When the strength, frequency and regularity of heart contractions are weakened, heart failure is diagnosed. Pathological changes in the activity of the heart provoke weakened blood flow in the human body and, as a result, oxygen starvation of tissues and organs, which causes characteristic symptoms.
Decompensated heart failure refers to the terminal stages of an abnormal process, which leads to irreversible cardiac pathological and functional disorders, which are dangerously fatal.
The pathological condition, which has become very widespread in the modern world, affects both women and men equally.
Overview of Heart Failure
A decrease in the contractile force of the heart muscle leads to a decrease in the volume of blood ejection and venous stagnation in the pulmonary and systemic circulation. The internal organs do not receive enough oxygen and nutrients, and due to increased venous pressure, edema develops. Stagnation of blood in the lungs leads to respiratory failure and oxygen starvation of tissues. A slowdown in blood flow in the vessels of the legs provokes the formation of blood clots, which can then break off and clog the arteries of the heart, lungs, and brain, causing death.
Classification of heart failure
According to the speed of development, acute and chronic heart failure
. The first appears and progresses quickly - within a few days or hours, the chronic one develops gradually.
Acute heart failure (AHF)
can develop according to the right or left ventricular type, depending on the location of myocardial damage.
The following stages are distinguished in the development of chronic heart failure (CHF):
- Symptoms of hemodynamic disturbances appear only during physical activity; nothing bothers the person at rest.
- Signs of venous stagnation: in one of the circulation circles; in large and small circles.
- Development of irreversible dystrophic changes in internal organs.
Causes of acute heart failure
The immediate causes of acute heart failure may be:
- complications of CHF (pulmonary embolism - blockage by a blood clot);
- myocarditis, pericarditis - inflammatory diseases of heart tissue;
- hypertension in the acute phase (hypertensive crisis);
- arrhythmia;
- myocardial infarction, coronary heart disease, major stroke.
Causes
The pathological condition is believed to be a consequence of certain cardiovascular diseases:
- excessive increase in blood pressure;
- heart valve defects;
- cardiac ischemia;
- cardiomyopathy;
- tachyarrhythmias, bradyarrhythmias;
- atherosclerotic changes;
- myocarditis;
- heart attacks.
At the moment, medicine does not have accurate data on the causes of the development of decompensated heart failure.
The disease can also be triggered by the following factors:
- endocrine diseases;
- anemia;
- infectious and inflammatory processes in the body;
- excessive physical activity;
- use of certain medications;
- bad habits (excessive consumption of alcohol, drugs, and smoking);
- extensive operations, burns;
- brain or heart injuries;
- nervous overload;
- unbalanced diet;
- pathological conditions of the liver and kidneys.
Pulmonary congestion accompanying decompensated heart failure leads to decompensated cardiopulmonary failure.
Causes of chronic heart failure
The development of CHF is caused by chronic lung diseases, congenital and acquired heart defects and other pathologies, including:
- stenosis and/or insufficiency of heart valves;
- hypertension;
- myocarditis, pericarditis;
- cardiac ischemia;
- hyperthyroidism is an excess of thyroid hormones in the blood.
At first, the compensatory capabilities of the heart allow one to maintain hemodynamics at the proper level, but over time they become depleted and signs of illness appear.
Stages of development of chronic pathologies
So, decompensation – what is it? A classification of diseases based on the stage of their progression will help answer the question. There are 3 degrees characterizing the development of pathology:
- Compensation stage - in this case, the body is able to independently compensate for the damage caused by the pathology. This form is characterized by the fact that the patient does not feel any special changes in his condition.
- Subcompensation stage - the body no longer copes with the pathology completely, and can only partially compensate for the damage caused to it. The patient notices a deterioration in his condition.
- The stage of decompensation is final; it occurs when the body has completely spent its strength and can no longer work to compensate for the damage caused by pathology. In this case, the patient is extremely weakened, feels unwell, in addition to the underlying disease, notes general weakness and impaired ability to work.
