseases, as well as dental caries. Chronic inflammation in the tonsils can be promoted by immunodeficiency conditions, other diseases of the internal organs, concomitant endocrine pathology. With chronic tonsillitis in the tonsils You can detect up to several dozen (usually about 30) types of microorganisms - fungi and bacteria, but the main cause of the disease is streptococcus.
Tonsillitis caused by beta-hemolytic streptococcus.
In the presence of chronic tonsillitis, a large amount of pus accumulates in the lacunae, consisting of dead microbes, white blood cells - leukocytes, and other cells (purulent-caseous plugs). Pathogenic microbes multiply in the purulent contents of the lacunae. The waste products of microbes from the tonsils enter the blood and lead to the development of tonsillogenic intoxication, manifested by fatigue, muscle and joint pain, headaches, decreased mood, and low-grade fever. Tonsils turn into a repository of infectious agents, from where they can spread throughout the body and cause inflammatory processes. Frequent illnesses further weaken the immune system, which leads to further development of tonsillitis. This is how a vicious circle of disease is formed. Chronic tonsillitis is dangerous due to complications associated with the spread of infection throughout the body. These include peritonsillar abscesses, damage to the heart (tonsilogenic myocardial dystrophy, acute rheumatic fever), blood vessels, and kidneys. Tonsillogenic myocardial dystrophy refers to frequently developing, but much less frequently diagnosed lesions of the heart muscle in chronic tonsillitis. It is caused by toxins from bacteria found in the tonsils and products of local inflammation and tissue breakdown. Clinical signs of tonsillogenic myocardial dystrophy are caused by disruption of the autonomic nervous system (vegetative dysfunction) and disruption of various types of metabolism in the heart muscle (electrolyte, protein), which results in disruption of energy production in the heart muscle. In the early stages of development, tonsilogenic myocardial dystrophy is manifested by a high heart rate - tachycardia, interruptions in heart function - extrasystole, shortness of breath during intense physical exertion, and a disturbance in the general well-being of patients. With late diagnosis, signs of heart failure appear, the volume of exercise causing shortness of breath decreases, and more severe rhythm and conduction disturbances appear. With timely diagnosis and treatment of the extracardiac factor - chronic tonsillitis, which caused the listed changes in the heart muscle, they are reversible and the structure and functions of the heart muscle are gradually restored. The greatest danger to the prognosis and quality of life of patients is cardiac damage in acute rheumatic fever. Acute rheumatic fever (ARF) is a post-infectious complication of tonsillitis (tonsillitis) or pharyngitis caused by group A beta-hemolytic streptococcus, in the form of a systemic inflammatory disease of connective tissue with a predominant localization of the pathological process in the cardiovascular system (carditis), joints (migratory polyarthritis) , brain (chorea) and skin (ring-shaped erythema, rheumatic nodules), developing in predisposed individuals, mainly young people (7-15 years). In the Russian Federation and the Republic of Belarus, the incidence of rheumatic fever ranges from 0.2 to 0.6 cases per 1000 children. The primary incidence of ARF in Russia at the beginning of the 21st century was 0.027 cases per 1000 population. The frequency of newly diagnosed chronic rheumatic heart disease (CRHD), which includes heart defects and specific changes in valves (marginal fibrosis), detected by ultrasound examination of the heart, is 0.097 cases per 1000 population, including rheumatic heart disease - 0.076 cases per 1000 adult population. The existing statistical differences between the incidence of primary incidence of acute rheumatic fever and chronic rheumatic heart disease indicate the presence of a large number of undiagnosed acute forms of the disease. The time interval between acute streptococcal tonsillitis, pharyngitis, exacerbation of chronic tonsillitis and the onset of acute rheumatic fever is 3-4 weeks. In acute rheumatic fever, all structures of the heart can be affected - endocardium, myocardium, pericardium. Damage to the myocardium (heart muscle) always occurs. Manifestations of heart damage may include palpitations, shortness of breath associated with physical activity or at rest, aching pain in the heart area, which, unlike angina, does not have a clear connection with physical activity and can persist for a long period of time, palpitations, interruptions in heart function, paroxysmal rhythm disturbances - atrial fibrillation, atrial flutter. Usually, heart damage is combined with a joint syndrome such as arthralgia - pain in large joints (knees, shoulders, ankles, elbows) or arthritis (inflammation) of the same joints. Inflammation of the joints is characterized by pain, changes in the shape of the joint caused by swelling, redness of the skin in the area of the affected joint, a local increase in temperature and dysfunction of the joint in the form of limited range of motion. Small joints are affected much less frequently. The inflammatory process in the joints is migratory in nature and quickly resolves with