Pressure
40 thousand die every year due to cerebral hemorrhage due to high blood pressure. At the same time, if you follow the rules for controlling blood pressure and do not provoke its increase, you can avoid not only feeling unwell, but also more serious problems.
A persistent increase in blood pressure above 140/90 is a serious factor for concern and suspicion of the risk of cardiovascular disease.
Too rare (less than 50 beats per minute), frequent (more than 90–100 per minute) or irregular pulse should also alert you; such deviations may indicate coronary disease, a violation of the conduction system of the heart and the regulation of cardiac activity.
To keep your heart beating correctly
The heart is the “motor” that forces our body to work without days off or breaks. It is not surprising that it is this organ that often needs routine, or even major, “repairs”. Well-known Samara cardiologist Mikhail Kachkovsky spoke to the press about the risks of heart disease and how to avoid them.
— Heart disease is dangerous because it is one of the main causes of mortality in the population. Moreover, if every fourth person in the world dies from these diseases, in Russia every second person dies,” Mikhail Arkadyevich voiced the sad statistics.
Pain resembling osteochondrosis
Pain between the shoulder blades, in the neck, left arm, shoulder, wrist, even in the jaw can be a sure sign of not only osteochondrosis or myositis, but also heart problems.
Article on the topic
Stroke: risk factors, dangerous symptoms, first aid A symptom of angina pectoris may be the occurrence of such symptoms after physical activity or emotional shock. If pain occurs even during rest and after using special heart medications, this symptom may indicate an approaching heart attack.
Endovascular diagnostic methods
It is impossible to imagine medicine of the 21st century without endovascular methods of diagnosis and treatment. Currently, X-ray endovascular surgery is a highly effective and low-traumatic method of treatment for coronary disease, vascular and valvular pathology, and congenital heart defects. Endovascular surgery occupies its niche in almost all areas of modern medicine (oncology, urology, gynecology, etc.). The development of endovascular treatment methods promotes close cooperation between endovascular surgeons, cardiologists, cardiac surgeons and other related specialties. Such cooperation led to the development of a new direction - the so-called hybrid surgery.
Over the past decades, the number of clinics engaged in endovascular surgery has increased significantly in our country. The nineties of the 20th century became the heyday of endovascular surgery. Catheter technology has reached a high level of development and is constantly being improved. High-tech innovations appear almost every year. Some of them are destined to remain in the history of interventional cardiology, and some are destined to become the operator’s perfect tool. And only extensive experimental and clinical experience will be able to determine the place of each method in endovascular surgery.
Today, X-ray endovascular interventions represent an alternative to almost any open surgery for pathology of the heart and blood vessels. The range of endovascular interventions performed is enormous.
Federal State Budgetary Institution National Medical Research Center of Sports Sciences named after. A.N. The Ministry of Health of the Russian Federation is one of the pioneers of domestic endovascular surgery. It was here in 1982 that the cornerstone of many schools on endovascular diagnostics and treatment was laid. Today, the departments of the Federal State Budgetary Institution National Medical Research Center for Cardiovascular Agricultural Sciences named after. A.N. The Ministry of Health of the Russian Federation, engaged in the provision of x-ray endovascular medical care, is equipped with the most modern equipment, not inferior to leading clinics in Europe and the USA, including all available methods of intravascular imaging and invasive assessment of intracoronary physiology. Every year, the center performs more than 15,000 diagnostic endovascular interventions and more than 3,000 thousand endovascular operations in patients with coronary heart disease, vascular pathology, congenital and acquired heart defects . The staff of the departments is represented by first-class international specialists who have extensive experience in performing these operations in complex clinical cases.
Cardiac ischemia
Coronary heart disease is an acute or chronic myocardial damage that occurs as a result of a decrease or cessation of arterial blood supply to the heart muscle, which is based on pathological processes in the coronary artery system. IHD is a widespread disease. One of the leading causes of mortality, temporary and permanent disability throughout the world. In the structure of mortality, cardiovascular diseases are in first place, of which IHD accounts for about 40%.