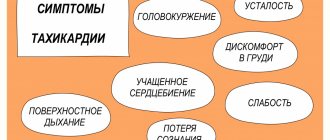
Symptoms of heart failure
The clinical picture of this pathology depends on what type of insufficiency develops and in what circle of blood circulation venous stagnation develops.
In right ventricular AHF
The volume of venous blood in the systemic circulation increases, resulting in the following symptoms:
- feeling of increased heartbeat;
- swelling of the limbs;
- swelling of the neck veins;
- a sharp drop in blood pressure, pallor, weakness, dizziness.
For left ventricular AHF
Blood stagnation occurs in the pulmonary circulation (pulmonary), so the following signs appear:
- chest pain;
- cough with pale pink frothy sputum;
- dyspnea;
- the appearance of foam in the corners of the mouth;
- disturbance of consciousness, confusion;
- the patient takes a forced sitting position, slightly leaning forward, in which the condition improves slightly.
A person with AHF needs urgent medical attention. If such symptoms appear, do not hesitate, you must call an ambulance.
Symptoms of chronic heart failure:
- shortness of breath, at first only during physical activity, later - at rest;
- cyanosis of the nasolabial triangle, fingertips;
- swelling of the legs, which appears in the evening and disappears in the morning;
- an increase in the volume of the abdomen due to the accumulation of fluid in it (ascites);
- signs of dysfunction of the liver, kidneys, central nervous system.
If such symptoms appear, it is recommended to consult a cardiologist or therapist.
Decompensation - what is it?
From Latin this word is translated as “lack of compensation” or “disequilibrium”. It is known that everything in our body is interconnected, therefore, when any disease occurs, compensatory mechanisms begin to operate. They are present in all organs and systems, and, if necessary, begin to use their reserves, for which there was no need previously. Decompensation - what is it? This state indicates that the body’s mechanisms have been exhausted, and it is no longer able to balance itself.
Diagnosis of heart failure
The examination program for a person with suspected heart failure includes:
- collection of complaints and symptoms;
- initial examination, listening to heart sounds and breathing sounds;
- ECG of the heart;
- Cardiac echocardiography (Echo-CG);
- X-ray of the chest organs;
- Ultrasound of the abdominal organs.
Diagnostic measures
Symptoms inherent in decompensated heart failure cannot serve as a basis for an accurate diagnosis. Only with the help of additional studies can the presence of pathology be established and appropriate treatment prescribed.
In addition, we should not forget about concomitant diseases, which also need to be identified and all measures taken to eliminate them.
Diagnosis of heart failure in the stage of decompensation occurs using the following methods.
1. Analysis of patient complaints.
2. Examination of the patient, which may reveal:
- pallor or bluish tint of the lips, nose and other areas located at a considerable distance from the heart;
- weakness and increased heart rate;
- deviation from normal blood pressure (the acute form is usually characterized by a decrease in blood pressure, although the opposite is not excluded).
It should be noted that wheezing and breathing sounds inherent in the acute course of the pathology prevent an accurate diagnosis.
3. Blood and urine tests.
Electrocardiography is a mandatory test if any cardiac dysfunction is suspected, and is also used as a mandatory preventive measure.
4. Electrocardiography, which allows to identify:
- cardiac scars;
- thickening of the heart muscle;
- abnormal heart rhythm;
- impaired cardiac conduction.
However, the presence of these abnormalities on the electrocardiogram is not an accurate criterion for diagnosing decompensated heart failure; they are also inherent in other diseases.
5. Ultrasound of the heart in combination with Doppler study is the most effective study and allows you to determine heart failure according to the following criteria:
- the volume of blood ejected by the ventricles is reduced by half;
- the ventricles have thickened walls (the anterior wall is 5 mm thicker than normal);
- an increase in the volume of the heart chambers;
- decreased ventricular contractility;
- expansion of the pulmonary aorta;
- disruption of the heart valve apparatus;
- the presence of congestion in the systemic circulation (the inferior vena cava, when filling the lungs with air (inhalation), decreases by less than half);
- increased pressure in the pulmonary artery.
