What is called pulse
When the heart muscles contract, the walls of the blood vessels vibrate in a certain rhythm and with a certain force.
These fluctuations are called the pulse, an indicator of the work of the heart and the condition of the blood vessels. Normally, there should be equal intervals between pulsations. Among the causes of disturbances in the rhythm of oscillations of the vascular walls:
- heart pathology
- problems with blood vessels
- endocrine system diseases
- intoxication
- tachycardia of a heavy smoker
- heavy physical activity
- trauma with blood loss
- acute cold
- severe stress, etc.
Any disturbance in heart contractions signals that something is wrong in the body. You should definitely consult a doctor. But first of all, learn how to measure your pulse correctly.
Pulse is an indicator of the work of the heart and blood vessels.
Providing first aid to victims
Photo: Victor Vasenin
The manual of the Ministry of Emergency Situations of Russia will help participants in road accidents and eyewitnesses of a heart attack in a sick person not to get confused in a difficult situation. The book also lists algorithms for providing first aid for traumatic injuries and emergency conditions. Such as external bleeding from injuries, abdominal wounds, penetrating chest wounds, bone fractures and thermal burns, as well as hypothermia and frostbite. Readers will learn how to behave correctly in order to actually help someone who has been electrocuted, or has swallowed water in a river, or perhaps has become a victim of serious poisoning. The manual also contains recommendations for help in case of injuries and chemical burns of the eyes, bites of poisonous snakes, insects, as well as heat and sunstroke.
Priority actions when providing first aid to sick and injured people
First of all, assistance is provided to those who are suffocating, who have profuse external bleeding, a penetrating wound to the chest or abdomen, who are unconscious or in serious condition.
| Make sure that you and the victim are not in danger. Use medical gloves to protect the victim from body fluids. Carry (lead) the victim to a safe area. |
| Determine the presence of a pulse, spontaneous breathing, and the reaction of the pupils to light. |
| Ensure patency of the upper respiratory tract. |
| Restore breathing and cardiac activity by using artificial respiration and chest compressions. |
| Stop external bleeding. |
| Apply a sealing bandage to the chest for a penetrating wound. |
Only after stopping external bleeding and restoring spontaneous breathing and heartbeat, do the following:
| Call (on your own or with the help of others) an ambulance. Apply an aseptic (clean) bandage to the wounds. |
| Ensure immobility of body parts at the fracture sites. |
| Apply cold to the sore spot (bruise, fracture, wound). |
| Place in a restorative position, protect from hypothermia, give a warm, salted or sweet drink (do not drink or feed in the absence of consciousness and abdominal injury). |
Procedure for performing cardiopulmonary resuscitation
2.1. Rules for determining the presence of a pulse, spontaneous breathing and the reaction of the pupils to light (signs of “life and death”)
| Determine the presence of a pulse in the carotid artery. (There is a pulse - the victim is alive.) |
| Listen to breathing, determine the presence or absence of chest movements. (There is movement of the chest - the victim is alive.) |
| Determine the reaction of the pupils to light by lifting the upper eyelid of both eyes. (The pupils narrow in the light - the victim is alive.) |
Proceed to resuscitation only if there are no signs of life (points 1-2-3).
2.2. Sequence of artificial ventilation
| Ensure patency of the upper respiratory tract. Using gauze (handkerchief), remove mucus, blood, and other foreign objects from the mouth using a circular motion of your fingers. |
| Tilt the victim's head back. (Lift your chin while holding the cervical spine.) Do not perform this if you suspect a fracture of the cervical spine! |
| Pinch the victim's nose with your thumb and forefinger. Using a device for artificial ventilation of the lungs of the “mouth-device-mouth” type, seal the oral cavity, make two maximum, smooth exhalations into his mouth. Allow two to three seconds for each passive exhalation of the victim. Check whether the victim’s chest rises when inhaling and falls when exhaling. |
2.3. Rules for closed (indirect) cardiac massage
| Determine the location of the xiphoid process, as shown in the figure. |
| Determine the point of compression two transverse fingers above the xiphoid process, strictly in the center of the vertical axis. |
| Place the heel of your palm on the compression point. |
| Apply compressions strictly vertically along the line connecting the sternum to the spine. Perform compressions smoothly, without sudden movements, using the weight of the upper half of your body. |
The depth of chest compression should be at least 3-4 cm, 100-110 compressions per minute.
| - For infants, massage is performed using the palmar surfaces of the second and third fingers; - for teenagers - with the palm of one hand; - in adults, the emphasis is placed on the base of the palms, the thumb is directed towards the head (legs) of the victim. The fingers are raised and do not touch the chest. |
| Alternate two “breaths” of artificial pulmonary ventilation (ALV) with 15 pressures, regardless of the number of people performing resuscitation. |
| Monitor the pulse in the carotid artery, the reaction of the pupils to light (determining the effectiveness of resuscitation measures). |
Closed cardiac massage should only be performed on a hard surface!