Etiology of IHD
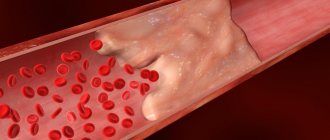
The leading etiological factor in the development of coronary heart disease is atherosclerosis of the coronary arteries. Atherosclerosis develops consistently, in waves and steadily. As a result of the accumulation of cholesterol in the artery wall, an atherosclerotic plaque is formed. Excess cholesterol leads to an increase in plaque size and obstructions to blood flow. Symptoms worsen with the growth of atherosclerotic plaque, which gradually narrows the lumen of the artery. A decrease in the lumen area of the artery by more than 90-95% is critical, causing a decrease in coronary blood flow and deterioration of well-being even at rest.
Clinical picture of IHD
The first description of angina pectoris was offered by the English physician William Heberden in 1772: “... pain in the chest that occurs while walking and forces the patient to stop, especially while walking soon after eating. It seems that this pain, if it continues or intensifies, can take a person’s life...” Usually, symptoms of the disease first appear after 50 years. At first they occur only during physical activity.
The classic manifestations of coronary heart disease are:
- Pain behind the sternum, often radiating to the lower jaw, neck, left shoulder, forearm, hand, back. Often occurs in cold weather.
- The pain is pressing, squeezing, burning, suffocating. The intensity varies.
- Triggered by physical or emotional factors. At rest it stops on its own.
- Lasts from 30 seconds to 5-15 minutes.
- Quick effect of taking nitroglycerin.
Diagnosis of IHD
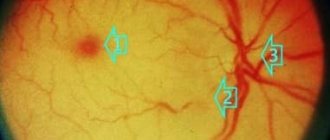
Selective coronary angiography is considered the “gold standard” in the diagnosis of obstructive lesions of the coronary arteries of the heart.
This X-ray contrast study is used to find out whether the narrowing of the vessel is significant, which arteries and how many of them are affected, in what place and over what extent.
Treatment of coronary artery disease
Treatment of this pathology is primarily aimed at restoring normal blood supply to the myocardium and improving the quality of life of patients. Unfortunately, purely therapeutic (conservative) treatment methods are not always effective. Today, the generally accepted methods of treating coronary artery disease with proven and undeniable effectiveness are surgical revascularization of the myocardium - coronary artery bypass grafting (CABG) and percutaneous coronary intervention (PCI) or “stenting”.
The first coronary artery stenting in humans was performed by J. Puel et al. in March 1986 in Toulouse (France) and almost simultaneously with them U. Sigwart et al. in Lausanne (Switzerland).
Today, in the era of high technologies in the field of pharmaceuticals and medical engineering, modern intracoronary stents make it possible to achieve good results both in the early and late periods after PCI.
This operation is performed under local anesthesia . An artery puncture (radial or femoral) is performed in the wrist or thigh area, an introducer (catheter) is installed, and a guiding catheter is inserted through it along a guide under the control of an angiographic unit.
The catheter is inserted into the left or right coronary artery, and then a series of images are taken. Through the installed catheter, a microconductor is passed into the artery through the affected area. A coronary stent is guided and installed to the affected area via a microconductor.
Today, the range of percutaneous coronary interventions has expanded significantly from the treatment of simple local narrowings to multivessel revascularization of the myocardium (including the trunk of the left coronary artery) and recanalization of chronically occluded (completely closed vessels) coronary arteries. Today, stents with a special bioabsorbable coating have been introduced into clinical practice ,
allowing to reduce the frequency of restenosis (overgrowth) and stent thrombosis, thereby minimizing the risk of recurrent heart attacks in the patient after stenting. Intravascular imaging techniques have also been widely introduced, providing real-time images of the coronary arteries in the patient during surgery, comparable to data obtained using a light microscope. All of the above makes it possible to obtain intraluminal images of the coronary arteries in real time. This allows the surgeon to obtain a “jewelry” result when installing a stent in the coronary vessels.
Intraoperative shuntoraphy
At the Federal State Budgetary Institution National Medical Research Center for Sports Agriculture named after. A.N. , intraoperative shuntography was introduced into routine practice
. Intraoperative bypass grafting is an angiographic study at the final stage of coronary artery bypass surgery. Using anigography, the patency of all placed bypasses is checked directly in the cardiac surgery operating room. If a lesion or malfunction of the shunt is detected, the operating surgeon has the opportunity to eliminate it directly in the operating room, thereby achieving an “ideal” result of a major cardiac surgery.
Federal State Budgetary Institution National Medical Research Center of Sports Sciences named after. A. N. Bakuleva Ministry of Health of the Russian Federation is the only center in the Russian Federation and one of the few centers in the world where intraoperative bypass grafting is performed simultaneously with coronary bypass surgery.
Congenital heart defects (CHD)
The second half of the twentieth century was marked by stunning advances in virtually all aspects of pediatric cardiovascular surgery.
Currently, using X-ray endovascular treatment methods, it is possible to eliminate such congenital heart defects as atrial septal defect (ASD), patent ductus arteriosus (PDA) or ductus Botallus, patent foramen ovale (POO), ventricular septal defect (VSD), coarctation of the aorta. Over the past decade, these interventions have become the “standard” procedure with virtually zero mortality. X-ray endovascular treatment methods are the method of choice for such critical conditions of newborns as critical valvular stenosis of the aorta and pulmonary artery. The implementation of balloon atrioseptostomy, proposed in 1966 by Rashkind and Miller, in newborns with complex congenital heart disease incompatible with life led to a sharp decrease in mortality among this severe category of patients.
Today, at the Federal State Budgetary Institution National Medical Research Center for Cardiovascular Agricultural Sciences named after. A.N. Bakulev Ministry of Health of the Russian Federation performs a full range of endovascular interventions for congenital heart defects in patients of all age groups,
including in newborns with critical malformations of the heart and blood vessels.
Many operations were performed for the first time in world practice, and the developed techniques are unique.
The most common are patent ductus arteriosus, atrial septal defect, coarctation of the aorta, valvular stenosis of the aorta and pulmonary artery.
Coarctation of the aorta
Coarctation of the aorta is a congenital narrowing of the aorta in the area of transition of the arch into the descending part of the aorta, and sometimes in the thoracic or abdominal region. The frequency of this defect ranges from 6.3% to 15% among all congenital heart defects (CHD). The defect is rarely isolated; more often it is combined with other congenital defects.
Clinic
Patients complain of dizziness, heaviness and headache, increased fatigue, nosebleeds, possible pain in the heart, as well as weakness and pain in the lower extremities, cramps in the leg muscles, and chilly feet. Women may experience menstrual irregularities and infertility. On examination, good physical development is noted with a disproportion of the muscular system: the muscles of the upper half of the body are hypertrophied with relative hypotrophy of the muscles of the pelvis and lower extremities, the legs are cold to the touch. When palpating the intercostal arteries, their increased pulsation is noted.
Of decisive importance in the diagnosis of aortic coarctation is determining the nature of the pulse in the arms and legs. There is no or sharply weakened pulsation in the femoral arteries, and at the same time a tense pulse in the upper extremities. Systolic blood pressure in the arms of patients with isolated severe coarctation of the aorta reaches high numbers up to 190-200/90-100 mm Hg.
Diagnostics
Diagnosis is suggested by clinical examination (including blood pressure measurements in all 4 extremities), confirmed by chest x-ray and ECG, and based on the results of two-dimensional color flow echocardiography and Doppler studies. In older patients - using CT or MR angiography.
The most informative method for detecting aortic coarctation is
two-dimensional echocardiography (EchoCG).
Endovascular treatment In our country, the first TLBAP for aortic coarctation was performed by Yu.S. Petrosyan et al. in 1985 at the Institute of Cardiovascular Surgery of the USSR Academy of Medical Sciences. The operation is performed under sedation through a small puncture of the femoral artery. A catheter and balloon are passed through the puncture to the site of narrowing of the aorta. Next, the narrowed section of the aorta is expanded with a balloon of the appropriate size, restoring the lumen and blood flow through the aorta. Federal State Budgetary Institution "NMITs SSH im. A.N. Bakuleva" has extensive experience in the treatment of aortic coarctation.
Angiogram of a patient with aortic coarctation performed via arterial access:
a- aorthoraphy before balloon angioplasty, arrows indicate the membrane in the area of the aortic isthmus;
b — opening of the balloon (the arrow indicates the constriction corresponding to the area of coarctation of the artery);
c- aortography after balloon angioplasty - narrowing of the aortic isthmus has been eliminated.
Stenting of aortic coarctation in children weighing more than 15 kg
Stenting of coarctation/recoarctation is indicated in children weighing more than 15-20 kg. It must be remembered that stenting of aortic coarctation is performed with special stents, which can be further expanded as the child grows.
Drawing. Stenting of aortic coarctation
A – aortography visualizes a narrowing of the isthmus
B — after stenting of aortic coarctation.
VALVE AORTIC STENOSIS IN NEWBORNS
Valvular aortic stenosis is a congenital heart defect in which the cusps of the aortic valve are fused. Without surgical intervention, the mortality rate among newborns with congenital valvular aortic stenosis is extremely high - almost 85-90% of patients die during the first month of life.
Symptoms
Newborns with severe aortic stenosis become irritable, eat poorly, sweat during feeding, have trouble breathing, have unnaturally pale or grayish skin, cold palms and soles, decreased urine output, and an increased heart rate.
Treatment
Balloon dilatation (expansion) of the aortic valve is one of the treatment methods
Experience of the Federal State Budgetary Institution "NMITSSSH im. A.N. Bakulev"
National Medical Research Center for Cardiovascular Surgery named after. A. N. Bakuleva.
Drawing. Stages of performing transluminal balloon valvuloplasty of aortic valve stenosis.
a — angiography of the ascending aorta: a stream (arrow) of non-constricted blood is visible, indicating stenosis of the aortic valve;
b — left ventriculography (the arrow indicates the flow of uncontrasted blood from the LV, also indicating aortic valve stenosis);
c – positioning of the balloon in the projection of the aortic valve. Radiopaque balloon marks (arrows) are located above and below the aortic valve annulus;
Atrial septal defect
Atrial septal defect (ASD) is a congenital heart defect (CHD), characterized by the presence of a communication (hole) between the right and left atria, which causes the existence of an arteriovenous discharge between them. The risk of developing an ASD in an unborn child is significantly higher in those families where there are relatives with congenital heart disease. In addition to hereditary conditions, viral diseases of the pregnant woman (rubella, chickenpox, etc.), endocrinopathies, taking certain medications and alcohol during pregnancy, occupational hazards, gestational complications (toxicosis, threat of miscarriage, etc.) can lead to the occurrence of ASD.
Complaints
Dyspnea and palpitations are the most common early symptoms of the disease in large ASDs in children, but usually during the first months of life hemodynamic compensation and regression of the clinical picture occur. Subsequently, in most children, ASDs are asymptomatic, and patients have no complaints. Children often have an asthenic physique with noticeable pallor of the skin.
Diagnosis
It is recommended to diagnose ASD using transthoracic echocardiography (EchoCG) using color Doppler mapping, which is the main diagnostic tool in diagnosing ASD, determining its size, location, volume and direction of blood shunting.
Today, endovascular treatment methods with appropriate anatomy are the method of choice in the treatment of ASD. Defects are closed using special occluder devices. The occluder is a double-disk device: the left disk opens in the left atrium, the right disk opens in the right atrium. The defect remains between the two disks. The operation is performed under local anesthesia through the femoral vein. The duration of the operation is 40-60 minutes. After the operation, the patient is transferred to the ward and can be discharged the next day.
Drawing. Various modifications of occluders for closing atrial septal defect.
Patent ductus arteriosus
Patent ductus arteriosus (PDA) is a vessel through which pathological communication between the aorta and the pulmonary artery (PA) remains after birth. Comments: Normally, the PDA is necessarily present in the fetus, but closes soon after birth, turning into an arterial ligament.
Risk factors for patent ductus arteriosus are premature birth and prematurity, family history, the presence of other congenital heart diseases, infectious and somatic diseases of the pregnant woman.
PDA usually occurs in premature infants and is extremely rare in infants born at term.
Complaints of patients with PDA are nonspecific. Clinical manifestations depend on the size of the duct and the stage of hemodynamic disorders. The course of the defect varies from asymptomatic to extremely severe. With large duct sizes, the latter manifests itself already from the first weeks of life with signs of heart failure and retardation in physical development. In young children, when screaming (or straining), cyanosis may appear, which is more pronounced on the lower half of the body, especially on the lower extremities. It is typical that cyanosis disappears after the load is stopped.
Diagnostics
The main diagnostic method is ultrasound and auscultation. Auscultation reveals a “machine” noise characteristic of the defect in the second or third intercostal space to the left of the sternum, radiating into the interscapular space and vessels of the neck.
Treatment
The main treatment method for PDA is endovascular intervention. Small ducts are closed using spirals, large ones (more than 3 mm) - using occluders. In 1992, P. Cambier was the first in the world to use a coil for embolization of the patent ductus arteriosus. The operation is performed through the femoral artery or vein without opening the chest. The duration of the operation is 30-40 minutes. The patient is transferred to a ward under observation and can be discharged after a day. The implanted devices are MRI-compatible, meaning MRI examinations can be performed after 6 months.
A B
Drawing. A - Patent ductus arteriosus. B - after closing the duct with a spiral.
Large ducts are closed using special devices called occluders.
Drawing. Occluder for closing the patent ductus arteriosus.
Patent foramen ovale
The patent foramen ovale (PFO) is a short interatrial canal (average length 5 mm) located exactly on the axis of blood flow coming from the inferior vena cava. In 25-30% there is no complete anatomical occlusion, and the oval window remains open or, more precisely, openable. This is called LLC and, as a rule, is not considered a deviation, but rather a variant of the norm. In most cases, LLC remains asymptomatic and does not manifest itself. The most obvious manifestations of PFO are paradoxical arterial embolisms, the most serious of which are the resulting strokes .
Indications for closing an LLC:
Migraine (with aura), sleep apnea, stroke, diving, high-altitude pulmonary edema, LLC is closed using special occluders. The operation is performed under local anesthesia, accessed through the femoral vein. An occluder is passed through the installed catheter, which closes the LLC using two disks (“sandwich”).
Drawing. Various devices for closing a patent oval window
Vascular pathology
Endovascular methods of treating blood vessels and veins is one of the most interesting and rapidly developing specialties of medicine with a steady increase in the number of operations. Endovascular treatment methods are used when all major vessels and veins are affected (carotid, renal, subclavian arteries, vessels of the lower extremities).
Vascular pathology
X-ray endovascular methods of diagnosis and treatment occupy a leading position in the treatment of vascular pathology, and their share is steadily growing every year. These methods are most actively used in the pathology of the carotid, brachiocephalic, renal arteries, and vessels of the lower extremities.
Stenting of the internal carotid artery
According to the American Heart Association (AHA/ASA), approximately 6.5 million strokes occur annually in the United States. About 20% of all ischemic strokes occur due to atherosclerotic stenosis of the carotid arteries, usually located in the area of their division into the external and internal arteries. Atherosclerosis of the ICA is one of the main pathologies of the ICA, which poses a threat of developing cerebral stroke due to blockage of cerebral vessels, followed by disability or leading to death.