proper treatment. Damage to the heart and joints is usually accompanied by fever, weakness, sweating, and disability. Some patients experience lesions of the nervous system, skin rashes such as erythema annulare and subcutaneous rheumatic nodules. To make a diagnosis of acute rheumatic fever, there are diagnostic criteria that include clinical, laboratory and instrumental data, as well as information about past infection caused by group A beta-hemolytic streptococcus and its rheumatogenous strains. A timely diagnosis allows the patient to recover when treated with antibiotics, glucocorticoid hormones, and non-steroidal anti-inflammatory drugs. However, if treatment is started late, patients do not comply with the motor regimen, the presence of a genetic predisposition, or unsanitized focal infection (decompensated tonsillitis, caries), the outcome of acute rheumatic fever can be chronic rheumatic heart disease with or without heart disease. Heart disease occurs as a result of inflammatory damage to the heart valves. The presence of a heart defect of rheumatic etiology requires the patient to be classified as at high risk of developing infective endocarditis, the most severe form of heart damage associated with infectious agents. Acute rheumatic fever is a disease in which prevention is important to reduce both the initial incidence and repeated episodes of the disease (recurrent acute rheumatic fever). Primary prevention is aimed at reducing primary morbidity and includes a set of medical, sanitary and hygienic measures, as well as adequate treatment of infections caused by group A beta-hemolytic streptococcus. The first direction includes hardening measures, familiarization with hygienic skills, sanitation of chronic foci of infection, primarily chronic tonsillitis and caries. The tonsils are thoroughly sanitized by repeated rinsing and washing with solutions of antibacterial agents, and vacuum aspiration of the pathological contents of the lacunae. If this does not give the desired result, the issue of surgical treatment is discussed - removal of the tonsils. In each specific case, the choice of treatment tactics is determined by an otolaryngologist and therapist, cardiologist or rheumatologist. Adequate treatment of sore throat and pharyngitis is aimed at suppressing the growth and reproduction of streptococcus in the body during the development of streptococcal pharyngitis, sore throat, and tonsillitis. The basis of treatment is antibiotic therapy in combination with anti-inflammatory drugs, which must be carried out for at least 10 days with mandatory monitoring of a general blood test, urine test, and, according to indications of a biochemical blood test, when signs of the disease occur, at the end of treatment and a month after the appearance of the first signs of the disease. Laboratory research carried out within these periods allows you to make a correct diagnosis, determine the effectiveness of treatment, and, most importantly, not to miss the onset of the development of complications in the form of acute rheumatic fever. Secondary prevention aims to prevent the development of recurrent acute rheumatic fever and progression of the disease in people who have had ARF. It is performed in patients who are not allergic to penicillin drugs. The drug used for prophylaxis in adults is benzathine benzylpenicillin (extencillin, retarpen) at a dose of 2,400,000 units once every 3 weeks intramuscularly. Prophylactic regimens depend on the age of the patient and the outcome of acute rheumatic fever. In accordance with the recommendations of the Association of Rheumatologists of Russia, secondary prevention includes the following regimens:
- For patients who have had ARF without carditis (arthritis, chorea) - at least 5 years after the attack or up to 18 years (based on the “whichever is longer” principle).
- For patients with cured carditis without heart disease - at least 10 years after the attack or up to 25 years (based on the “whichever is longer” principle).
- For patients with a formed heart defect (including operated ones) - for life.
The most severe and prognostically unfavorable heart disease associated with infection is infective endocarditis - a disease characterized by the development of an inflammatory process on the valvular or parietal endocardium, including damage to large intrathoracic vessels extending from the heart, resulting from exposure to a microbial infection. Most often these are various bacteria - streptococci, staphylococci, enterococci, Escherichia coli, Pseudomonas aeruginosa and many others. 119 different pathogens leading to the development of the disease have been described.
Aortic valve
Mitral valve
This is what heart valves look like during the development of infective endocarditis. Overlays of microbes and blood cells disrupt their function, destroy the valve and often require emergency surgical treatment.
The prevalence of infective endocarditis at the beginning of the 21st century was 2-4 cases per 100,000 population per year. There is a widespread increase in incidence, most pronounced in older age groups and amounting to 14.5 cases per 100,000 population aged 70-80 years. Diagnosis of the disease is difficult. At the first visit to a doctor, the diagnosis is made only in 19 - 34.2% of patients. The average time from initial treatment to diagnosis is at least 1.5 - 2 months.