2.4. Removal of a foreign body from the respiratory tract using the Heimlich maneuver
Signs: The victim is suffocating (convulsive breathing movements), unable to speak, suddenly becomes cyanotic, and may lose consciousness.
Children often inhale parts of toys, nuts, and candies.
| Place the baby on the forearm of your left hand, and clap the palm of your right hand 2-3 times between the shoulder blades. Turn the baby upside down and pick him up by the legs. |
| Grab the victim from behind with your hands and clasp them in a “lock” just above his navel, under the costal arch. Press sharply with force - with your hands folded into a “lock” - into the epigastric region. Repeat the series of pressures 3 times. For pregnant women, apply pressure to the lower parts of the chest. |
| If the victim is unconscious, sit on top of the hips and sharply press on the costal arches with both palms. Repeat the series of pressures 3 times. |
| Remove the foreign object with your fingers wrapped in a napkin or bandage. Before removing a foreign body from the mouth of a victim lying on his back, he must turn his head to the side. |
IF, DURING RESUSCIVATION, INDEPENDENT BREATHING, HEARTBEAT DOES NOT RECOVER, AND THE PUPILS REMAIN WIDE FOR 30-40 MINUTES AND THERE IS NO HELP, IT SHOULD BE CONSIDERED THAT THE BIOLOGICAL DEATH OF THE VICTIM HAS OCCURRED.
Algorithms for providing first aid to victims of traumatic injuries and emergency conditions
3.1. First aid for external bleeding
| Make sure that neither you nor the victim is in danger, put on protective (rubber) gloves, and take the victim out of the affected area. |
| Determine the presence of a pulse in the carotid arteries, the presence of spontaneous breathing, and the presence of pupillary reaction to light. |
| If there is significant blood loss, place the victim with his legs elevated. |
| Stop the bleeding! Call (on your own or with the help of others) an ambulance. |
| Apply a (clean) aseptic dressing. |
| Keep the injured part of the body immobile. Place a cold pack (ice pack) on the bandage over the wound (sore area). |
| Place the victim in a stable lateral position. |
| Protect the victim from hypothermia by giving plenty of warm, sweet drinks. |
Pressure points of arteries
| 1. Temporal 2. Maxillary 3. Carotid 4. Radial 5. Brachial 6. Axillary 7. Femoral 8. Tibial On the extremities, the point of pressure of the artery to the bone should be above the site of bleeding. On the neck and head - below the wound or in the wound (press with your finger). |
3.2. Methods for temporarily stopping external bleeding
Clamp the bleeding vessel (wound)
| The artery should be pressed firmly with the flesh of two to four fingers or a fist against nearby bone formations until the pulse disappears. |
Finger pressure on the artery is painful for the victim and requires great endurance and strength from the person providing assistance. Before applying a tourniquet, do not release the pinched artery so that bleeding does not resume. If you start to get tired, ask someone present to press your fingers on top.
Apply a pressure bandage or pack the wound
| While holding the vessel clamped, apply a pressure bandage made from folded aseptic (clean) napkins or several tightly rolled layers of gauze bandage. Wound tamponade: tightly “stuff” a sterile bandage, towel, etc. into the wound, then bandage it to the wound. |
| If the pressure bandage gets wet, place a few more tightly folded tissues on top of it and press firmly with your palm over the bandage. |
Apply a hemostatic tourniquet
A tourniquet is a last resort measure to temporarily stop arterial bleeding.
| Place a tourniquet on a soft pad (elements of the victim’s clothing) above the wound as close to it as possible. Place the tourniquet under the limb and stretch. |
| Tighten the first turn of the tourniquet and check the pulsation of the vessels below the tourniquet or make sure that the bleeding from the wound has stopped and the skin below the tourniquet has turned pale. |
| Apply subsequent turns of the tourniquet with less force, applying them in an upward spiral and capturing the previous turn. |
| Place a note indicating the date and exact time under the tourniquet. Do not cover the tourniquet with a bandage or splint. In a visible place - on the forehead - make the inscription “Tourniquet” (with a marker). |
The duration of the tourniquet on the limb is 1 hour, after which the tourniquet should be loosened for 10-15 minutes, having previously clamped the vessel, and tightened again, but not more than for 20-30 minutes.
Stopping external bleeding with a tourniquet (a more traumatic way to temporarily stop bleeding!)
| Place a tourniquet (tourniquet) made of narrowly folded available material (fabric, scarf, rope) around the limb above the wound on top of clothing or placing the fabric on the skin and tie the ends with a knot so that a loop is formed. Insert a stick (or other similar object) into the loop so that it is under the knot. |
| Rotating the stick, tighten the tourniquet (tourniquet) until the bleeding stops. |
| Secure the stick with a bandage to prevent it from unwinding. Every 15 minutes, loosen the tourniquet to avoid necrosis of the limb tissue. If bleeding does not return, leave the tourniquet loose, but do not remove it in case rebleeding occurs. |
3.3. First aid for abdominal wounds
| Prolapsed organs should not be placed into the abdominal cavity. Drinking and eating are prohibited! To quench your thirst, wet your lips. |
| Place a roll of gauze bandages around the prolapsed organs (to protect the prolapsed internal organs). |
| Apply an aseptic bandage over the rollers. Without pressing the prolapsed organs, apply a bandage to the abdomen. |
| Apply cold to the bandage. |
| Protect the victim from hypothermia. Wrap yourself in warm blankets and clothes. |
Call (on your own or with the help of others) an ambulance and ensure that the victim is transported to a medical facility.
3.4. First aid for penetrating chest wounds
Signs: bleeding from a wound on the chest with the formation of blisters, air being sucked through the wound.
| If there is no foreign object in the wound, press your palm against the wound and close the access of air to it. If the wound is through, close the entry and exit wound holes. |
| Cover the wound with an airtight material (seal the wound), secure this material with a bandage or plaster. |
| Place the victim in a half-sitting position. Apply cold to the wound using a cloth pad. |
| If there is a foreign object in the wound, secure it with bandage rolls, a plaster or a bandage. It is prohibited to remove foreign objects from the wound at the scene of the incident! |
Call (on your own or with the help of others) an ambulance and ensure that the victim is transported to a medical facility.
3.5. First aid for nosebleeds
Causes: nose injury (blow, scratch); diseases (high blood pressure, decreased blood clotting); physical stress; overheating.
| Sit the victim down, tilt his head slightly forward and let the blood drain. Squeeze your nose just above your nostrils for 5-10 minutes. In this case, the victim must breathe through his mouth! |
| Invite the victim to spit out the blood. (If blood enters the stomach, vomiting may occur.) |
| Apply cold to the bridge of your nose (wet handkerchief, snow, ice). |
| If the bleeding from the nose does not stop within 15 minutes, insert rolled gauze swabs into the nasal passages. |
If the bleeding does not stop within 15-20 minutes, refer the victim to a medical facility.
3.6. First aid for broken bones
| Make sure that neither you nor the victim is in danger, take (take) the victim out of the affected area. |
| For open fractures, first stop external bleeding. |
| Ensure that the site of bone fractures is immobilized using splints or improvised means (a branch, a board) over clothing. |
Call (on your own or with the help of others) an ambulance.
| Apply an aseptic bandage to the wound. With an open fracture. |
| Place a cold pack (ice pack) on the bandage over the wound (sore area). |
| Wrap the victim in a warm (rescue) blanket and clothing. |
3.7. Rules for immobilization (immobilization)
Immobilization is mandatory. Only if there is a threat to the injured rescuer is it permissible to first move the injured person to a safe place.
| Immobilization is performed by immobilizing two adjacent joints located above and below the fracture site. |
| Flat, narrow objects can be used as an immobilizing agent (splint): sticks, boards, rulers, rods, plywood, cardboard, etc. The sharp edges and corners of the splints should be smoothed using improvised means. After application, the splint must be secured with bandages or adhesive tape. For closed fractures (without damaging the skin), a splint is applied over clothing. |
| For open fractures, do not apply a splint to places where bone fragments protrude. |
| Attach the splint along its entire length (excluding the level of the fracture) to the limb with a bandage, tightly, but not too tightly, so as not to interfere with blood circulation. In case of a fracture of the lower limb, apply splints on both sides. |
| In the absence of splints or available means, the injured leg can be immobilized by bandaging it to the healthy leg and the arm to the body. |
3.8. First aid for thermal burns
| Make sure you are not in danger. Stop (knock down) the victim. |
| Extinguish burning clothing in any way (cover the person with a blanket). |
Call (on your own or with the help of others) an ambulance. Ensure that the victim is transported to the burn department of the hospital.
| Carry (take) the victim out of the affected area. Irrigate the burn site with alcohol diluted with water (1:1), vodka for 2-3 minutes (cooling, disinfection, anesthesia), then with cold water for 15-30 minutes. |
| Do not open blisters, cut off any stuck clothing around the burn wound! Do not remove foreign objects or stuck clothing from the wound! Apply a sterile bandage to the burn area and apply ice over the bandage. Give plenty of warm, salted drink (mineral water). |
3.9. First aid for general hypothermia
| Carry (take) the victim out of the affected area, ensuring your own safety. |
| Take the victim into a warm room or warm the victim (wrap the victim in a warm (rescue) blanket, clothing). |
Call (on your own or with the help of others) an ambulance.
| If the victim is conscious, give plenty of hot, sweet drinks. Feed him hot food. The use of alcohol is prohibited! |
If there are signs of your own hypothermia, fight sleep, move; use paper, plastic bags and other means to insulate your shoes and clothes; look for or build a shelter from the cold.
3.10. First aid for frostbite
| Bring the victim into a warm room. |
| Wrap frostbitten areas of your body in several layers. External warming of frostbitten parts of the body should not be accelerated. Warmth should arise inside with the restoration of blood circulation. |
In case of frostbite, use oil or Vaseline; rubbing frostbitten areas of the body with snow is prohibited.
| Wrap the victim in blankets and, if necessary, change into dry clothes. |
| Give plenty of hot sweet drinks. Feed him hot food. |
Call (on your own or with the help of others) an ambulance and ensure that the victim is transported to a medical facility.
3.11. First aid for electric shock
| Ensure your safety. Put on dry gloves (rubber, wool, leather, etc.) and rubber boots. If possible, turn off the power source. When approaching the victim on the ground, walk in small steps, no more than 10 cm. |
| Remove the wire from the victim with a dry, non-conductive object (stick, plastic). Drag the victim by his clothes at least 10 meters from the point where the wire touches the ground or from live equipment. |
Call (on your own or with the help of others) an ambulance.
| Determine the presence of a pulse in the carotid artery, the reaction of the pupils to light, and spontaneous breathing. |
| If there are no signs of life, perform cardiopulmonary resuscitation. |
| When spontaneous breathing and heartbeat are restored, place the victim in a stable lateral position. |
| If the victim regains consciousness, cover and warm him. Monitor his condition until medical personnel arrive; repeated cardiac arrest may occur. |
3.12. First aid for drowning
| Make sure you are not in danger. Remove the victim from the water. (If you suspect a fracture of the spine, pull the victim out on a board or shield.) |
| Lay the victim on his stomach on your knee, let the water drain from the respiratory tract. Ensure patency of the upper respiratory tract. Clear the oral cavity of foreign objects (mucus, vomit, etc.). |
Call (on your own or with the help of others) an ambulance.
| Determine the presence of a pulse in the carotid arteries, the reaction of the pupils to light, and spontaneous breathing. |
| If there is no pulse, breathing or reaction of the pupils to light, immediately begin cardiopulmonary resuscitation. Continue resuscitation until medical personnel arrive or until spontaneous breathing and heartbeat are restored. |
| After restoring breathing and cardiac activity, place the victim in a stable lateral position. Cover and warm him. Ensure constant monitoring of the condition. |
3.13. First aid for traumatic brain injury
| Stop the bleeding. Press the sterile cloth firmly onto the wound. Hold it with your fingers until the bleeding stops. Apply cold to your head. |
Call (on your own or with the help of others) an ambulance.
| Monitor the presence of a pulse in the carotid arteries, spontaneous breathing, and the reaction of the pupils to light. |
| If there is no pulse in the carotid arteries, no reaction of the pupils to light, no spontaneous breathing, perform cardiopulmonary resuscitation until spontaneous breathing and heartbeat are restored or until medical personnel arrive. |
| After restoring breathing and cardiac activity, place the victim in a stable lateral position. Cover and warm him. Ensure constant monitoring of his condition. |
3.14. First aid for poisoning
3.14.1. First aid for oral poisoning (when a toxic substance enters the mouth)
Call an ambulance immediately. Find out the circumstances of the incident (in case of drug poisoning, present the medicine wrappers to the arriving medical worker).
If the victim is conscious
| Provide gastric lavage. Let's drink a glass of clean water at a temperature of 18-20 C. For one liter of water, it is advisable to add a dessert spoon of salt (10 g) and a teaspoon of baking soda (5 g). After drinking every 300-500 ml of water, you should induce vomiting by touching the root of the tongue with your fingers. The total volume of liquid taken during gastric lavage should be at least 2500-5000 ml. Gastric lavage is carried out until the “clean lavage waters”. If you are unconscious, do not rinse your stomach! |
| Dissolve 10-20 tablets of activated carbon in a glass of water until it becomes a paste. Give the victim something to drink (as an absorbent). |
If the victim is unconscious
| Determine the presence of a pulse in the carotid arteries, the reaction of the pupils to light, and spontaneous breathing. |
| If there is no pulse, breathing, or pupillary response to light, begin CPR immediately. |
| Place the victim in a stable lateral position. |
| Wrap the victim in warm blankets and clothes. |
Call (on your own or with the help of others) an ambulance and ensure that the victim is transported to a medical facility.
3.14.2. First aid for inhalation poisoning (when a toxic substance enters the respiratory tract)
Signs of carbon monoxide poisoning:
pain in the eyes, ringing in the ears, headache, nausea, vomiting, loss of consciousness, redness of the skin.
Signs of household gas poisoning:
heaviness in the head, dizziness, tinnitus, vomiting; severe muscle weakness, increased heart rate; drowsiness, loss of consciousness, involuntary urination, pale (blue) skin, shallow breathing, convulsions.
| Make sure that neither you nor the victim is in danger, take the victim to a safe place or open the windows and ventilate the room. |
Call an ambulance.
| Determine the presence of a pulse in the carotid arteries, the presence of pupillary reaction to light, and spontaneous breathing. |
| If there is no pulse, breathing or reaction of the pupils to light, immediately begin cardiopulmonary resuscitation. |
| When spontaneous breathing and heartbeat are restored, place the victim in a stable lateral position. |
Algorithms for providing first aid for acute diseases and emergencies
4.1. First aid for a heart attack
Signs:
acute pain behind the sternum, radiating to the left upper limb, accompanied by “fear of death,” palpitations, shortness of breath.
| If the patient is unconscious, determine the presence of a pulse in the carotid arteries, the reaction of the pupils to light, and spontaneous breathing. |
| Determine the presence of a heartbeat, spontaneous breathing, and the reaction of the pupils to light. If not available, proceed with cardiopulmonary resuscitation. |
Call and instruct others to call an ambulance. Provide fresh air, unfasten tight clothes, and give a semi-sitting position.
4.2. First aid for damage to the organs of vision
4.2.1. If foreign bodies enter
| Rinse your eye generously with clean water (preferably at room temperature). Rinse so that water does not get into the uninjured eye. |
| Place (if possible) two drops of 30% sodium sulfacyl solution (albucid) into each eye. |
| If it is impossible to remove the foreign body, apply a bandage to both eyes (if you do not cover both eyes with a bandage, then movements of the healthy eye will cause movement and pain in the affected eye). Contact a medical facility immediately. |
The victim should only move hand in hand with an accompanying person!
Ensure that the victim is transported to a medical facility.
4.2.2. For chemical burns to the eyes
| Gently spread your eyelids with your fingers and rinse your eyes generously with clean water (preferably at room temperature). Rinse your eyes so that the water flows from your nose to your temple. |
| Apply a bandage to both eyes (if you do not cover both eyes with a bandage, movements of the healthy eye will cause movement and pain in the affected eye). Contact a medical facility immediately. |
The victim should only move hand in hand with an accompanying person!
In case of acid contact
You can wash your eyes with a 2% solution of baking soda (add baking soda to a glass of boiled water on the tip of a table knife).
In case of contact with alkali
you can wash your eyes with a 0.1% solution of citric acid (add 2-3 drops of lemon juice to a glass of boiled water).
4.2.3. For eye and eyelid injuries
The victim should be in a lying position
| Place (if possible) two drops of 30% sodium sulfacyl solution (albucid) into each eye. |
| Apply a bandage to both eyes (if you do not cover both eyes with a bandage, movements of the healthy eye will cause movement and pain in the affected eye). The victim should only move hand in hand with an accompanying person! |
Ensure that the victim is transported to a medical facility.
4.3. First aid for poisonous snake bites
Limit the mobility of the affected limb.
| If a leg is bitten, tape it to the other leg. |
| If your hand is bitten , secure it in a bent position. |
| If the heart and breathing stop, begin cardiopulmonary resuscitation. |
Ensure that the victim is transported to a medical facility for administration of anti-snake serum.
4.4. First aid for insect bites
| If an insect bites you, remove the sting from the wound. |
| Apply cold to the bite site. |
If an allergic reaction occurs, consult a doctor. Monitor the patient's condition until a medical professional arrives.
4.5. First aid for fainting
Signs:
pallor, sudden short-term loss of consciousness.
| Lay the victim on his back with his legs elevated, loosen his tie, unbutton the collar of his outerwear, loosen his trouser belt, take off his shoes, and provide access to fresh air. Consult a doctor for examination and determination of the cause of fainting. |
If consciousness does not recover for more than 3-5 minutes, call (on your own or with the help of others) an ambulance.
4.6. First aid for heatstroke (sunstroke)
Signs:
weakness, drowsiness, thirst, nausea, headache; increased breathing and increased temperature, loss of consciousness are possible.
| Move the victim to a cool, ventilated place (in the shade, to an open window). |
| Lay the victim down. Unbutton your collar, loosen your belt, take off your shoes. |
| Determine the presence of a pulse in the carotid arteries, spontaneous breathing, and the reaction of the pupils to light. |
If these signs are absent, proceed with cardiopulmonary resuscitation.
| Place towels (napkins) soaked in cold water on your head, neck and groin areas. |
| If loss of consciousness lasts more than 3-4 minutes, turn the victim into a stable lateral position. |
| During convulsions, hold the victim’s head and torso, protecting from injury. |
| When consciousness is restored, give the victim cool mineral or ordinary, slightly salted water. |
Call (by yourself or with the help of others) an ambulance
.
How to measure your pulse manually
- The subject of measurement is the number of pulsations per minute, at rest. For more accurate calculations, use a stopwatch.
- Manual pulse measurements are usually taken from the inside of the wrists of the left and right hands, more precisely, in the area of the radial artery, close to the skin - at the base of the thumb.
- With rhythmic pulsations, you can count how many beats (oscillations of the vascular walls) there were in 30 seconds and double the result.
- For non-rhythmic pulsations, it is recommended to count the beats for a minute.
- In some cases, it is possible to measure the pulse in the area of other arteries located close to the skin on the neck (posterior edge of the sternocleidomastoid muscle), temple, thigh, elbow, under the collarbone, in the groin at the edge of the pubis.
How to measure the pulse on your hand yourself
To independently measure your pulse on your arm you need:
- Unbutton or remove clothing that is constricting your left arm.
- Take a comfortable position in a chair or at a table (the left hand and forearm should have support, be closer to the heart, palm facing up).
- With the fingers of your right hand, grasp the wrist joint of your left so that the index, middle and ring fingers are on top, and the thumb is on the bottom.
- A pulsation will be felt under three fingers closer to the base of the palm and thumb of the left hand.
- Turn on the stopwatch and count the beats for 1 minute.
Watch this video on how to correctly measure your own pulse:
On which hand?
It makes no difference which hand you use to measure your pulse. In most people it is completely identical on both upper limbs. If there are differences in filling or frequency, this may be a sign of severe vascular disease:
- atherosclerotic changes in arteries;
- aneurysm (protrusion of the wall) of the aorta;
- aortic pathologies – narrowing above the valve, coarctation;
- arteritis (inflammation of the artery) Takayasu (pulselessness disease).
