Characteristics of normal heart sounds.
The first sound occurs during systole after a long pause.
It is best heard at the apex of the heart, since the systolic tension of the left ventricle is greater than that of the right. By nature, the first tone is longer and lower than the second.
The second tone is formed during diastole after a short pause. It is best heard at the base of the heart, as it occurs when the semilunar leaflets of the aortic valves and pulmonary trunk close. Unlike the first tone, it is shorter and higher pitched.
In pathology, when the sonority of tones can change, it helps to distinguish the first and second tones by the fact that the first tone coincides with the apical impulse (if the latter is palpated) and with the pulse of the aorta and carotid artery.
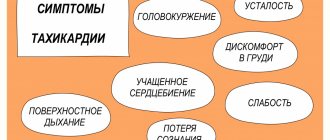
Changes in heart sounds can be expressed as:
v weakening or enhancing the sonority of one or both tones,
v in changing their timbre, duration,
v in the appearance of bifurcation or splitting of fundamental tones,
v the appearance of additional tones.
Heart sounds are amplified when large air cavities are located near it (large pulmonary cavity, large gas bubble of the stomach) - due to resonance. The sonority of the tones also depends on the composition of the blood flowing through the heart: when the viscosity of the blood decreases, as is observed with anemia, the sonority of the tones increases.
Fig. 8. Valve projection locations
on the anterior chest wall
In the diagnosis of heart diseases
It is of great importance to identify changes in tones caused by damage to the heart itself, i.e. caused by cardiac causes.
A weakening of both tones can be observed with a decrease in the contractility of the heart muscle in patients with myocarditis, myocardial dystrophy, cardiosclerosis, with collapse, or accumulation of fluid in the pericardial cavity.
An increase in both tones occurs due to an increase in the influence of the sympathetic nervous system on the heart. This is observed during heavy physical work, anxiety, and in people suffering from Graves' disease.
More often than a change in both heart sounds, there is a change in one of them, which is especially important in the diagnosis of heart disease.
Weakening of the first sound at the apex of the heart is observed:
· Insufficiency of the mitral and aortic valves.
With mitral valve insufficiency during systole, the valve leaflets do not completely cover the left atrioventricular orifice.
Strengthening of the first sound at the apex of the heart is observed:
· with narrowing of the mitral orifice.
Weakening of the first tone at the base of the xiphoid process of the sternum
· with insufficiency of the tricuspid valve and the pulmonary valve.
Strengthening of the first tone at the base of the xiphoid process of the sternum is heard:
· with stenosis of the right atrioventricular orifice.
An increase in the first tone is also observed with extrasystole - premature contraction of the heart - due to low diastolic filling of the ventricles.
Normally, the strength of the second tone over the aorta and pulmonary trunk is the same.
Weakening of the second tone over the aorta is observed:
· in case of aortic valve insufficiency, or due to their cicatricial compaction;
· with large destruction of the aortic valve leaflets, the second sound above it may not be heard at all;
· with a significant decrease in blood pressure;
Weakening of the second tone above the pulmonary trunk is observed:
· in case of insufficiency of its valve (which is extremely rare);
· with a decrease in pressure in the pulmonary circulation.
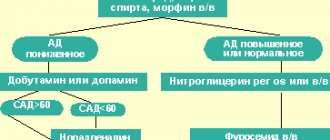
Strengthening of the second tone can be observed either above the aorta or above the pulmonary trunk.
In cases where the second tone is more sonorous above the aorta, they speak of the accent of the second tone on the aorta, but if it is more sonorous above the pulmonary trunk, they speak of the accent of the second tone on the pulmonary artery.
The emphasis of the second tone on the aorta is observed:
· when the pressure in it increases (hypertension, nephritis, heavy physical work, mental agitation), since at the beginning of diastole the blood hits the valve flaps with greater force.
The emphasis of the second tone on the pulmonary artery appears:
· with increased pressure in the pulmonary circulation, blood overflow of the pulmonary vessels (for example, with mitral heart defects),
· obstruction of blood circulation in the lungs and narrowing of the pulmonary artery bed (with emphysema, pneumosclerosis, etc.)
