Heart defects are various anomalies of the valve apparatus, septa, large vessels and individual parts of the heart, causing circulatory disorders.
There are a huge number of heart defects, each of which is dangerous to human health in its own way. Almost always, a heart defect requires surgical intervention.
1 Holter - diagnosis of heart defects
2 Diagnosis of heart defects
3 ECG for heart defects
Structural pathology of the heart can begin to develop in a person in the mother's womb - this phenomenon is called congenital heart disease . The cause is usually chromosomal abnormalities or infections suffered by the mother. From 5 to 8 babies out of a thousand are born with this defect. The defect can be detected through fetal ultrasound.
If the disease appears as a consequence of injury, infection or systemic disease, we are talking about acquired heart disease .
At its core, the defect is a collective name for diseases of different parts of the heart. Both types of heart defects have many subtypes, with varying degrees of severity and consequences for human health.
Types of heart defects
In most cases, heart defects affect the valve apparatus. Complications that arise as a result of this pathology can cause early disability and even death.
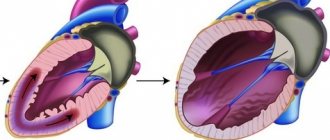
The main role of the valve apparatus is to freely pass blood through itself when the heart contracts and to delay the reverse movement of blood through the valve when relaxing, maintaining a rhythmic and continuous flow of blood. Defective valves cease to fully perform this work and function, which is why blood hardly flows through the narrowed valve into the cavity of the heart and does not fully leave the chambers or flows back through a closed valve.
Acquired heart defects:
- valve insufficiency (incomplete closure of the valves or damage to the valves) - causes reverse blood flow;
- valve stenosis (narrowing of the lumen between the open valves) - complicates blood circulation;
- prolapse (bulging) of the valve, as a result of which its leaflets bulge into the heart cavity, and often reverse blood flow occurs due to insufficient closure of the valve.
In cardiological practice, combined and associated defects are often encountered, in which several valves are affected at once.
Most often, the mitral (mitral heart disease) and aortic (aortic heart disease) heart valves suffer from abnormal changes.
Congenital heart defects:
- atrial septal defect;
- ventricular septal defect;
- patent ductus arteriosus;
- transposition (violation of position) of large great vessels;
- coarctation of the aorta;
- pulmonary stenosis, etc.
Congenital heart defects can occur either individually or in combination with each other. Thus, the combination of right ventricular hypertrophy, transposition of the aorta, ventricular septal defect and stenosis of the right ventricular outflow tract is called tetralogy of Fallot (or blue heart disease).
1 X-ray for heart defects
2 Diagnosis of heart defects using x-rays
3 Ultrasound for heart defects
Aortic insufficiency
Aortic insufficiency is a dysfunction of the aortic valve, in which the valves do not close completely and blood returns from the main vessel of the body - the aorta - back to the heart.
What is aortic insufficiency?
Aortic insufficiency can be congenital (due to impaired formation of the aortic valve during intrauterine development) and acquired (due to the effects of pathological processes, that is, diseases).
Why does it arise?
Normally, the aortic valve has 3 thin cusps, which, when opening, allow blood from the heart to the internal organs, and when closing, prevent blood from getting back into the heart and overloading it.
Quite often, as a result of a violation of intrauterine development, the aortic valve from birth may have only 2 leaflets, this leads to accelerated “aging” of the valve with the formation of a narrowing of its lumen and/or unevenness of the leaflets.
The second common cause of aortic insufficiency is infective endocarditis. This extremely dangerous disease is characterized by inflammation and destruction of vital structures of the heart with the formation of heart failure and vegetations (accumulations of colonies of microorganisms on destroyed heart structures). An absolutely healthy person can develop infective endocarditis against the background of complete well-being. It is worth noting that aortic valves with congenital malformations are most often affected by infection.
Everyone knows such a disease as atherosclerosis; it affects the vessels of all organs, as well as some structures of the heart. The aortic valve is an intravascular formation as it is located in the lumen of the main artery of the body, the aorta. When atherosclerotic plaques develop on the aortic valve, thickening of the leaflets may occur. Thickened valves lose elasticity and become covered with calcium salts, which leads to disruption of closure and backflow of blood.
Who can get sick
The disease is typical for patients of any age. Children are born with a bicuspid aortic valve, which makes them sick from birth; often the disease is detected when a dangerous complication occurs - infective endocarditis or dissection (dissection) of the aorta. ( Any age )
Atherosclerosis progresses with age in all people, causing the gradual formation of aortic insufficiency in a certain proportion of the population. ( Most typically from 45 to 70 years old )
A special group consists of patients with infective endocarditis. ( Any age )
What are the symptoms of the disease?