There is a group of patients at high risk of developing infective endocarditis, which includes:
- patients with previous infective endocarditis,
- patients with prosthetic heart valves,
- patients with blue congenital defects,
- patients after surgical operations on the aorta, pulmonary vessels
- patients with acquired heart defects, primarily of rheumatic etiology (CRHD).
In addition, a moderate (intermediate) risk group has been identified, which includes patients with the following diseases:
- Mitral valve prolapse due to myxomatous degeneration or other causes with grade 2-3 regurgitation or prolapse of several valves
- Non-cyanotic congenital heart defects (excluding secondary ASD)
- Bicuspid (two-leaf) aortic valve
- Hypertrophic cardiomyopathy (idiopathic hypertrophic subaortic stenosis).
It has been established that for the development of infective endocarditis, the pathogen must enter the blood. The most common cause of this may be dental procedures, accompanied by gum damage and bleeding. In the presence of caries or gum disease, bacteremia (the presence of a pathogen in the blood) can occur quite often.
| Type of manipulation | Frequency of bacteremia |
| Tooth extraction | 61-85%, |
| Preventive dental treatment | 0-28%, |
| Teeth cleaning | 0-26%, |
Depending on the initial state of the heart and endocardium, the disease can occur in two ways.
Primary IE (30% of cases) occurs on the unaffected endocardium under the influence of severe infections (staphylococci, gram-negative microorganisms, fungi). Secondary IE (70% of cases) develops on valves or endocardium that are changed due to congenital or acquired heart defects. Diagnosis of infective endocarditis is difficult due to the fact that in the early stages there are no specific signs of the disease. Nonspecific symptoms include fever, general malaise, weight loss, and decreased ability to work. Signs of heart damage appear at 3-4 weeks of illness. Before this, the disease can masquerade as kidney disease, lung disease, stroke, thromboembolism in various internal organs, worsening chronic heart failure. Prevention of infectious endocarditis may lead to a reduction in morbidity. According to researchers from France, per 1,500 patients receiving antibiotic prophylaxis, 60 to 120 cases of infective endocarditis are prevented. The economic costs of preventing infective endocarditis are significantly less than those of treating it. Manipulations that can cause bacteremia and in which antibiotic prophylaxis should be carried out include:
- Bronchoscopy.
- Cystoscopy during urinary tract infection.
- Biopsy of the urinary organs or prostate gland.
- Dental procedures with a risk of damaging the gums or mucous membranes.
- Tonsillectomy, adenoidectomy.
- Esophageal dilatation or sclerotherapy for esophageal varicose veins.
- Interventions for biliary obstruction.
- Transurethral resection of the prostate gland.
- Instrumental dilatation of the urethra.
- Lithotripsy (crushing stones).
- Gynecological interventions in the presence of infection.
Active participants in the organization and implementation of the prevention of infective endocarditis should be not only doctors, but also patients themselves.
Not even the most competent and knowledgeable doctor will be able to implement a prevention program without the desire and understanding of the importance of prevention on the part of the patient himself. “If someone is looking for health, ask him first if he is ready to part with all the causes of his illness in the future - only then will you be able to help him.” Socrates
This is the meaning of prevention, both non-pharmacological, which is based on the correction of many behavioral risk factors, and medicinal. Knowing when to carry out prevention, you should also know how to carry it out. The choice of prevention method is based on 3 principles. The first principle is to determine which group you belong to - high or intermediate risk. The second principle is to assess the tolerability of antibacterial drugs - have any allergic reactions to penicillin drugs (penicillin, bicillin, ampicillin, amoxicillin, oxacillin, and others) have ever been recorded? The third principle is before which procedure a prophylactic administration of an antibacterial drug is carried out. When performing dental procedures or diagnostic and therapeutic manipulations on the respiratory tract and esophagus, the following preventive regimens are recommended: For patients of all groups without allergies to penicillin drugs:
- Amoxicillin in a dose of 2.0 grams orally 1 hour before the procedure.
- In case of problems with oral administration, ampicillin or amoxicillin at a dose of 2 grams intravenously 30-60 minutes before the procedure.
