Thalassemia (Cooley's anemia) is a hereditary disease in which the synthesis (production) of hemoglobin is impaired. Genetic pathology is more common among the peoples of Asia, the Near and Middle East, and African Americans; rare cases of the disease are registered in Russia in the Volga region. Clinical manifestations are varied and depend on the form of thalassemia. Sometimes the disease is diagnosed in the first days of life, in other cases it remains asymptomatic for a long time. Patients with mild forms live full lives and do not need drug therapy.
Classification
Thalassemia is classified according to the severity of the disease, mode of inheritance, and type of genetic defect. A detailed classification with explanations is presented in the table below.
| Classification sign | Form of the disease | Comments |
| Type of mutation | alpha thalassemia | associated with mutations in the HBA1 and HBA2 genes; with disturbances in one gene it is asymptomatic, changes in two or three genes cause chronic anemia, mutations in four genes are incompatible with life |
| beta thalassemia | distinguish beta thalassemia major and minor; the small form does not manifest itself in any way, the large form is characterized by a severe course | |
| Inheritance type | heterozygous | develops when inheriting one altered gene |
| homozygous | develops as a result of a mutation in both parents | |
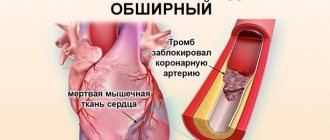
| Severity of the disease | mild moderate severe | the severity of the disease depends on the number of mutated genes; in mild forms there are no symptoms, severe forms are often complicated by circulatory disorders and lead to the development of cardiovascular diseases |
Thalassemia is more common in regions where malaria is common. Researchers attribute this to the fact that carriers of this type of mutation in genes are more resistant to malarial plasmodium.
Frequency of occurrence
Thalassemia is inherited in an autosomal recessive manner. This means that it affects both boys and girls equally. The recessive nature suggests that children with thalassemia appear in those families where mom and dad are both carriers of mutations. Although they may not even realize that they are carriers, since the symptoms are sometimes invisible.
The average incidence is 1 in 100,000 people and may vary by region. Beta thalassemia is more common than alpha thalassemia.
Causes of the disease
The cause of the development of the disease is a mutation in the gene, which carries information about the synthesis of globin chains - a protein involved in the formation of hemoglobin. As a result, its production (production) stops or occurs in smaller quantities, blood cells are destroyed, and anemia develops. The homozygous form of thalassemia is characterized by the presence of two defective genes that are inherited from both parents. With the heterozygous variant, a person becomes a carrier of an altered gene inherited from one of the parents.
Pathogenesis
The molecular basis of the pathogenesis of thalassemia is a genetic defect, which consists in the fact that in the cells of some patients abnormal RNA (ribonucleic acid, involved in coding, reading and regulation of genes) functions, while in others there is a deletion of genetic material (a change in the structure of chromosomes). As a result, the synthesis of one of the hemoglobin chains decreases or stops. Normally, the synthesis of hemoglobin chains is balanced, and the number of alpha and non-alpha chains is equal. A change in the synthesis of one of them leads to an imbalance. Thus, a lack of beta chains while maintaining the production of alpha chains leads to an excess of free alpha chains, and vice versa.
Epidemiology[edit]
Malaria
The worldwide distribution of hereditary alpha thalassemia follows areas of malaria infection, suggesting its protective role. Thus, alpha thalassemia is common in sub-Saharan Africa, the Mediterranean basin, and generally in tropical (and subtropical) regions. The epidemiology of alpha thalassemia in the United States reflects this global pattern of distribution. In particular, HbH disease is seen in Southeast Asia and the Middle East, while Hb Bart hydrops fetalis is found only in Southeast Asia. [21] Data show that 15% of Greek and Turkish Cypriots carry beta thalassemia genes, and 10% of the population carry alpha thalassemia genes. [22]
Symptoms of Thalassemia
The clinical picture of thalassemia depends on the form of the disease. However, most patients have the following symptoms:
- delayed growth and development;
- change in skin color (pallor, yellowness, darkening);
- tendency to fractures due to thinning bones;
- skeletal deformities;
- enlarged liver and spleen;
- stones in the bile ducts.
In severe beta thalassemia, clinical manifestations are noticeable within the first year of a child’s life. Characteristic signs of this form of the disease:
- Mongoloid face (flattened bridge of the nose, narrowing of the palpebral fissures);
- altered head shape (“tower skull”);
- enlarged upper jaw;
- malocclusion.
Beta thalassemia minor is asymptomatic and is detected using laboratory diagnostic methods.
Note! Thalassemia can lead to mental and physical underdevelopment of the child, so the disease cannot be ignored. If you suspect a genetic pathology, you must undergo an examination and, if the diagnosis is confirmed, begin treatment.
Diagnosis of the disease
Pathology can be suspected in children with characteristic clinical signs in whose family cases of thalassemia have been identified. Patients with a suspected genetic mutation should visit a hematologist (blood disease specialist) and a medical geneticist. Laboratory diagnostics will help confirm or refute the diagnosis:
- Typical signs of thalassemia in a blood test are a decrease in hemoglobin levels and color index, the presence of red blood cells of an altered shape, an increase in iron and indirect bilirubin.
