Vascular diseases of the legs are quite common. They have their own specifics, which is associated with the distance of the lower extremities from the heart and the need for blood to rise from bottom to top. Vascular diseases of the legs are associated with their deformation, expansion, blockage, narrowing, and inflammation. The type of lesion depends on the structure of the wall: veins are subject to stretching of the wall and expansion of the lumen, while arteries are characterized by muscle atrophy and narrowing of the lumen. Due to these changes, the vessels cannot perform their functions normally, blood circulation is disrupted, which is fraught with serious consequences, including amputation of limbs.
Atherosclerosis of leg vessels
The disease develops gradually and usually appears after 50 years. Characterized by partial or complete blockage of arteries with cholesterol plaques.
Doctors include the following reasons:
- Natural aging of the body.
- Diabetes.
- Poor nutrition: eating foods rich in cholesterol.
- Smoking.
- Genetic predisposition.
- Excess weight, which leads to increased stress on blood vessels.
- Frequent stressful situations.
At the initial stage, atherosclerosis does not manifest itself in any way, and is often discovered by chance during an examination by a doctor.
Symptoms of the disease are caused by impaired blood circulation:
- Pale, with a bluish tint to the limbs.
- Numbness in the legs and crawling.
- Coldness in the lower extremities below the knee.
- Pain in the calves while walking and then at rest.
- Memory loss, dizziness.
- Development of heart diseases.
The diagnosis is made based on the patient’s story about his lifestyle, instrumental and laboratory tests. The attending physician prescribes to the patient:
- Blood test for coagulation and lipids.
- Ultrasonography.
- Angiography.
- Capillarography.
For atherosclerosis, complex treatment is carried out, including diet, medication, and physical therapy. As a rule, anticoagulants are prescribed as medications to prevent the formation of blood clots. In cases of significant closure of the lumen of the vessel, a surgical operation (bypass surgery) may be indicated, during which a shunt is inserted into the artery to widen it and restore blood flow.
Treatment of atherosclerosis of the lower extremities
Treatment of atherosclerosis is a complex that includes drug treatment, diet, physical therapy and, if necessary, surgical intervention.
Treatment with medications is aimed at restoring lipid metabolism, blood clotting processes and vascular metabolism. Prescribed:
- sedatives or tonics (for disturbances of nervous or endocrine metabolism),
- lowering cholesterol in the blood,
- vitamins,
- drugs that prevent the development of regional circulatory disorders.
Medical nutrition includes:
- restriction of food calories by 10-15%,
- reduction of animal fats and foods that increase cholesterol (brains, egg yolk, caviar, fatty meats and fish),
- the inclusion of products that help normalize lipid and cholesterol metabolism (cottage cheese, well-soaked herring, cod, oatmeal), vegetable oils (sunflower, corn, flaxseed, cottonseed), vegetables, fruits rich in plant fiber.
The severity of the diet is individual and depends on the degree of metabolic disorder of the patient.
Physical therapy is both a method of treating and preventing atherosclerosis. Physical training compensates for impaired body functions, has a positive effect on the functioning of the cardiovascular system, and nourishes organs and tissues with oxygen.
At the first stage of development of the disease, doctors recommend regularly doing gymnastics and walking. On weekends and during vacations, engage in tourism, skiing, skating, playing sports, etc. During the second stage of development of atherosclerosis, therapeutic exercises and walking are prescribed. Therapeutic gymnastics consists of breathing exercises and exercises with measured strength of the muscles of the arms and legs. With the third and fourth degrees of the disease, excessive physical activity is dangerous for the body. Therefore, you need to train injured limbs according to doctor’s instructions.
Surgical treatment of atherosclerosis is used for functional or morphological changes in the patient.
Obliterating endarteritis
This is one of the most complex vascular diseases of the legs. Endarteritis is characterized by damage to the walls of the arteries, leading to their narrowing (sometimes complete closure) and impaired circulation in the lower extremities. Usually, with obliterating endarteritis, changes occur in large vessels. It has been observed that people who smoke are more likely to suffer. The disease is diagnosed mainly in men aged 20-40 years, women practically do not get sick.
The causes of obliterating endarteritis have not been precisely established.
It is assumed that the impetus for the development of the disease can be:
- Disturbances in the functioning of the immune system.
- Allergic reactions.
- Blood diseases.
- Smoking.
- Complications after surgery.
- Infectious diseases.