For patients with allergies to penicillin drugs:
- Clindamycin 600 mg or
- Azithromycin 500 mg or
- Clarithromycin 500 mg orally 1 hour before the procedure
When performing manipulations on the organs of the genitourinary and gastrointestinal tract, the following preventive regimens are used:
- For persons who are not allergic to penicillin drugs: High-risk group - ampicillin or amoxicillin at a dose of 2 g intravenously and gentamicin at a rate of 1.5 mg/kg body weight intravenously 30-60 minutes before the procedure. After 6 hours, ampicillin or amoxicillin is taken orally at a dose of 1 gram.
Intermediate risk group
- Ampicillin (amoxicillin) 2.0 g intravenously 30-60 minutes before the procedure or amoxicillin 2.0 g orally 1 hour before the procedure
- For persons who are allergic to penicillin drugs:
High-risk group
- vancomycin 1.0 grams intravenously 1 hour before the procedure in combination with intravenous or intramuscular administration of gentamicin at the rate of 1.5 mg/kg body weight.
Intermediate risk group
— vancomycin 1.0 grams intravenously 1 hour before the procedure
The presented preventive programs for patients with acute rheumatic fever and infective endocarditis are not a prescription for purchase or a direction for administering the drug. All preventive regimens should be discussed with the attending physician - internist, cardiologist, rheumatologist. But without the knowledge of the patient himself, his awareness of the essence and significance of primary and secondary prevention of any disease, including infectious heart lesions, it is impossible to carry out preventive measures to maintain the high quality of his life. But it is prevention of both the disease itself and its complications that plays the most significant role. It is easier to prevent any disease than to treat it.
The importance of interaction between doctor and patient was recognized by ancient healers. Hippocrates wrote: “Life is short, the path of art is long, opportunity is fleeting, experience is unreliable, judgment is difficult. Therefore, not only the doctor himself must be ready to do everything that is required of him, but also the patient, those around him, and all external circumstances must contribute to the doctor in his activities. And the Chinese healer Lao-Jun writes about prevention: “If you want to save yourself from a disaster or solve a problem, then it is best to prevent their occurrence in your life in advance. And then there will be no difficulties. In order to cure an illness, get rid of a disease, it is best to be prepared for them ahead of time. Then there will be a happy outcome. Currently, people do not pay attention to this and do not try to prevent it, but direct their energy to escape. They do not try to prepare ahead of time, but try to cure themselves with the help of medications. Therefore, there are sovereigns who are not capable of guarding the sacrificial altar of state power. There are also organisms that are not able to maintain themselves intact over a long life. Thus, a man of wisdom achieves happiness when there are no omens. He gets rid of trouble before it has yet appeared. After all, disaster is born from little things, and illness arises from the subtlest deviations. People believe that a little goodness does not bring any benefit, and therefore they do not want to do goodness. It seems to them that there will be no damage from a small evil, and therefore they do not strive to improve. If you do not accumulate goodness little by little, then you will not get great Potency. If you do not abstain from evil in small things, then a big crime will be committed. Therefore, we will choose the most important thing to show how it is born.”
Treatment of pericarditis
The following groups of drugs are used in the treatment of pericarditis:
- Non-steroidal anti-inflammatory drugs that relieve the symptoms of inflammation.
- Antibiotics, antiviral, antifungal and antiparasitic drugs, if the etiological factor is an infectious agent.
- Glucocorticosteroids and cytostatics, if the cause of pericarditis is an autoimmune pathology.
- Treatment of the underlying disease that caused pericarditis - in case of renal failure, hemodialysis can be used, and in case of myocardial infarction - thrombolysis and restoration of blood flow through the coronary arteries.
- If there is a threat of developing cardiac tamponade, they resort to puncture of the pericardial cavity. The purpose of this manipulation is to remove fluid and prevent tamponade. But this puncture is no less important in diagnostic terms. The resulting exudate is subjected to microscopy, bacteriological and cytological examination. It can contain atypical tumor cells or an infectious pathogen.
The prognosis for pericarditis is generally favorable. If pericarditis is correctly diagnosed and treatment is started on time, then a complication in the form of tamponade is extremely unlikely. But it is worth remembering that pericarditis, the treatment of which requires a professional approach, is a rather formidable disease with dangerous complications.
By contacting CELT cardiologists, you can be absolutely sure of timely diagnosis and correct treatment tactics for any cardiac pathology. After all, we employ specialists of the highest category with extensive practical experience. Another argument in favor of CELT is that our clinic has the technical capabilities for a full and comprehensive examination.
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions