Pulmonary embolism (PE) is a serious, potentially life-threatening condition. Pulmonary embolism occurs due to blockage of blood vessels by thrombotic masses in the lungs. Pulmonary embolism (PE) can cause symptoms such as chest pain and/or shortness of breath. Also, in some cases, PE may have no symptoms at all, and it is difficult to detect without specialized examination. Massive pulmonary embolism can cause collapse and death. PE usually occurs due to the formation of a thrombosis in the lower extremity - deep vein thrombosis (DVT).
Pulmonary embolism (PE)
Prompt treatment is important and can save lives. Pregnancy, various medical conditions and medications, immobility, and major surgery all increase the risk of PE. Anticoagulant therapy, including heparin drugs, direct oral anticoagulants, or warfarin, is the usual treatment for PE.
Venous thromboembolic complications
Pulmonary embolism (PE) is part of a group of clinical problems collectively known as venous thromboembolic events (VTE).
Thrombosis is the blockage of a blood vessel by a blood clot (thrombus). Embolisms occur when part or all of a blood clot displaces from where it formed. The thrombotic masses then move with the bloodstream until they get stuck in narrower blood vessels in other parts of the body. In this case, the blood clot is called an embolus. Deep vein thrombosis (DVT) is the cause of venous thromboembolism, including pulmonary embolism (PE). Thrombosis most often occurs in the veins of the lower extremities.
What causes pulmonary embolism?
The usual cause of pulmonary embolism is deep vein thrombosis (DVT).
In almost all cases, the cause is a blood clot (thrombosis) that originally formed in a deep vein of the lower limb (known as deep vein thrombosis). This clot travels through the circulation and eventually becomes lodged in one of the lung's blood vessels. The broken thrombus is now called an embolus (and therefore can cause an embolism). Most deep vein thromboses arise from the veins of the legs or pelvis. Sometimes PE can occur from a blood clot in a vein in the arm or from a blood clot that forms in the heart. However, these situations are quite rare.
Other causes of pulmonary embolism
In rare cases, a blockage of a blood vessel in the lung may be caused by an embolus, which is not a blood clot. It could be:
- Fatty tissue from the bone marrow of a broken bone (if a large long bone such as a femur is broken).
- Foreign material from unsterile injection - for example, due to drug abuse.
- Amniotic fluid during pregnancy or childbirth (rare).
- Entry of a significant volume of air into the vein (rare).
- A small fragment of cancerous material (tumor) that has broken off from a larger tumor in a different location.
- Mycotic emboli are material from the focus of a fungal infection.
Who develops pulmonary embolism?
Almost all cases of pulmonary embolism are caused by deep vein thrombosis. Thus, people who are more likely to get pulmonary embolism are people who are prone to deep vein thrombosis. Let's look at some risk factors for pulmonary embolism. Important factors are immobility, severe somatic pathologies and major surgical intervention (especially gynecological operations, operations on the pelvis and lower extremities). The risk of developing deep vein thrombosis or PE in hospital can be significantly reduced by activating the patient to walk as soon as possible. Medicines to help prevent deep vein thrombosis and PE are also prescribed to those patients who are at high risk.
Contraindications to CT angiography of the pulmonary arteries
If the patient is pregnant or suspects that she may be pregnant, the doctor must be notified about this, because CT angiography can harm the fetus. CT angiography is also not recommended for women who are currently breastfeeding.
In addition, there is a risk of allergies if there is an individual intolerance to the components of the contrast agent. Patients who experience an allergic reaction to iodine should inform their doctor. Patients suffering from renal failure or other kidney diseases should also tell their radiologist in advance. In addition, the doctor should not be left in the dark if the patient is taking medications and herbal supplements. Contraindications to CT are people with elevated creatinine levels, diabetes mellitus (type II), thyrotoxicosis, and blood clotting problems.
Symptoms of pulmonary embolism
Symptoms of pulmonary embolism will depend on how large or small the clot is and how well a person's lungs can handle the clot. Frail or already ill people will have more severe symptoms than relatively healthy people. Symptoms of pulmonary embolism often occur suddenly.
A small pulmonary embolism can cause the following symptoms:
- Be asymptomatic (often).
- Shortness of breath - The degree of shortness of breath can range from very mild to severe.
- Chest pain, which is pleuritic in nature, that is, acute pain is felt when inhaling. Often you feel like you can't breathe deeply because it forces you to catch your breath. This happens because the blood clot can irritate the lining (pleura) around the lung. Shallow breathing is more comfortable for such patients.