The main symptoms of endarteritis:
- Difficulty walking and intermittent claudication.
- Severe pain.
- Rapid fatigue at low loads.
- Feeling of tingling and numbness in the legs.
- Swelling of the lower extremities.
- Blueness of the legs.
- Cramps.
- Trophic changes in the skin (dryness, cessation of hair growth, color change).
- Trophic ulcers.
The disease is considered incurable. To alleviate the condition, patients should adhere to the following recommendations:
- Completely stop smoking and drinking alcohol.
- Avoid hypothermia and heavy physical exertion on the legs.
- Take anti-inflammatory and blood thinning medications.
In severe cases, surgical treatment may be prescribed: arterial bypass, removal of the affected area of the vessel.
If left untreated, the disease can progress rapidly, leading to leg amputation.
Diagnostic methods for OASNK
If atherosclerosis of the arteries of the lower extremities is suspected, further examination is necessary to confirm (or exclude) the diagnosis of OASNK, establish the stage of the disease and determine treatment tactics. For this purpose, the following series of diagnostic measures are carried out:
- Examination by a vascular surgeon to determine the pulsation of the main arteries of the extremities, neck and abdominal cavity, as well as listening to noises in the projection of large vessels;
- Ultrasound duplex scanning
- X-ray contrast angiography;
- Computed tomography in angio mode;
- Magnetic resonance imaging in angio mode.
Through the above studies, local damage or multifocal (multi-level, multi-story) atherosclerosis of the main arteries, atherosclerosis of the aorta and arteries of the lower extremities is revealed. Areas of complete closure of the lumen (occlusion) of the artery and thrombosis may be detected.
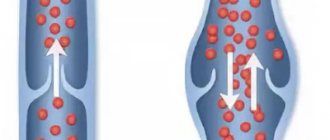
Varicose veins of the legs
This is a very common disease of the veins of the lower extremities, characterized by decreased elasticity of the venous walls and valve failure, as a result of which blood stagnates in the veins, the vessels dilate, lengthen, and form protruding nodes under the skin. The disease most often affects women. The exact causes of varicose veins are not clear. Provoking factors include:
- Hereditary predisposition.
- Valve defects and weakness of the venous walls.
- Significant loads on the legs.
- Sedentary lifestyle.
- Taking hormonal contraceptives.
- Overweight.
Reasons for appearance
Varicose veins are based on a characteristic persistent and irreversible change in the walls of blood vessels belonging to the superficial venous peripheral network. This is facilitated by venous hypertension (4, English). This increase in pressure is triggered and maintained by many predisposing factors.
At first, venous hypertension is reversible and does not lead to structural changes in blood vessels, but already at this stage pathological processes are launched, which over time or with the addition of other provoking factors lead to deformation of the veins - such irreversible changes are called varicose veins.
Even before the characteristic visible deformation of the veins, pathological processes develop with an increasing effect; consider the sequence (5, English):
- Venous hypertension is accompanied by difficulty in the outflow of blood and a slowdown in its flow. Red blood cells are grouped in the center of the lumen of the vessel, and leukocytes and platelets are pushed to its periphery.
- Redistribution of leukocytes along the inner lining of the veins. The production of endothelial factors is stimulated, which promotes the adhesion (sticking) of leukocytes and their activation. The process of thrombus formation begins, which aggravates the damage to the surface of the venous walls.
- Phlebosclerotic process in the area of venous valves. Normally, when filled with blood, the valves close tightly to each other and block the lumen of the vein. This is necessary to prevent reverse blood flow during cardiac systole. Sclerosis leads to deformation of the valves, and they are no longer able to fully perform their function.
At the earliest stages, all these changes do not yet lead to clinically significant hemodynamic disturbances. And patient complaints are so far limited to cosmetic defects. Over time, visible deformation of the affected area of the vessel begins. The vein acquires pathological bends and lengthens somewhat, local expansions and saccular bulges in the form of varicose nodes appear on it. This is accompanied by worsening valve insufficiency - the valves located in the area of varicose deformation cease to touch each other when filled.
The pathological reverse flow of blood that occurs at this stage is called vertical reflux. This hemodynamic disturbance is one of the key pathogenetic aspects of varicose veins, as it contributes to the formation of chronic venous insufficiency with blood stagnation. It is this that leads to the appearance of the main symptoms of varicose veins. But when small and very small venous vessels in the thickness of the dermis are affected, clinically significant stagnation of blood does not occur.