- When examining bone marrow substances, hyperplasia (proliferation) of the red hematopoietic lineage with a high number of erythroblasts and normoblasts (immature blood cells) is detected.
- Molecular genetic studies can identify a mutation in alpha or beta globin that disrupts the synthesis of globin protein chains.
- An ultrasound examination of the abdominal cavity reveals an enlarged liver and spleen, and stones in the gall bladder.
Differential diagnosis of the disease is carried out with iron deficiency, autoimmune, sickle cell and other types of anemia.
What are the prospects for Zinteglo?
Since Zinteglo is conditionally approved (without strict requirements, as in the case of other drugs), Bluebird is required to annually send updated clinical data to the regulator so that it renews the registration of the drug, based on the fact that the benefits outweigh the harm. As soon as the data is collected into a pool of the required volume, it will be possible to talk about a full-fledged marketing permit.
In the future, patients with a genotype characterized by a complete absence or critically low endogenous synthesis of beta-globin will be added to the spectrum of patients for whom Zynteglo gene therapy is indicated: for example, β0/β0, mutations IVS-I-110 or IVS-I-5. The effectiveness of treatment in such patients may be less clear: clinical trials of HGB-212 are testing this.
This year, Bluebird intends to submit a registration dossier for Zinteglo to the US Food and Drug Administration (FDA), with a launch expected in 2020.
Along the way, Bluebird is completing a test of Zynteglo in the gene therapy treatment of sickle cell anemia, since this pathology is caused by other mutations of the same beta-globin gene.
The estimated European population of patients with transfusion-dependent beta thalassemia is 11–13 thousand people, with half living in Italy. Commercial prospects in the United States are much more modest with a patient pool of 1,400–1,500 people. Taking into account the upcoming inclusion of sickle cell anemia, it is quite possible for Zinteglo to earn bestseller status, crossing the threshold of $1 billion in annual sales.
In terms of competition, luspatercept will see the light of day in the foreseeable future: the FDA will decide on its approval for transfusion-dependent beta thalassemia by early December. Luspatercept, being developed by Acceleron Pharma and Celgene, is an erythrocyte maturation activator. This soluble fusion protein, comprising a modified extracellular domain of activin receptor type IIB (ActRIIB) and the Fc domain of human immunoglobulin IgG1, targets specific ligands of the transforming growth factor beta (TGF-β) superfamily that regulate late-stage erythropoiesis. Luspatercept is thought to act as a ligand decoy that inhibits abnormal Smad2/3 signaling responsible for ineffective erythropoiesis.
Treatment of thalassemia
Treatment for thalassemia depends on the form of the disease. Patients with beta thalassemia minor do not require drug therapy other than taking B vitamins and folic acid. Patients with homozygous beta thalassemia from the first days of life are recommended to undergo blood transfusion therapy (transfusion of red blood cells), the introduction of chelating drugs (to bind iron), and hormones in case of a sharp deterioration of the condition. In severe cases, bone marrow transplantation is indicated for patients with thalassemia.
How much does Zinteglo cost?
PS Bluebird put the cost of Zinteglo at 1.575 million euros ($1.77 million). As expected, payment will be made in installments over five years in equal installments: first an advance, and then annual payments, but only if the effectiveness of treatment is recorded.
Bluebird has not yet determined the final cost of its gene therapy, but it will obviously be prohibitive. It is clear that in highly developed countries with medical insurance, none of the patients pays the entire amount out of their own pocket.
Yes, according to Bluebird's calculations, the "fair price" of Zinteglo, calculated taking into account the improvement in the patient's quality and life expectancy, is within $2.1 million, but the final cost is expected to be significantly less. This astronomical amount obviously comes from the total costs of the health care system for many years of chronic therapy for beta thalassemia. Thus, according to experts, one American patient with this disease costs somewhere between 200-300 thousand dollars annually.
It is proposed to pay 20% in advance in the first year, and the remaining amount to be paid in 20% installments annually for four years, provided that the effectiveness of treatment meets predetermined criteria, such as the disappearance of the need for blood transfusions or a significant reduction in the number of such procedures.
In other words, you will have to pay only based on the effectiveness of gene therapy, especially since there is still no indisputable data on the duration of its healing effect. The approach seems reasonable given the differences in intermediate outcomes among patients, although the overall effectiveness of Zynteglo is impressive.
According to industry experts, the cost of Zinteglo will be $1.2 million in the United States and $900 thousand (785 thousand euros) in Europe.
Complications of the disease
In severe forms, the disease can lead to the development of complications. Among the most common complications of a genetic mutation of the globin protein are:
- Increased iron levels in the blood. Excess iron in the body occurs due to the progression of the disease or as a result of frequent blood transfusions. High levels of iron lead to damage to the liver, endocrine system, and cause the development of arrhythmia.
- Enlarged spleen (splenomegaly). This genetic mutation is often accompanied by the destruction of a large number of red blood cells, creating an increased load on the spleen, as a result of which the organ increases in size. Splenomegaly can worsen anemia and reduce life expectancy. If the spleen is very enlarged, surgery to remove it - splenectomy - may be required. Surgery is recommended for patients over six years of age.