Clinic:
If
patency is impaired, the following manifestations occur:
- stroke
- dizziness
- noise in ears
- darkening of the eyes
- weakness
Often arterial stenosis precedes an acute disruption of cerebral blood supply. Pathology can be recognized by the following symptoms:
- nausea and vomiting
- headache
- numbness of the limbs or one side of the face
- difficulties with coordination
- speech problems
Diagnostics:
- USDG
- CT – angiography
- Angiography
Surgery:
One of the treatment methods for internal carotid artery (ICA) stenosis is ICA stenting. The method consists of installing a high-tech, biocompatible, metal (cobalt-chromium alloy) frame in the narrowing zone with complete restoration of the artery lumen, which prevents the development of acute disorders of cerebral blood supply (TIA and stroke).
This operation is performed under local anesthesia using access through the femoral or radial arteries (through the thigh or arm). Through an installed catheter, a special self-expanding stent of various designs is passed and implanted into the affected area of the carotid artery. In order to reduce the number of complications, special filter traps are used in all operations. After the operation, the patient is transferred to the ward and discharged the next day.
Clinical examples:
- Stenosis of the left ICA 85%
- Stenosis of the right ICA 95%
Renal artery stenting
The blood supply to the kidneys is provided by the renal arteries, which arise from the largest vessel in the body (the aorta). With renal artery stenosis, the patient develops so-called renovascular hypertension. Progression of stenosis over time can lead to the development of renal failure.
Diagnostics:
- USDG
- CT – angiography
- Angiography
Surgery:
Renal artery stenting is an effective and safe procedure. The method consists of installing a high-tech, biocompatible, metal (cobalt chromium alloy) frame into the narrowing zone, under local anesthesia, with complete restoration of the artery lumen, which prevents further progress of organ ischemia (decreased function), and also leads to stabilization of blood pressure.
Stenting of lower extremity arteries
Pathology:
Atherosclerosis of the arteries of the lower extremities is one of the main pathologies, which poses a threat to the development of ischemia of the lower extremities, leading to decreased function of the lower extremities, as well as trophic tissue damage.
Clinic:
If patency is impaired, the following manifestations occur:
- Pain in the legs when walking - “intermittent claudication”
- Numbness, cold feet
- Hair reduction
- Dystrophy of the nail plates
- Trophic ulcers
- Dry gangrene
- Wet gangrene
- Dysfunction of the pelvic organs
Diagnostics:
- USDG
- CT – angiography
- Angiography
Surgery:
Stenting of the arteries of the lower extremities is an effective and safe procedure. The method consists of installing a high-tech, biocompatible, metal (cobalt-chromium alloy) frame into the narrowing zone, under local anesthesia, with complete restoration of the lumen of the artery, which prevents the development of chronic and acute disorders of the blood supply to the lower limb, and also eliminates the clinical picture of the disease.
Subclavian artery stenting
Atherosclerosis of the subclavian artery develops most often in the initial part of this artery and may be accompanied by the development of symptoms of circulatory disorders in the arm or cerebral circulatory failure due to the phenomenon of vertebral-subclavian steal, when blood flows through the vertebral artery into the subclavian artery, as a result of which the development of cerebral ischemia is possible .
Clinic:
If its patency is impaired, the following manifestations occur:
- Pain, fatigue, coldness, parasthesia, numbness of the upper limb
- Dizziness
- Instability
- Ataxia
- Nystagmus, diplopia, hemianopsia
- Hearing loss
Diagnostics:
- USDG
- CT – angiography
- Angiography
Surgery:
Subclavian artery stenting is an effective and safe procedure. The procedure is painless and takes place under local anesthesia.
Stenting is performed through a small puncture in the femoral or radial artery (through the arm). Through an installed catheter, a special stent of the appropriate size is passed into the affected area of the subclavian artery and implanted. Next, the stent is deployed and the narrowed area is reinforced with complete restoration of the lumen.
Endoprosthetics of the abdominal aorta
Anatomy:
The aorta is the largest vessel in the human body. It departs directly from the heart, giving off main branches to all organs and tissues in the body. Anatomically, the aorta is divided into the ascending section (aortic arch) and the descending section (thoracic section and abdominal section).