Phlebitis
This is inflammation of the walls of the veins with subsequent disruption of blood vessels and deterioration of blood circulation. The main reasons for the development of phlebitis are as follows:
- Varicose veins.
- Infectious diseases.
- Injuries.
Signs of phlebitis:
- The affected vein becomes deformed, increases in size and becomes dense.
- The skin at the site of the affected vessel turns red and its temperature rises.
- The sore leg becomes uncomfortable and may swell.
The disease can be both acute and chronic. With phlebitis, thrombophlebitis often develops, that is, in addition to inflammation of the walls of the veins, their blockage (partial or complete) with a blood clot is added.
Treatment will depend on the causes of phlebitis. Typically, patients are prescribed anti-inflammatory drugs in the form of tablets or injections, and anticoagulants to prevent increased blood clotting and the formation of blood clots.
Possible complications
Deformed veins and the sclerotic valves located in them are not able to recover to their original level under the influence of drug therapy. The changes are irreversible and prone to progression, especially when provoking factors persist and new adverse effects are added.
In the initial stages of the disease, developing venous insufficiency can decompensate - this does not indicate getting rid of varicose veins, but a temporary slowdown in the pathological process. Subsequently, adjacent sections of the vein and other vessels are involved in phlebosclerosis. The greatest clinical significance is the damage to the communicating veins, which provide communication between the superficial venous network of the legs and the deep one. They penetrate (perforate) the fascia located on top of the muscles, therefore they are also called perforators.
Most communicating vessels also have valves, which normally prevent the non-physiological discharge of blood from deep veins to superficial ones, therefore varicose changes in perforators are accompanied by the development of horizontal reflux. This shutdown of the natural mechanism for regulating pressure in the superficial venous system leads to serious consequences:
What happens if varicose veins are not treated?
Turning off the natural mechanism for regulating pressure in the superficial venous system leads to serious consequences (11, German):
- worsening phlebosclerosis and accelerating the process of varicose veins against the background of significantly increased venous hypertension;
- increased phlebostasis, which increases the likelihood of developing intravascular thrombosis;
- disruption of the walls of the capillary network, which is accompanied by an increase in their permeability to plasma and protein molecules, accumulation of metabolic products in tissues and the development of chronic hypoxia.
The addition of horizontal reflux is a factor contributing to persistent decompensation of chronic venous insufficiency. Trophic disorders arise and increase in the skin and soft tissues, swelling and physical discomfort experienced by the patient increase, and the risk of developing thrombophlebitis increases. Varicose veins become complicated, advanced, with a significant area of damage to the veins. And the treatment will no longer give as quick and tangible results as at the early stage.
Thrombophlebitis
This disease is characterized by inflammation of the walls of the veins with a simultaneous increase in blood viscosity, the formation of blood clots, narrowing of the lumen of blood vessels and poor circulation. Blood clots are life-threatening because they can break off and enter any part of the circulatory system, including the pulmonary artery. Often thrombophlebitis of the lower extremities develops with varicose veins, but there are other causes of the pathology:
- Infectious diseases.
- Injuries of the lower extremities.
- Increased blood clotting.
- Changes in blood composition, for example, as a result of taking certain medications.
- Pregnancy and childbirth.
Thrombophlebitis that develops with varicose veins usually affects the lower part of the thigh and the upper third of the lower leg. The following symptoms are noted:
- general deterioration of health (malaise, fever);
- pain in the area of the affected vessel, which intensifies with movement;
- redness and shine of the skin in the projection of the affected vein;
- swelling of the affected leg and its noticeable difference in size from the healthy one;
- infiltrates in the form of cord-like seals are easily palpable.
Treatment of thrombophlebitis primarily involves taking blood thinners to prevent blood clots, followed by anti-inflammatory drugs. If a blood clot is present, surgical intervention is indicated to remove the blockage of the vein. In addition, it is necessary to wear compression hosiery, use gels, massage, and physical exercises that improve blood circulation in the veins.
Symptoms and manifestations of varicose veins at the initial stage
The symptoms of initial varicose veins depend on the diameter of the affected vessels and their significance for the general venous outflow.
The “cosmetic” type of the disease is characterized by the presence of only external defects in the form of spider veins (telangiectasia) or a superficial fine mesh. There cannot be any other complaints, since the affected vessels have a very small diameter and are responsible for draining blood only from certain areas of the skin.