Method of assessing pulse for an adult
When studying the pulse of an adult, it is necessary to adhere to the method of sequential determination of characteristics:
- frequency (counting per minute);
- rhythmicity (the number of beats for every 10 seconds should be equal);
- filling (the pulse wave is clearly noticeable on the wrist);
- tension (reflects arterial tone);
- uniformity - all blows are of the same force.
If it's hard to find on your wrist
If it is difficult to find a pulse in the wrist, this is a sign of heart failure, low blood pressure, or narrowing of the arteries of the upper extremities. In this case, it is recommended to count the number of heartbeats in the neck (on the carotid artery) or on the chest under the left mammary gland.
Pulse measurement with a tonometer
You can conveniently and quickly measure fluctuations in the vascular walls using a special electronic tonometer, which displays blood pressure and pulse indicators on the screen. Depending on the type of model, it can be worn on the wrist or shoulder.
For an untrained adult, a normal heart rate is considered to be between 60 and 80 beats per minute.
It is necessary to strictly follow the instructions for the device. Regardless of the type of tonometer, when measuring your pulse, follow the following important rules:
- do calculations at rest, being relaxed
- take a sitting position
- empty your bladder beforehand
- an hour before measurement, do not consume caffeine, alcohol, or nicotine
- keep your elbow approximately at heart level
- If you want to measure your pulse again, do so after at least 5 minutes.
Remember that when a serious illness is detected, the doctor will not limit himself to simply counting the pulse and recommends more in-depth examinations, for example, undergoing an electrocardiography procedure or doing a so-called treadmill test, that is, a study of the functioning of the heart and blood vessels on a treadmill.
A tonometer will help you accurately determine your heart rate.
How to measure your pulse in 10 seconds
To measure your pulse in 10 seconds, you need:
- Feel the pulse on the radial artery of the arm or carotid artery (on either side).
- Start the stopwatch for 10 seconds.
- Start counting from the first beat until the signal.
The result obtained must be multiplied by 6. This method is not suitable for determining the pulse rate in diseases, because the measurement error can be from 10 to 16 beats per minute. Athletes use this technique to find out whether the selected load corresponds to the training interval.
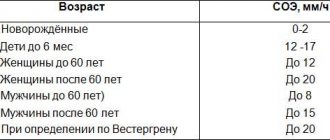
Normal heart rate in adults and children
Heart rate can depend not only on diseases, but also on many other factors. In particular, on gender and age, body weight and temperature, diet and even the environment. For example, people who are professionally involved in sports have a faster heart rate than untrained people; The pulse quickens in the afternoon and slows down at night.
In order for anyone to determine whether their pulse is normal, they should first take into account their age.
The norm for children is:
- in newborns - from 110 to 160 beats per minute
- in infants from 1 month to 1 year – from 100 to 150
- children from 3 to 8 years old – from 70 to 125
- children from 9 to 11 years old – from 60 to 100
- teenagers from 12 to 15 years old – from 55 to 95
in adults:
- up to 50 years – from 64 to 84
- up to 60 years – from 64 to 84
- after 60 – from 69 to 89
Slow and fast heartbeat
The heart muscle can contract at an increased (tachycardia) or decreased (bradycardia) rhythm. If the pulse does not correspond to the norm, there is no need to immediately sound the alarm: the reason may be not only in pathology, but also in the physiology of the female or male body. Thus, some increase in heart rate is observed when women reach menopause, or when estrogen levels decrease; slowing of the pulse - when taking certain medications.
Various physical and mental stress affect the heart rate, even the difficult digestion process after a heavy holiday dinner and the use of energy drinks. Typically, physiological causes of abnormal heart rate are temporary. After 45 minutes, the pulse readings can return to normal.
Record your heart rate readings on both hands - this will allow you to get more accurate data when measuring this indicator manually.
Clinical practice shows that the pulse often increases when the nervous system is damaged, cardiac pathology, or hormonal system disorders. It is possible that with high readings a tumor or some kind of infection develops in the body.
The pulse slows down if the body experiences intoxication, peptic ulcer disease, or increased intracranial pressure, myocardial infarction develops. Perhaps this signals a lack of thyroid hormones, organic damage to the heart, or poor oxygen supply to tissues.
Only a specialist can answer the question why your pulse is too fast or too rare. In any case, consult a doctor immediately if your pulse is abnormal:
- dyspnea
- my head is spinning
- fainting or presyncope
- heart pain
- vision problems
When playing sports, it is important to regularly measure your pulse.