- Coughing up blood (hemoptysis).
- Increased body temperature (from low-grade fever to fever).
- Increased heart rate (tachycardia).
A large pulmonary embolism or large number of clots (multiple embolism) may cause the following symptoms:
- Severe shortness of breath.
- Chest pain – With a massive pulmonary embolism, pain may be felt in the center of the chest behind the sternum.
- Confusion, feeling unwell, or fainting. This is because a large blood clot interferes with the heart and circulation, causing a sharp drop in blood pressure.
- Rarely and in extreme cases, a massive pulmonary embolism can cause cardiac arrest, when the heart stops pumping due to a blood clot. This may result in death even if resuscitation is attempted.
- Symptoms of deep vein thrombosis may occur, such as pain in the back of the leg, tenderness of the calf muscles, or swelling of the leg or foot.
Massive pulmonary embolism is so called not because of the actual large size of the blood clot (embolus), but because of the magnitude of its effect. PE is high risk if it causes serious problems, such as collapse or a drop in blood pressure. Major thromboembolism is by definition associated with a high risk.
Massive pulmonary embolism kills approximately 1 in 7 people.
Treatment of pulmonary hypertension
Therapy depends on the cause that led to the development of pulmonary hypertension. It must be remembered that the pressure in the pulmonary artery may exceed normal due to the following factors:
- physical exercise
- hypothermia
- pregnancy
- stay in the highlands
The condition of a person with pulmonary hypertension can be alleviated by inhaling oxygen. But it is contraindicated for those who have right-to-left shunting and arterial hypertension.
In chronic nonspecific lung diseases, pulmonary hypertension can be reduced with the help of such medications6
- slow calcium channel blockers
- aminophylline
- nitrates
But they do not affect the life expectancy of people with PH, which was proven by studies no more than 20-30 years ago. It is possible to reduce PH and increase life expectancy with long-term low-flow oxygen therapy.
Taking diuretics reduces the severity of right ventricular failure. But when prescribing, some caution is needed, because in patients with pulmonary hypertension, large diuresis can reduce the preload on the right ventricle and cardiac output will decrease. A relevant drug is furosemide, which is prescribed at a dose of 20-40 mg per day. Taken orally. Hydrochlorothiazide is also effective at a dose of 50 mg/day orally.
Slow calcium channel blockers are used to reduce pulmonary artery pressure in patients with established pulmonary hypertension. The effect is exerted by nifedipine at a dose of 30-240 mg/day or diltiazem at a dose of 120-900 mg/day.
Cardiac glycosides are not effective drugs for the treatment of patients with PH. They can be used in small doses for atrial fibrillation to slow the heart rate. It should be taken into account that in patients with PH, glycoside intoxication develops faster as a result of hypoxemia and hypokalemia during diuretic therapy.
If drug treatment does not produce results, lung or heart-lung transplantation is recommended.
How is pulmonary embolism diagnosed?
The diagnosis is based on clinical symptoms and medical history. For example, if a bedridden patient undergoing major surgery in a hospital develops shortness of breath, it is likely to be a pulmonary embolism.
Pregnant women who experience symptoms and/or signs suggestive of PE should be hospitalized immediately, as pulmonary embolism during pregnancy is a very serious condition and requires prompt diagnosis and treatment. For other patients, the Wells score is used to decide whether hospitalization is necessary. This allows you to assess the risk of developing pulmonary embolism, taking into account the following clinical signs:
- Clinical features of deep vein thrombosis.
- Heart rate more than 100 beats per minute.
- Immobilization for more than three days or surgery in the previous four weeks.
- Previous deep vein thrombosis and pulmonary embolism.
- Coughing up blood (hemoptysis).
- Treatment of cancer over the past six months.
- The alternative diagnosis is less likely than PE. Example: pneumothorax, pneumonia, myocardial infarction or gastroesophageal reflux.
If the likelihood of pulmonary embolism is high, emergency hospitalization of the patient is necessary. Various tests will be used to confirm the diagnosis. These may include the following activities:
Duplex ultrasound scanning of the veins of the lower extremities
This study is used to determine blood flow disorders in the veins of the lower extremities. Lower extremity ultrasound is a simple, non-invasive test that can detect deep vein thrombosis. If DVT is detected, it can be assumed that the cause of other symptoms (such as shortness of breath or chest pain) was a pulmonary embolism. It is better to start treatment with anticoagulants immediately both in cases of deep vein thrombosis and in cases of suspected pulmonary embolism. If thrombotic masses are detected in the veins of the lower extremities, further studies may not be required. However, if the ultrasound results are negative, both deep vein thrombosis and pulmonary embolism cannot always be excluded. Further clinical studies will be required.
D-dimer blood test
This test detects fragments of the breakdown products of a thrombotic blood clot. The higher the level, the greater the likelihood of a blood clot forming in the vein. Unfortunately, the test can be positive in a number of other situations, such as if you have recently had surgery or are pregnant. Therefore, a positive result does not diagnose DVT or PE. However, in a complex of studies, this test can show how likely the presence of thrombosis is. To some extent, this may help decide whether further research is needed. A negative D-dimer result with a low risk of thrombosis means that the likelihood of a blood clot is extremely low. However, if your risk of venous thromboembolism is high, the D-dimer test cannot rule out the possibility of a blood clot and you will need further testing.
Ultrasound scan of the heart (echocardiography)
Echocardiography is useful for patients who may have massive PE, as it can show the effect on the heart. If there is massive PE, this puts stress on the right side of the heart. This test can be performed at the patient's bedside.
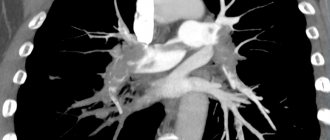
Computed tomography of the lungs with blood flow contrast
This is a specialized test that examines blood circulation in the lungs. This technique is the most accurate for detecting pulmonary embolism.
General studies
These studies are focused on diagnosing the condition of the heart, lungs and blood. This may help with diagnosis or identify other conditions:
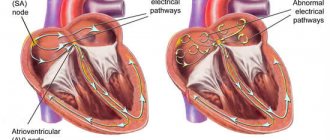
- An electrocardiogram (ECG) is performed on all patients. This is necessary to identify any signs of cardiac strain that may occur with PE. Any heart rhythm abnormalities, such as atrial fibrillation, that may result from thromboembolism are identified.
- Blood tests are used to look for signs of heart attack, infection, or inflammation. An arterial blood gas test may also be done, which involves taking a blood sample from an artery rather than a vein. This is necessary to check the oxygen level in the blood.
- A chest x-ray is used to detect pneumonia or other chest conditions.
- Treatment of pulmonary embolism
Establishment of clinical class and verification of diagnosis
Pulmonary function tests can identify obstructive or restrictive changes for the purpose of differential diagnosis of PH and clarify the severity of lung damage. Patients are characterized by a decrease in the diffusion capacity of the lungs for carbon monoxide (40-80% of normal), a slight or moderate decrease in lung volumes, a normal or slightly decreased PaO2, and usually a decreased PaCO2 due to alveolar hyperventilation.
Ventilation-perfusion lung scintigraphy is a screening method to exclude chronic thromboembolism as a cause of pulmonary hypertension. In patients after thromboembolism, perfusion defects are found in the lobar and segmental zones in the absence of ventilation disturbances. Perfusion scintigraphy has historically become one of the first methods for detecting perfusion defects in the pulmonary parenchyma in pulmonary embolism. The images obtained in acute PE and CTEPH differ significantly. Perfusion defects in acute PE are more clearly defined and contrast sharply with normally functioning tissue. In CTEPH, perfusion defects are not clearly defined and often do not correspond to the blood supply area of the large pulmonary artery.
Computed tomography and CT angiopulmonography
The CT picture of chronic thromboembolism can be represented by occlusions and stenoses of the pulmonary arteries, eccentric filling defects due to the presence of blood clots, including recanalized ones. CT angiopulmonography is performed on spiral computed tomographs during the phase of passage of the contrast agent through the pulmonary arterial bed. Among the methodological features, it should be noted that the study must be carried out using at least an 8-spiral tomograph, with a minimum step (no more than 3 mm) and a slice thickness (no more than 1 mm). A thorough scan should cover both lungs completely, from the apices to the phrenic sinuses. Contrast enhancement of the right chambers of the heart and pulmonary arteries should match or exceed the degree of contrast enhancement of the left chambers of the heart and aorta. The second, arterial phase of scanning is recommended for all patients over 40 years of age, especially if there is evidence of arterial thrombosis and coronary artery disease in the anamnesis. Modern software allows you to reconstruct images of the pulmonary arteries in any plane, construct maximum intensity projections and three-dimensional images. In most cases, to clarify the nature of the lesion, it is enough to analyze cross sections using an image viewer, which makes it possible to determine the presence of changes not only in the lobar and segmental branches, but also in a number of subsegmental arteries. Pathological changes, in addition to the presence of “old” thrombotic material, may include local thickening of the vessel wall, narrowing at the mouth of the vessels and along them, occlusions, intravascular structures in the form of membranes and bridges. If changes are detected in several branches of the pulmonary arteries, we can conclude that there is a high probability of thromboembolic nature of PH. It is important to note that the resolution of modern CT scanners is limited and does not allow the determination of very thin membranous and stringy structures in the lumen of the LA, especially if the size of the object does not exceed 2-3 mm. In some cases, calcification of the “old” thrombotic material develops, and CT can be invaluable in determining the location of the calcification. CT makes it possible to detect not only stenotic changes in the vessels of the lungs, but also disturbances in the perfusion of lung tissue by the nature of the contrast of the parenchyma. In some cases, parenchymal enhancement is so uneven that mosaic enhancement is detected on scans. A clearly defined mosaic pattern of segments usually indicates a good prognosis for surgical treatment. Contrasting exclusively in the root zones is not a true mosaic and is often observed in microvascular forms of PH. By providing detailed images of the lung parenchyma, CT allows the diagnosis of other lung diseases. In addition to the state of the arterial bed, CT can provide comprehensive information about all intrathoracic structures, which is important for confirming the diagnosis and developing a surgical treatment plan. Before performing the operation, the condition of the pulmonary parenchyma, bronchial tree, and pulmonary veins should be taken into account.
Angiographic diagnostics
The main objectives of angiographic diagnosis are to determine the severity of pulmonary hypertension, clarify the nature of the lesion in the pulmonary bed through angiopulmonography, and identify/exclude coronary disease. Carrying out catheterization in isolation without high-quality angiopulmonography in a patient with clear signs of CTEPH is inappropriate. This study should provide clear information to doctors to resolve the issue of the patient’s operability and the severity of his condition. Hemodynamic criteria for post-embolic pulmonary hypertension, identified during catheterization of the right heart, are: mean pulmonary artery pressure (PAP) above 25 mm Hg. Art., pulmonary artery wedge pressure (PAWP) ≤ 15 mm Hg. Art., PVR > 2 units. according to Wood (160 dyn. sec cm-5) in the presence of multiple stenotic and/or occlusive lesions of the branches of the pulmonary artery of various calibers.
Basic methods of treating pulmonary embolism
Anticoagulant therapy
Anticoagulant therapy is often referred to as blood thinning. However, it does not actually thin the blood. Anticoagulant therapy changes certain chemicals in the blood to prevent thrombotic clots from forming. This therapy does not dissolve the clot (as some people mistakenly think). Anticoagulation prevents the formation of new clots, and therefore thromboembolism. The body’s own mechanisms in the blood destroy the clot. Anticoagulant treatment is usually started immediately (if PE is suspected) to prevent worsening of the thrombosis while awaiting test results. Anticoagulation medications come in two forms: injections and tablets (or syrup for those who cannot swallow tablets). The first include heparin and fondaparinux. Tablet forms include warfarin and direct oral anticoagulants.
Supportive treatment is also used in the treatment of pulmonary embolism.
This therapy helps the body cope with the consequences of pulmonary embolism.
- Oxygen to reduce shortness of breath.
- In some cases, intravenous fluids are given to support circulation.
- If the patient is unwell or has a massive pulmonary embolism, careful monitoring and possibly intensive care are necessary.
- Additional procedures
They are usually used to treat severe or massive PE when the patient is very unwell or when treatment with anticoagulants is not possible.
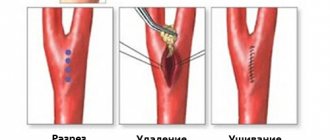
Thrombolysis is an injection of drugs that is used to dissolve a blood clot. The drugs commonly used are alteplase, streptokinase, or urokinase. They are more powerful than the anticoagulants heparin and warfarin described above. However, there is a greater risk of side effects such as unwanted bleeding. Unwanted bleeding may even include bleeding into the brain (intracerebral hemorrhage).
Kava filters . They can be used to prevent blood clots from reaching the lungs. The filter is placed in a large vein called the inferior vena cava. The filter is inserted through a thin tube, which is inserted into a large vein and then inserted along the vein into the correct position. This procedure does not require anesthesia and can be performed at the patient's bedside. Filters may be useful when anticoagulant treatment alone is not sufficient or for patients who for some reason cannot undergo anticoagulant treatment. Currently, the indications for the use of vena cava filters are narrowing.