Pathology:
An aortic aneurysm is usually called a lumen formed in it that is twice (or more) the normal diameter of the vessels. The defect appears as a result of the destruction of the elastic fibers (filaments) of the central shell, as a result of which the remaining fibrous tissue elongates, thereby expanding the diameter of the vessels and leading to thinning and tension of their walls. As the disease progresses and the subsequent increase in the size of the lumen, there is a possibility of rupture of the aortic aneurysm with massive internal bleeding, leading to death in 2 out of 5 cases.
Clinic:
An abdominal aortic aneurysm manifests itself in the form of dull, aching and gradually increasing pain in the abdomen. Unpleasant sensations, as a rule, occur to the left of the navel and radiate to the back, sacrum and lower back. If such symptoms are detected, you should consult a doctor, otherwise the abdominal aortic aneurysm may rupture.
Most often, with an abdominal aortic aneurysm, the first signal is attacks of pain. They occur unexpectedly and often radiate to the lower back, groin area or legs. The pain lasts for several hours and is difficult to respond to medications. When the aneurysm becomes inflamed, the temperature may rise. Sometimes blueness and coldness of the fingers are observed.
Diagnostics:
- USDG
- MRI
- CT – angiography
- Angiography
Surgery:
Abdominal aortic replacement is an effective and safe procedure. The method consists of installing a high-tech, biocompatible, coated metal (cobalt-chromium alloy) frame into the expansion zone, under local anesthesia, completely excluding the aneurysmal expansion from the bloodstream, which prevents further increase in the size of the aneurysm, the formation of blood clots, and also prevents aortic rupture.
Drawing
Abdominal aortic aneurysm before and after stenting
Transcatheter aortic valve implantation
Transcatheter aortic valve implantation (TAI) has opened new possibilities for the treatment of patients with severe disease (narrowing) of the aortic valve. Transcatheter aortic valve implantation (TAVI) is a modern minimally invasive transcatheter method of replacing the fortal valve with an artificial biological one.
Aortic valve stenosis
- a severe pathology, it ranks second among all acquired structural heart diseases, and significantly increases the risk of sudden cardiac death. Such patients experience severe heart failure and shortness of breath even with minimal exertion, attacks of angina in the form of chest pain, sudden weakness, peripheral edema and fainting. Just 15 years ago, the main method of treating this pathology was open surgery on a stopped heart. However, in modern medical practice, an alternative minimally invasive transcatheter approach of aortic valve implantation (TAI) is increasingly being used, when a biological prosthesis is passed through the opening in the common femoral artery and implanted in the position of the aortic valve. In 80% of cases, the operation does not require general anesthesia; the patient is conscious and in contact with the doctor. The operation time varies from 30 to 70 minutes, and the patient's stay in the intensive care unit is reduced to 24 hours. Modern endovascular valve prostheses have proven their effectiveness in many multicenter studies conducted by leading clinics in Europe and the USA, and the design of the models used allows us to minimize the risks of developing adverse consequences in the postoperative period while achieving maximum clinical effect.
Drawing. Transcatheter aortic valve implantation
Chest pain
A feeling of burning and squeezing, obvious, dull, severe or periodic pain, spasm - all these sensations in the chest are the surest sign of heart problems. With spasm of the coronary vessels, the pain is burning and acute, which is a sign of angina pectoris, which often occurs even at rest, for example at night. An attack of angina is a harbinger of myocardial infarction and coronary heart disease (CHD).
Severe, prolonged pain in the chest, radiating to the left arm, neck and back, is characteristic of a developing myocardial infarction. Chest pain during myocardial infarction can be extremely severe, including loss of consciousness. By the way, one of the most common causes of heart attack is atherosclerosis of the coronary vessels.
Chest pain radiating to the back of the head, back, or groin area is a symptom of an aortic aneurysm or dissection.
Dull and wave-like pain in the heart area, which does not spread to other areas of the body, accompanied by an increase in temperature, indicates the development of pericarditis.
However, acute chest pain may also indicate other diseases, for example, be a symptom of intercostal neuralgia, herpes zoster, sciatica in the neck or chest, spontaneous pneumothorax, or esophageal spasm.