Aortic insufficiency is a disease in which no symptoms at all may occur for a long time; this is due to the compensatory capabilities of the body. In acute aortic insufficiency, symptoms appear at lightning speed and often lead to death in the first days of the disease.
The following complaints are typical for this disease:
- Shortness of breath during moderate physical activity (people around you may notice that you get tired more quickly)
- Palpitations, sensation of heart pulsation in the left side of the chest
- Interruptions in heart function
- Feeling of pulsation in the vessels of the whole body, head, fingertips. The pulsation of the vessels of the neck is especially noticeable.
- Dizziness when changing body position, or physical effort, stress.
- Late stages of the disease are characterized by sudden attacks of loss of consciousness
- Edema of the lower extremities
How is the diagnosis made?
Most often, when undergoing a professional examination, medical examination, or fluorography, doctors may notice significant deviations in the shape of the heart or changes in the electrocardiogram. An experienced cardiologist will always be able to hear a heart murmur characteristic of aortic insufficiency and will prescribe a number of studies:
- Electrocardiograms
- X-ray of the chest organs
- ECHO-cardiography (ultrasound of the heart)
- In difficult cases, multislice computed tomography with the introduction of a contrast agent is required.
This scope of research allows you to confirm or exclude the diagnosis, determine the stage of the disease and prognosis.
What are the stages of the disease?
Aortic insufficiency occurs:
- Easy
- Moderate
- Expressed
- Heavy
Who is treating?
It all depends on the cause, severity and presence of symptoms. Mild to moderate aortic insufficiency, not associated with infective endocarditis, and not accompanied by symptoms of heart failure, is observed by a cardiologist with periodic consultations with a cardiac surgeon.
If there are signs of infective endocarditis, treatment is carried out by a cardiac surgeon, regardless of the degree of damage and the presence of symptoms. Severe aortic insufficiency is treated by a cardiac surgeon. Treatment method: surgical replacement of the aortic valve, plastic surgery of the aortic valve, replacement of the ascending aorta.
What are the approaches to surgical treatment?
Depending on the stage of the disease, the patient’s age and many other factors, there are open surgical techniques and minimally invasive methods.
Each method has its own advantages and disadvantages.
Aortic valve replacement using an open technique under artificial circulation.
During open surgery, a longitudinal incision of the sternum and complete visualization of the heart are performed under artificial circulation. Then a heart-lung machine is connected, the heart stops, the altered heart valve is excised, and a prosthetic heart valve is securely sewn in its place.
Advantages of the method:
- Wide use
- This approach is considered excellent
- It is easy to influence complications that arise during surgery
Disadvantages of the method:
- Significant surgical trauma (scar length 20-25 cm).
- The need to sleep strictly on your back for 3 to 6 months.
Duration of the operation: from 3 to 6 hours.
In the intensive care unit: usually about 36 hours.
Total duration of hospitalization: 12-15 days.
Risk of intervention: about 1.5%
Aortic valve replacement from a mini-access under artificial circulation
This surgical correction option is characterized by a smaller incision, which is less traumatic for the patient. The course of the operation is similar to open surgery.
Advantages of the method:
- Less traumatic method
- Cut about 10 cm long
- Early rehabilitation
- There is no need to sleep on your back for long periods of time
Disadvantages of the method:
- Great technical complexity
- Limited ability to influence complications during surgery, or requires switching to a larger incision
Duration of the operation: from 2 to 8 hours.
In the intensive care unit: usually about 24 hours.
Total duration of hospitalization: 10-15 days.
Risk of intervention: more than 2%
Aortic valve plastic surgery
In rare cases in adults and quite often in children, the valve can be preserved by modifying its weak points surgically.
Advantages of the method:
- There is no need for lifelong use of anticoagulants, you continue to live with your own valve
Disadvantages of the method:
- It is difficult to predict the duration of the effective correction period
- Repeat surgery may be required if the valve ruptures again
Duration of the operation: from 3 to 8 hours.
In the intensive care unit: usually about 36 hours.
Total duration of hospitalization: 12-15 days.
Risk of intervention: moderate
What's the prognosis?
If you seek medical help in a timely manner, most patients, after successful surgical treatment, fully return to normal life within 3-6 months. People who work physically can return to work after 4-6 months; if the work does not involve physical effort, 6-8 weeks is often enough for rehabilitation. It should be understood that in each specific case the pace of rehabilitation is individual and depends on the patient’s age, the degree of “neglect” of the case, the presence of concomitant diseases, and complications during treatment.
I need to get examined! What are the stages?
1. Consultation with a cardiac surgeon.
After an in-person examination and a standard physical examination, it is possible with a high degree of probability to confirm or refute aortic stenosis.
Research will be conducted:
- Electrocardiography
- ECHO-cardiography (ultrasound of the heart)
If the diagnosis is confirmed, further examination is indicated before hospitalization in a specialized hospital.
- Determination of blood group, Rh factor
- Diagnosis of HIV, hepatitis B, C, syphilis
- General urine analysis
- General blood analysis
- Standard biochemical blood test
- X-ray of the chest organs, or fluorography
- Consultation with a urologist for men, a gynecologist for women
- Fibrogastroscopy
The main purpose of the examination before planned hospitalization is to exclude possible contraindications.
2. Hospitalization to a specialized hospital for further examination
In a hospital setting the following will be performed:
- Coronary angiography (men over 40 years old, women in menopause)
- Control ECHO-cardiography
- Examination with the participation of the head of the department or a professor as part of a council in order to determine the indications for surgical treatment and the choice of treatment tactics.
3. Discharge from the hospital with the exact date of hospitalization for surgical treatment if consent and indications are available.
4. Registration of a quota of high-tech medical care for surgical intervention.
5. Hospitalization for surgical treatment
6. Postoperative observation.
If you find yourself with similar symptoms, or your cardiologist suggests this diagnosis, do not hesitate, seek qualified medical help, we will conduct an examination on an outpatient basis, accompany hospitalization in a specialized hospital for high-tech additional examination and surgical treatment, and ensure proper monitoring after the operation.
Without surgical treatment of severe forms, the long-term prognosis for life is unfavorable. Patients die from acute myocardial infarction, sudden arrhythmic death, rupture of aortic aneurysm, aortic dissection, and progressive congestive heart failure.
Remember: aortic valve insufficiency is a structural change in the heart, cannot be cured by any drug, and if the cause is infective endocarditis, emergency surgery is often required!!!
Make an appointment now
Causes of heart defects
Causes of congenital defects (CHD):
- chromosomal and genetic abnormalities;
- infections suffered during pregnancy (for example, rubella, etc.);
- maternal alcoholism and drug addiction;
- side effects of medications;
- irradiation.
Causes of acquired defects:
- infectious, rheumatic endocarditis (rheumatic heart defects, chronic rheumatic heart disease, infective endocarditis - usually insufficiency of the aortic, mitral and tricuspid valves);
- systemic connective tissue diseases;
- heart injuries;
- sepsis;
- infectious diseases (especially syphilis);
- oncology.
Risk factors for developing heart defects
- hereditary predisposition (CHD);
- complications during pregnancy (CHP);
- taking medications (toxic to the fetus) during pregnancy (CHD).
1 Laboratory diagnostics for heart defects: tests
2 VEM for heart defects
3 ECHO-kg for heart defects
Symptoms of heart defects
The manifestations of the disease depend entirely on the severity of the lesion.
Thus, mild congenital and acquired defects in the early stages of development can occur unnoticed and have no effect on well-being. However, it should be remembered that severe congenital heart defects often affect the appearance, physical development and resistance of the body. Therefore, blueness or pallor of the skin, low height and weight, as well as a tendency to frequent colds may themselves be symptoms of the disease.
With acquired and congenital defects of moderate severity, obvious symptoms of heart failure appear (shortness of breath during exercise, swelling of the legs), dizziness, tachycardia, weakness, and fatigue.
Severe congenital (for example, blue heart disease) and acquired (valve insufficiency in combination with aortic stenosis) heart defects may be accompanied by symptoms of acute heart failure (asphyxia, pulmonary edema).
Common symptoms of heart disease:
- dyspnea;
- arrhythmia (usually tachycardia);
- cyanosis of the skin (blueness) or pallor;
- dizziness, weakness;
- swelling of the veins of the neck and head;
- decreased blood pressure;
- fainting.
1 Diagnosis of heart defects
2 Diagnosis of heart defects
3 Stress test for heart defects
What can an x-ray reveal?
An X-ray of the heart will provide a large amount of information regarding the position, size and condition of the organ and its structures. Based on these data, the doctor will be able to draw a conclusion about the presence of pathologies and identify the cause of the patient’s deterioration in well-being.