Surgical embolectomy. In some cases, it is possible to remove the embolus surgically. This is called an embolectomy. This is a major operation because it involves surgery on the organs of the chest, near the heart. A specialized medical facility and a highly specialized surgical team are required. This is usually considered a last resort for seriously ill patients. The operation carries a significant risk of death. This intervention will only be considered as an option if there is a massive PE, limiting other treatment options.
Catheter thrombolysis .
This type of treatment is called catheter embolectomy or catheter clot fragmentation. It involves advancing a catheter through the blood vessels until it reaches the clot in the lung. Once the clot is reached, it can be removed or broken up (fragmented) with treatment given through the tube. This is a highly specialized treatment, so it is only available in certain treatment facilities.
Preparation for CT angiography of the pulmonary arteries
— Three hours before the procedure, you must stop eating or taking pills; only light drinking is allowed.
— The doctor must be provided with the necessary medical documentation and statements with the results of ultrasound, previous CT or MRI studies. This is necessary to ensure that CT angiography is performed with high quality.
— The patient should take care of preliminary blood donation in order to conduct a biochemical analysis that reveals the level of urea and creatinine. To do this, you can provide analysis results no more than two weeks old or take a rapid analysis.
— To get the most accurate result, the patient should remove metal objects and things from the chest area. We are talking about jewelry, clothes with metal fittings or thread, and mobile phones.
Complications of pulmonary embolism
Most people with PE are treated successfully and have no serious complications. However, serious complications are possible, including:
- Collapse - due to the effect of a blood clot on the heart and circulation. This can cause cardiac arrest and can be fatal. PE can cause heart strain. This can lead to a condition called heart failure, where the heart pumps less than normal.
- Recurrence of pulmonary embolism. Blood clots may occur again later (called recurrent PE). Treatment with anticoagulants helps prevent this.
- Bleeding. Complications due to treatment. Treatment with anticoagulants may have side effects. The main one is bleeding in various locations, for example, from a stomach ulcer. Approximately 3 in 100 patients will have significant bleeding due to treatment of PE with anticoagulants. This type of bleeding can usually be treated successfully. However, it is almost always safer to take anticoagulants to prevent recurrent PE, which can be even more severe.
- Chronic pulmonary hypertension. If small PEs recur, they may contribute to the development of a condition in which there is increased pressure in the blood vessels of the lungs (pulmonary hypertension).
Causes and pathogenesis
Pulmonary hypertension is divided into congenital and acquired. Otherwise, these forms are called primary and secondary. Among the causes of increased pressure in the pulmonary artery are the following:
- chronic lung diseases (bronchial asthma, COPD, sarcoidosis, interstitial pulmonary fibrosis, tuberculosis, silicosis, asbestosis)
- heart diseases (heart failure, acquired and congenital heart defects)
- stay in the highlands
- vasculitis
- effects of drugs on the body
- TELA
Pulmonary hypertension without a known cause is called primary hypertension. The cause of PH may be an increase in pressure in the pulmonary veins. Growth is provoked by the following factors:
- left ventricular failure
- mitral valve defects
- pulmonary vein compression
- left atrium myxomas
Increased pulmonary blood flow can also trigger pulmonary hypertension:
- patent ductus arteriosus
- ventricular septal defect
- atrial septal defect
Among the causes of the disease in question is an increase in pulmonary vascular resistance, which can be caused by:
- taking drugs that reduce appetite (fenfluramine) or chemotherapy drugs
- obstruction of the pulmonary artery and its branches
- inflammatory changes in the lung parenchyma
- destruction of the pulmonary vascular bed (with chronic destructive lung diseases, pulmonary emphysema)
- chronic alveolar hypoxia (for example, when staying high in the mountains)
Valvular defects lead to the occurrence of passive PH as a result of the transfer of pressure from the left atrium to the pulmonary veins and then to the pulmonary artery system. With mitral orifice stenosis, there can sometimes be a reflex spasm of the pulmonary arterioles due to increased pressure at the mouths of the pulmonary veins and in the left atrium. Long-term development of PH leads to irreversible sclerotic changes in arterioles and their obliteration.
If a person has congenital heart defects, PH results from increased blood flow in the pulmonary artery system and resistance to blood flow in the pulmonary vessels. Left ventricular failure, which occurs with dilated cardiomyopathy, coronary heart disease, and hypertension, can also cause pulmonary hypertension because the left atrium and pulmonary veins become higher than normal.