Heart murmurs.
When auscultating the heart, in some cases, in addition to tones, sound phenomena called heart murmurs are heard.
Murmurs can occur: inside the heart itself - intracardial, outside of it, extracardiac.
Organic murmurs occur due to anatomical changes in the structure of the heart valves.
Functional noises appear:
in case of dysfunction of unchanged valves
· with an increase in blood flow speed or a decrease in blood viscosity.
The most common cause of intracardial murmur is heart defects.
Based on the time the noise appears during systole or diastole, systolic and diastolic murmurs are distinguished.
Systolic murmur appears:
· when, during systole, blood, moving from one part of the heart to another or from the heart to large vessels, encounters a narrowing on its way.
· with stenosis of the aortic mouth or pulmonary trunk, since with these defects, during the expulsion of blood from the ventricles, an obstacle arises in the path of blood flow - narrowing of the vessel.
· listened to insufficiency of the mitral and tricuspid valves.
Its occurrence is explained by the fact that during ventricular systole, blood flows not only into the aorta and pulmonary trunk, but also back into the atrium through an incompletely covered mitral or tricuspid opening. Since this not completely covered hole is a narrow gap, noise occurs when blood passes through it.
Diastolic murmur appears in cases where there is a narrowing in the path of blood flow in the diastole phase:
· with narrowing of the left or right atrioventricular orifice, since with these defects during diastole there is a narrowing in the path of blood flow from the atria to the ventricles.
· in case of insufficiency of the aortic valve, pulmonary trunk - due to reverse blood flow from the vessels into the ventricles through the gap formed when the leaflets of the altered valve are not completely closed.
During auscultation it is necessary to determine:
1) the ratio of noise to the phase of cardiac activity (to systole or diastole);
2) properties of noise, its nature, strength, duration;
3) noise localization, i.e. best place to listen;
4) direction of noise conduction.
The ratio of noise to systole or diastole is determined by the same criteria by which we distinguish between the first and second sounds.
Date added: 2015-03-03; ; ORDER A WORK WRITING
The II tone consists of 2 components: valvular and vascular. Their formation occurs at the very beginning of ventricular diastole. The pressure in them drops sharply, while in the aorta and pulmonary artery it remains high. A pressure gradient occurs again, but this time between the vessels (aorta and pulmonary artery) and the ventricles. Blood under pressure rushes from the vessels into the ventricles and, entering the crescents of the valves, closes them - the valve component of the second tone appears. At the same time, oscillation of the initial parts of the aorta and pulmonary trunk occurs as a result of the ejection of blood from the leaflets of closed valves - this is how the vascular component of the second tone is formed.
Both tones are heard over the entire region of the heart, but the first tone is better heard (it is louder) than the second tone at the apex of the heart and the base of the xiphoid process, i.e., where it arises. Therefore, the assessment of the first tone is made at the apex of the heart, because systolic tension of the left ventricle is greater than the right. The second sound occurs on the semilunar valves, so it is better heard at the base of the heart (in the second intercostal space to the right and left of the sternum). This is where it is assessed. Note that normally the second sound over the aorta and pulmonary artery should be equal in strength.
Distinctive features of I and II tones
1. The first sound is better heard at the apex of the heart and the base of the xiphoid process. There it is louder than tone II. The second tone is better heard at the base of the heart.
2. I tone is longer than II.
3. The first sound occurs after a long pause (after diastole), and the second sound occurs after a short pause (after systole).
4. Tone I is lower in timbre (frequency), and tone II is higher.
5. The first tone coincides with the apical impulse and pulsation of the carotid arteries, the second sound does not coincide.
Sometimes a third tone can be heard in children and young people. In adults it is not normally heard, but it is often recorded on a phonocardiogram (graphic recording of heart sounds). The third sound occurs in diastole, in the phase of rapid passive filling of the ventricles with blood, 0.12-0.18 seconds after the second sound, because The first portions of blood, flowing from the atria into the ventricles, cause vibrations of the walls of the ventricles. Normally, the third tone is very quiet, of low timbre, better heard directly by the ear and perceived as a push.