Heart sizes
An X-ray of the heart must be taken to find out whether the size of the organ is normal. They are very important in determining pathologies. The size is determined not by the width and length that are visible on an x-ray, but by the cardiothoracic index. To do this, you need to measure the width of the chest at the level of the fourth rib, and also find out the width of the heart in the same area. If the cell is twice as wide as the organ, the index will be 50%. If it is higher, then the heart muscle is enlarged. Myocardial hypertrophy may indicate ischemia or hypertension. Dilation of the chambers may be associated with cardiomyopathy or heart failure.
Condition of the great vessels
When thinking about what an X-ray of the heart shows, it is worth knowing that the condition of the great vessels will become known. The doctor will be able to find out if there are plaques, calcium deposits, or any lumps in the aorta. It will also be possible to identify a disease that is characterized by the accumulation of fluid in the pericardial sac. It is otherwise called “pericarditis”. If the fluid accumulates slowly, the organ becomes like a bag, but if it accumulates quickly, it becomes like a ball. If the condition is aggravated by calcium salt deposits, the doctor will diagnose constrictive pericarditis.
Diagnosis of heart defects
After talking with the patient, collecting complaints and physical examination, the cardiologist prescribes laboratory and hardware tests.
Methods for diagnosing heart defects:
- biochemical and clinical blood tests;
- electrocardiography (ECG);
- 24-hour Holter ECG monitoring;
- Ultrasound of the heart (ECHO-CG);
- chest x-ray;
- MSCT or MRI of the heart and large vessels;
- Transesophageal ECHO-CG.
Most of the listed diagnostic methods are also used to determine indications for surgical treatment of heart defects.
X-ray anatomy
If you need to take a picture, it is worth learning the x-ray anatomy of large vessels and the heart. The X-ray anatomy of this organ consists of its shadow, the pulmonary artery, the aorta, and the vena cava. 2/3 of the listed structures are located to the left of the midline of the chest, only 1/3 protrudes to the right side. Chest X-ray anatomy includes the lungs, bronchi and trachea.
There are several types of location of the heart shadow, depending on its angle and the patient’s constitution. Namely:
- vertical – the angle is more than 45 degrees;
- oblique – the angle is 45 degrees;
- horizontal – angle less than 45 degrees.
As X-rays of the heart show, the horizontal position is usually characteristic of women, and the vertical position is usually characteristic of tall people.
Treatment of heart defects
Drug treatment for heart defects is generally not considered effective. Therefore, therapy is aimed at antibacterial treatment for acute rheumatism, eliminating the manifestations of chronic rheumatic heart disease, heart failure and other severe complications. The only correct way to treat heart defects today is surgery.
Surgical methods for treating heart defects:
- valve replacement - in case of severe valve insufficiency and severe stenosis, the defective valve is replaced with an artificial one (there are mechanical and biological prosthetic heart valves);
- implantation of several prosthetic heart valves - for combined and combined defects;
- closing the atrial/ventricular septal defect - applying a suture or patch made of artificial material;
- ligation of the patent ductus arteriosus;
- X-ray surgery, transcatheter operations on the beating heart (closure of septal defects with Amplatzer, transcatheter implantation of the aortic valve - TAVI, application of a clip to the mitral valve leaflets in case of severe mitral valve insufficiency, closure of the patent ductus arteriosus, etc.).
In our clinic you can undergo diagnosis and treatment of heart defects. Our cardiologists are also knowledgeable in the outpatient management of patients with heart defects and in the outpatient management of patients with prosthetic heart valves.
Everything necessary for high-precision diagnosis of heart defects and other diseases of the heart and blood vessels is at the disposal of the cardiology department of the MedicCity clinic. You can undergo a full examination of the heart and blood vessels - ECG, ultrasound of the heart, bicycle ergometry, 24-hour blood pressure monitoring and ECG on a 12-channel holter at a convenient time by appointment.
Our clinic staff consists of only experienced specialists with serious scientific training and many years of medical practice!
Features of the procedure in children
Sometimes heart x-rays may be performed in children. This type of study is very rarely prescribed to children, since the procedure is contraindicated under 15 years of age. However, it may be required to identify heart defects, as well as when planning surgical interventions or to evaluate the effectiveness of the chosen treatment method. X-rays may also be needed to identify tumor processes.
If we are talking about a very young child, an X-ray of the heart will be taken using a special device. It is a stand on which the child is placed and his torso, head and limbs are secured with belts. This will ensure that the patient remains completely still while the doctor takes the image. The procedure will take no more than a couple of seconds, and discomfort is possible only from the belts with which the fixation is carried out. If we are talking about older children, they can undergo the procedure even without adults.