In chronic diseases of the respiratory organs, PH for a long period of time has a compensatory nature, because hypoxic pulmonary vasoconstriction turns off non-ventilated areas of the lungs from perfusion, which eliminates the shunting of blood in them, and hypoxemia decreases. At this stage, the use of a drug such as aminophylline reduces pressure in the pulmonary circulation, reduces compensatory vasostriction, and reduces intrapulmonary shunting of blood with deterioration of oxygenation. As lung disease progresses, PH becomes a factor in the pathogenesis of the formation of chronic “pulmonary heart.”
What are the prospects for pulmonary embolism?
This depends on the type of pulmonary embolism and the presence of concomitant diseases.
If PE is treated correctly and promptly, the prognosis is good and most patients can make a full recovery.
The prognosis is worse if there is a serious disease that contributed to the embolism, such as advanced cancer. Massive PE is more difficult to treat and is life-threatening. PE is a serious condition and can have a high risk of death, but this is greatly reduced with early treatment.
The most dangerous time for complications or death is the first few hours after an embolism. In addition, there is a high risk of developing a new pulmonary embolism within six weeks of the first one. Therefore, treatment must be started immediately and continued for at least six months.
Procedure for CT angiography of the pulmonary arteries
Before performing a CT angiography, a contrast agent with an iodine-containing dye is injected into the patient's elbow area. During the administration of the substance, the patient may experience a feeling of warmth spreading throughout the body, a salty or metallic taste in the mouth, and mild nausea. Such sensations are usually short-lived.
CT scan of the pulmonary arteries is performed on an outpatient basis. The patient and the doctor are in different rooms. While the patient is in a supine position on the CT scanner table, the radiologist operates the machine and instructs the patient from the next room. The doctor and patient see each other through the window located between the rooms. They talk through a speakerphone located in the tomograph itself. If necessary, the patient has the opportunity to call a doctor. The scanner is shaped like a ring and is open on both sides, so the patient has the opportunity to monitor what is happening. Due to the fact that image acquisition is a very precise process, to ensure maximum quality, the radiologist asks the patient from time to time to remain still and hold his breath for a few seconds. The duration of the entire procedure is about an hour.
After a CT scan, you should drink as much water as possible to prevent dehydration and speed up the removal of the contrast agent.
How to prevent pulmonary embolism?
To avoid pulmonary embolism, it is necessary to prevent and promptly treat chronic diseases. One of the causes of venous thrombosis is varicose veins. Any person who suspects he has this disease should visit a phlebologist and have the venous system of the lower extremities diagnosed. After diagnosis, you need to follow the doctor's recommendations. Also, patients planning major surgery should be assessed for the risk of deep vein thrombosis, and people at high risk of DVT may require prophylactic doses of anticoagulants before and after surgery.
Frequently asked patient questions about pulmonary embolism (PE)
What are the symptoms of pulmonary embolism?
The main symptoms to suspect pulmonary embolism are cough, shortness of breath, chest pain and hemoptysis.
How to avoid pulmonary embolism?
In order to prevent the development of pulmonary embolism, it is necessary to prevent venous thrombosis: promptly treat varicose veins and other vein pathologies, avoid prolonged immobilization for various diseases and surgical treatment, use anticoagulants in case of increased risks of thrombosis.
Who is more likely to develop pulmonary embolism?
Pulmonary embolism, as a rule, affects patients with severe cardiac and pulmonary pathology, cancer patients, and patients in various surgical hospitals after long-term surgical interventions.
What should you do if you suspect pulmonary embolism?
At the slightest suspicion of pulmonary embolism, you must call an ambulance. Before the arrival of medical personnel, the patient must be laid on a flat surface and ensure free access of air.
Statistics on morbidity and mortality of pulmonary embolism
Statistics show that about 0.1% of the world's population dies every year from pulmonary embolism. In terms of the frequency of deaths, this pathology is second only to coronary heart disease, strokes and some cancers.
The main cause of mortality in pulmonary embolism is late diagnosis. About 90% of patients do not receive the necessary treatment in the early stages of this acute condition.
The difficulty in diagnosing thromboembolism is that this condition can masquerade as a large number of heart and lung diseases. Many patients begin receiving therapy for heart attack or asthma. As a result, valuable time is lost.
Another danger of pulmonary embolism is suddenness. It affects not only patients with cardiovascular diseases, but also women during childbirth, and practically healthy people after injuries. Most often, after a diagnosis of pulmonary embolism is made, only 70% of patients can be saved. But if the pathology was diagnosed in a timely manner and optimal treatment was started, then this figure can increase to 98% percent.