It is rarely possible to listen to the IV tone. It occurs at the end of ventricular diastole 0.05-0.06 seconds before the first sound and is caused by atrial systole, when the remaining amount of blood in them quickly enters the ventricles, causing vibrations of their walls. Normally, the IV tone is not heard in adults.
Many clinicians explain the occurrence of physiological III and IV tones by high elastic properties and good tone of the heart muscle in children, adolescents and young adults, in whom they most often occur. Unlike pathological III and IV tones, which form the so-called “gallop rhythm,” physiological III and IV tones are heard against the background of normal I and II tones.
Changes in sonority of tones
The sonority (loudness) of tones is influenced by extracardiac and cardiac causes. There are intensification and weakening of tones.
Extracardiac causes affecting the sonority of heart sounds
1. Weakening of both tones occurs with thickening of the chest wall, obesity, pronounced development of the muscles of the shoulder girdle, edema of the chest wall, accumulation of fluid in the left pleural cavity, and pulmonary emphysema. In these cases, the heart “moves away” from the chest wall.
2. Strengthening of both tones occurs when the heart approaches the anterior chest wall. This happens with weight loss, in asthenic patients, with wrinkling of the edges of the lungs, tumors of the posterior mediastinum. In addition, the sounds intensify when air-containing cavities appear in the lungs near the heart (lung abscess, tuberculosis cavity), a decrease in blood viscosity, and tachycardia.
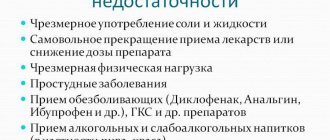
Intracardiac causes affecting the sonority of heart sounds
1. Weakening of both tones occurs when the heart muscle is damaged: with inflammation (myocarditis), myocardial infarction, myocardial dystrophy, cardiosclerosis, fluid accumulation in the pericardial cavity.
2. Strengthening of both tones occurs when the tone of the sympathetic nervous system increases, during physical activity, emotional stress, and thyrotoxicosis.
A change in the sonority of only one of the heart sounds is of greater diagnostic significance.
Factors influencing the sonority of the first tone.
1. The state of the main components that form the first sound - valvular, muscular, and to a lesser extent - vascular. Speaking about the valve component, we must first of all keep in mind the insufficiency of the atrioventricular valves. However, insufficiency of any of the four valves will also lead to a weakening of the first tone, since there will be no “period of closed valves.” Any pathological conditions affecting the heart muscle (myocarditis, heart attack, cardiosclerosis, myocardial dystrophy, etc.) will also lead to a weakening of the first tone.
2. The degree of blood filling of the ventricles of the heart. The greater the blood supply, which is often observed with heart defects, the longer the duration of ventricular systole and the duller the first sound is perceived. On the contrary, a decrease in the blood filling of the ventricles leads to a shortening of systole, it becomes energetic, fast, and the first sound is perceived loud, sometimes flapping.
3. The amplitude of movement of the atrioventricular valve leaflets: the larger it is, the louder the first sound (for example, a systolic click with mitral valve prolapse); as the amplitude decreases, the first sound weakens.
4. State of myocardial muscle mass. The systole of the hypertrophied myocardium lengthens, the first sound becomes muffled. This is also facilitated by dystrophic changes that develop over time in the hypertrophied heart muscle due to inadequacy of coronary circulation.
5. Extracardiac causes (degree of development of muscles, fatty tissue in the chest area, etc.).
Based on these patterns, the main reasons for the weakening of the first tone are:
1. extracardiac: pulmonary emphysema, thickening of the chest;
2. cardiac: damage to the heart muscle (myocarditis, cardiosclerosis, myocardial infarction, cardiomyopathy, etc.); insufficiency of any heart valve (due to the “absence of a period of closed valves” in combination with an increase in blood supply to the ventricles); stenosis of the aortic orifice and pulmonary artery (overflow of blood from the left and right ventricles and prolongation of their systole); ventricular hypertrophy of any origin (increase in muscle mass and prolongation of ventricular systole).