- Infectious complications. With a genetic mutation, the likelihood of developing infectious diseases increases. The highest risk is observed in patients after removal of the spleen.
- Bone deformation. Thalassemia can lead to bone marrow overgrowth and bone deformities. Enlarged bone marrow also causes thinning bones and increases the likelihood of fractures.
Prevention of thalassemic mutations
To prevent the risk of having children with thalassemia, parents need to visit a medical geneticist at the stage of pregnancy planning. This is especially true for families with genetic mutations of varying severity in their family. Modern antenatal diagnostics using high-tech equipment makes it possible to identify most thalassemic mutations.
If thalassemia is detected after the birth of the child, it is important to begin treatment on time. Timely adequate therapy will reduce the risk of complications and bone deformities in a child to a minimum.
Links[edit]
- ^ a b c d e f g h
Origa, Rafaella;
Mine, Paolo; Galanello, Renzo; Cao, Antonio (1 January 1993). "Alpha thalassemia". GeneReviews
. PMID 20301608. Retrieved September 22, 2021.updated 2013 - ^ a b BRS Pathology
(4th ed.). Lippincott Williams & Wilkins medical. December 2009 p. 162. ISBN. 978-1451115871. - ^ a b c d e
"Evaluation of alpha thalassemia: approaches, laboratory tests, hemoglobin electrophoresis".
emedicine.medscape.com
. Retrieved May 24, 2021. - ^ a b
“Complications and treatment |
Thalassemia | Blood diseases | NCBDDD | CDC". www.cdc.gov
. Retrieved September 22, 2021. - Online Mendelian Inheritance in Man (OMIM): hemoglobin - alpha locus 1; HBA1 - 141800
- Online Mendelian Inheritance in Man (OMIM): hemoglobin - alpha locus 2; HBA2 - 141850
- Lanzkovsky's Guide to Pediatric Hematology and Oncology 6th edition (2016)
. - ^ a b c d e
“Alpha thalassemia - Symptoms, diagnosis and treatment |
BMJ Best Practice". bestpractice.bmj.com
. Retrieved November 17, 2021. - Link, Genetics Home. "Alpha thalassemia". A Home Guide to Genetics
. Retrieved November 25, 2021. - Origa, Rafaella; Moi, Paolo (1993), Adam, Margaret P.; Ardinger, Holly H.; Pagon, Roberta A.; Wallace, Stephanie E. (ed.), "Alpha Thalassemia", GeneReviews®
, University of Washington, Seattle, PMID 20301608, retrieved November 25, 2021. - "Assessment of Anemia - Etiology | BMJ Best Practice". bestpractice.bmj.com
. Retrieved November 25, 2021. - Steensma DP, Gibbons RJ, Higgs DR (January 2005). "Acquired alpha thalassemia in association with myelodysplastic syndrome and other hematologic malignancies". Blood
.
105
(2):443–52. DOI: 10.1182/blood-2004-07-2792. PMID 15358626. - ^ a b
Galanello R, Cao A (February 2011).
“Gene test review. Alpha thalassemia". Genetics in Medicine
.
13
(2): 83–8. DOI: 10.1097/GIM.0b013e3181fcb468. PMID 21381239. - "Hemoglobin H disease". Orphan
. Retrieved September 22, 2021. - Vichinsky EP (January 1, 2009). "Alpha thalassemia major—new mutations, in utero management and outcomes." Hematology. American Society of Hematology. Educational program
.
2009
(1): 35–41. DOI: 10.1182/asheducation-2009.1.35. PMID 20008180. - ^ a b c
Viprakasit, VIP;
Equattanakit, Supachai (April 1, 2021). "Clinical classification, screening and diagnosis of thalassemia." Hematology/Oncology Clinics of North America
.
Thalassemia. 32
(2): 193–211. DOI: 10.1016/j.hoc.2017.11.006. ISSN 0889-8588. PMID 29458726. - "UpToDate" . www.uptodate.com
. Retrieved November 25, 2021. - ^ a b
Taher, Ali;
Musallam, Khaled; Cappellini, Maria Domenica, ed. (2017). Guidelines for the management of non-transfusion-dependent thalassemia (NTDT)
(2nd ed.). International Thalassemia Foundation. pp. 24–32. Retrieved November 5, 2021. - "Thalassemia | Doctor | Patient" . Patient
. Retrieved September 22, 2021. - Kroeger EM, Singer ST, Witt RG, Sweeters N, Lianoglou B, Lal A, et al (December 2021). "Favorable outcomes after intrauterine transfusion in fetuses with alpha thalassemia major: a case series and review of the literature." Prenatal diagnosis
.
36
(13):1242–1249. DOI: 10.1002/pd.4966. PMID 27862048. - Harteveld CL, Higgs DR (May 2010). "Alpha thalassemia". Journal "Orphanet of Rare Diseases"
.
5
(1): 13. DOI: 10.1186/1750-1172-5-13. PMC 2887799. PMID 20507641. - Hematology made simpler. AuthorHouse. 2013-02-06. ISBN 9781477246511. Pg. 246