With the classic version of varicose veins, the symptoms are more obvious, although physical discomfort in the early stages of the disease is not permanent. The quality of life does not deteriorate significantly, and no serious complications arise. In this form, varicose veins can exist for quite a long time, decompensating and progressing with the addition of additional risk factors.
Severe symptoms of varicose veins
Symptoms of varicose veins affecting the saphenous veins of the legs include (8, English):
- Increased venous pattern in the lower extremities. There is a change in the course of visible superficial vessels and their bulging. But with obesity, this symptom is often masked by overdeveloped subcutaneous tissue. Obvious nodular deformation of blood vessels usually develops in later stages of the disease.
- The appearance of heaviness, a feeling of fullness and fatigue in the legs are signs of decompensation of venous insufficiency. They are usually accompanied by a tendency to slight swelling (pasty) of the legs. Such complaints may appear towards the end of the working day, especially if professional activities involve prolonged standing or sitting. In the early stages of varicose veins, discomfort and swelling disappear soon after taking a horizontal position with legs elevated. Facilitates the condition and performance of a set of exercises to engage the muscle pump of the legs.
- Increased fatigue of the leg muscles, and in some patients a tendency to cramps. This is explained by the beginning of metabolic changes in tissues, which are caused by microcirculation disorders against the background of phlebostasis.
The severity of symptoms may vary. In some patients, varicose veins in the initial stage debut with visible changes in the superficial veins. In others, signs of venous insufficiency initially appear, which is a sign of already existing valve pathology and serves as an indicator of a less favorable course of varicose veins.
Thrombosis
Inflammation of the deep veins and the formation of blood clots in them is called thrombosis. A thrombus quickly forms, and if it is not tightly attached to the wall of the vein, it can break off at any time and move along the vascular bed.
The main causes of thrombosis are as follows:
- congenital vascular pathologies;
- hormonal disorders;
- tumors;
- injuries with vascular damage;
- fractures;
- surgical interventions;
- leg paralysis and paresis;
- severe infections;
- excess weight.
In addition, provoking factors include:
- elderly age;
- heavy physical activity;
- sedentary lifestyle;
- prolonged bed rest and immobility;
- bad habits (drinking alcohol, smoking).
Symptoms of the disease are not always clearly expressed. Thrombosis can be suspected based on the following signs:
- Bursting, tugging, squeezing pain in the evening.
- Numbness and crawling in the lower legs.
- Heaviness in the leg at the end of the day.
- Swelling and increase in volume of the affected limb.
- Thinning of the skin of the affected leg, pallor and cyanosis.
- Glossy leather.
- Increase in temperature (general and local).
- Filling of the superficial veins with blood and their pronounced pattern under the skin.
- The temperature of the diseased leg is lower than that of the healthy leg.
Treatment of thrombosis can be conservative and surgical. In the first case, drugs of the following groups are prescribed:
- anti-inflammatory;
- anticoagulants of direct and indirect action;
- enzymes with thrombolytic properties;
- agents that improve microcirculation and blood fluidity.
In addition, elastic bandaging or wearing compression stockings is recommended.
Surgical treatment is prescribed for severe inflammation, a floating thrombus and a high risk of thrombus rupture with subsequent development of pulmonary embolism. The most common operation is thrombectomy, during which the clot is removed and blood flow is restored.
Prevention
The best way to prevent intermittent claudication and other symptoms of vascular disease in the legs is to maintain a healthy lifestyle. It means:
- Quit smoking if you smoke!
- If you have diabetes, monitor your blood glucose levels.
- Regular exercise for 30 minutes, at least 3 times a week, after consultation with your doctor.
- Reduce cholesterol and blood pressure.
- Eat foods low in saturated fat.
- Maintain a normal weight.
The concept of “ischemic syndrome” in the clinic of obliterating vascular diseases
Ischemic syndrome develops in the case of blockage of a large artery by an atherosclerotic plaque, narrowing of the lumen of small arterioles due to thickening of the inner lining (intima) of the vessels. Pain occurs in the limb while walking a certain distance. The patient perceives this pain as a blow from a whip; he is forced to stop and rest for a while. So, with ischemia of the first degree, the so-called “intermittent claudication” occurs when walking after 500 m, with the second - 200 m, and the third degree is characterized by the occurrence of pain after 10 - 15 m. With the fourth degree of ischemia, the pain is constant, necrosis of the limb tissue occurs and gangrene develops.