6. X-ray examination, using which specialists determine the enlargement of the right chambers of the heart and increased pressure in the lungs:
- the pulmonary artery undergoes changes (its trunk bulges, its branches expand);
- pulmonary vessels lose their clear outline;
- the heart increases in size;
- areas of increased density are observed;
- Initially, the bronchi are affected by edema.
7. Determination in blood plasma of the amount of hormonal substances secreted by the heart muscle (natriuretic peptides).
In a normal state, their level is:
- NT-proBNP – 200 pg/ml;
- BNP –25 pg/ml.
These indicators play a significant role in determining the severity of heart failure.
Calling an ambulance in a timely manner in case of acute heart failure can save a person’s life
Diagnosis and treatment of heart failure in Medical
Our doctors select an individual examination and treatment regimen based on the characteristics of each patient.
All diagnostics and treatment are carried out using expert-class equipment certified in Russia and approved for use by the Ministry of Health of the Russian Federation.
When should you see a doctor?
The reason for visiting a cardiologist should be alarming symptoms from the cardiovascular system: pain in the heart, dizziness, pressure surges, swelling, palpitations, etc. You should not delay your visit to the doctor, because in the early stages it is much easier to treat and control the disease.
Drug therapy for heart failure
Treatment of heart failure is carried out by prescribing drugs that facilitate the work of the heart, improve the rheological properties of the blood and hemodynamics. Such drugs include:
- B-adrenergic receptor blockers;
- cardiac glycosides;
- angiotensin receptor blockers;
- diuretics;
- nitrates.
Dosages and combinations of drugs are selected by the doctor; during the treatment process, it is often necessary to adjust the prescriptions taking into account the person’s condition.
It is unacceptable to prescribe medications to yourself after reading about the symptoms and treatment of diseases on the Internet or on the advice of a pharmacist at a pharmacy. Do not deprive yourself of the opportunities of modern world cardiology - contact a cardiologist for medical help at the Paracelsus Clinic.
Acute form of the disease
The body’s inability to cope with rapid decompensation in acute forms of heart failure gives the right to classify this pathology as decompensated in almost every case.
The causes of the critical condition have not yet been determined, but experts believe that it occurs when the rules of treatment and diet for a concomitant disease are not followed.
The occurrence of left-sided acute failure is directly related to the following conditions:
- myocardial infarction;
- mitral valve stenosis;
- severe hypertensive crisis;
- congenital or acquired heart valve defects;
- malignant metastatic tumor processes;
- sepsis, etc.
Overflow of the pulmonary vessels with blood, resulting from the inability of the heart to pump blood, provokes the occurrence of pulmonary failure and pulmonary edema.
Right-sided localization of the pathological process is observed as a result of:
- pulmonary embolism;
- massive myocardial infarction with internal rupture (interventricular septum rupture);
- unilateral or bilateral pneumonia;
- pleurisy or pericarditis.
The systemic circulation is subject to stagnation, which leads to accumulation of blood in the lungs and liver. These processes are fraught with the occurrence of liver failure, edema or pulmonary infarction, which cannot exclude death.
In most cases, right ventricular failure occurs due to acute pathological changes in the lung tissue.
A patient exposed to an acute form of the disease requires medical attention, which should follow immediately if the following manifestations occur:
- increasing shortness of breath (difficulty in breathing is especially pronounced if the patient wants to take a lying position);
- noisy breathing;
- cough, which can have a different character (dry, containing putrid or red sputum, pink foam, accompanied by pain in the heart, etc.);
- cyanosis on the lips, tip of the nose;
- feelings of anxiety, unreasonable fear.
With these symptoms, the patient requires hospital treatment, but to prevent death, he must be provided with immediate pre-medical care.