Blue lips – cyanosis
If this happens not because you are cold, and is accompanied by blue nails and increased heart rate, then this is a very bad symptom. It indicates that there are disruptions in cardiac activity and the heart does not provide the body with oxygen. Blue lips and nails are characteristic of heart disease.
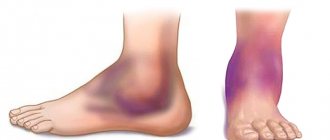
Legs can swell not only with heart disease, but also with kidney problems, varicose veins, and liver damage. Cardiac edema has characteristic features. Such swelling develops gradually, affecting the ankles of both legs, rising to the shins. The skin at the site of swelling is dense, cold (feet often get cold), and has a bluish tint. The swelling is painless, even when pressure is applied to it.
Such swelling, accompanied by other symptoms of heart problems, indicates developing heart failure, so they are the reason for contacting a cardiologist.
All of the above signs, especially if they appear in combination, cannot be ignored. The heart is no joke - myocardial infarction, stroke, cardiac arrest can occur suddenly. To prevent this from happening, you need to promptly contact a cardiologist, undergo an examination, identify the disease and follow all the doctor’s recommendations.
Palpitations
Palpitations can occur during intense physical activity, as a result of a person's emotional arousal, or due to overeating. But a strong heartbeat is very often an early warning sign of cardiovascular disease.
A strong heartbeat manifests itself as a feeling of disruption in the functioning of the heart; it seems that the heart is almost “jumping out” of the chest or freezing. Attacks may be accompanied by weakness, discomfort in the heart, and fainting.
Such symptoms may indicate tachycardia, angina pectoris, heart failure, or impaired blood supply to organs.
If you have at least one of the listed symptoms, it is important to immediately consult a doctor and undergo tests that will reveal the true cause of the ailment. One of the most effective methods of treating any disease is its early diagnosis and timely prevention.
Lack of air - shortness of breath
The condition of shortness of breath - difficulty breathing, lack of air - indicates heart or pulmonary failure. Cardiac shortness of breath initially develops with physical effort and goes away when the load stops. But as the disease progresses, shortness of breath can overtake a person, even when he is at rest, and even just lying down. This is already a formidable symptom.
Cardiac dyspnea usually manifests itself as difficulty breathing.
A specialist can distinguish between cardiac and pulmonary shortness of breath. In any case, both symptoms indicate serious health problems.
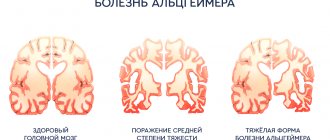
conclusions
The most common cause of death among men and women around the world is cardiac disease. The risk of developing heart disease especially increases in women after 50 years of age. Sometimes simple fatigue, lower back pain or indigestion are the first symptoms of heart disease in women. Therefore, it is so important to know what signs of cardiac pathology are manifested. Timely diagnosis and proper treatment not only affect life expectancy, but also its quality. To be confident in the health of your heart, you need to visit a cardiologist at least once every 2 years, and after 40 years, preventive examinations should become an annual ritual.
Working for a living
Continuous work of the heart - rhythmic contractions (systole), alternating with relaxations (diastole). During relaxation, the chambers fill with blood, and during contraction it is expelled.
- From the left ventricle, blood is pumped into the largest artery in the body, the aorta. Through it, blood flow is directed through organs and tissues, delivering oxygen.
- From them, blood moves through the veins and ends up in the right atrium.
The path taken is called the systemic circulation.
- From the right atrium, blood moves to the right ventricle. From there it is released into the pulmonary arteries and moves along them to the lungs. There, in the process of moving through the capillaries, it is enriched with oxygen and freed from carbon dioxide.
- The enriched blood arrives through the pulmonary veins into the left atrium.
This movement of blood flow, aimed at oxygen saturation, is called the pulmonary circulation.
- From the left atrium, blood enters the left ventricle. The movement is repeated again.
This is how the heart ensures the normal functioning of all systems and organs, saturating them with oxygen.
to contents ^