Strengthening the first tone
1. extracardiac reasons: asthenic chest, decreased airiness of the lung tissue, the presence of a cavity in the lung near the heart.
Question 4. Reasons for weakening and strengthening (emphasis) of tone II.
A weakening of
the second tone
is recognized in the presence of a symptom such as a decrease in the sound of the second tone in comparison with the first tone or when the degree of sonority of both tones is the same at the base of the heart (the place of auscultation of the aorta and pulmonary artery).
Weakening of the second sound over the aorta is very characteristic of heart disease - aortic valve insufficiency. The cause of aortic regurgitation syndrome is the complete or partial destruction of the valve leaflets, their scarring and reduction in area. In the absence of the obturator function of the valve, blood flows back through the gap (regurgitates) from the aorta into the left ventricle. A decrease in the area of the valve leaflets and the absence of a push of blood onto the leaflets leads to a decrease in the sonority of the second sound in the aorta. If the valves are completely destroyed, the second sound in the aorta may not be heard at all.
Weakening of the second tone in the pulmonary artery occurs with rather rare valvular heart defects: pulmonary valve insufficiency and narrowing of its mouth. The mechanism for weakening the tone in these cases is the same conditions as for similar aortic defects.
Strengthening, accent
of tone
II . Normally, in adults, when listening and comparing the second tone on the aorta and on the pulmonary artery, it is noted that their volume is the same. This is explained by the fact that the pulmonary valve is located closer to the chest than the aortic valve, due to which the transmission of sound phenomena from them is equalized, although the greater blood pressure in the aorta also gives a greater push force on the aortic valve leaflets when they close.
The mechanism of occurrence of tone II and its changes.
The period of blood expulsion from the ventricles of the heart consists of two phases - fast and slow blood expulsion. At the end of the slow ejection phase, the ventricular myocardium begins to relax and diastole begins. Blood pressure in the ventricles of the heart decreases, and blood from the aorta and pulmonary artery rushes back into the ventricles of the heart. It closes the semilunar valves and a second or diastolic heart sound occurs. The first tone is separated from the second tone by a short pause with an average duration of about 0.2 seconds. The second tone has two components, or two components. The main one in terms of volume is the valve
a component formed by vibrations of the leaflets of the semilunar valves.
After the slamming of the semilunar valves, blood rushes into the arteries of the systemic and pulmonary circulation. The pressure in the aorta and pulmonary trunk gradually decreases. All pressure changes and blood movement in the aorta and pulmonary artery are accompanied by vibrations of their walls, forming the second, less loud, component of the 2nd tone - the vascular
component.
The time from the beginning of ventricular relaxation to the closure of the semilunar valves is called the protodiastolic period.
equal to 0.04 seconds.
The blood pressure in the ventricles at this time drops to zero. The leaflet valves are still closed at this time, the volume of blood remaining in the ventricles and the length of the myocardial fibers have not yet changed. This period is called the isometric relaxation period
, equal to 0.08 seconds.
Towards its end, the cavities of the ventricles of the heart begin to expand, the pressure in them becomes negative, lower than in the atria. The leaflet valves open and blood begins to flow from the atria into the ventricles of the heart. The period of filling the ventricles with blood
begins , lasting 0.25 seconds. This period is divided into 2 phases of fast (0.08 seconds) and slow (0.17 seconds) filling of the ventricles with blood.
Second heart sound
best heard at the base of the heart. Since the second sound is predominantly valvular, it has 2 points of best auscultation - at the point of auscultation of the pulmonary artery valves and at the point of auscultation of the aortic valves.
The sound phenomena of the pulmonary artery valve, forming the 2nd heart sound, are best heard above the place of the chest wall that is located closest to the mouth of the pulmonary artery, namely in the second intercostal space to the left of the sternum. Here, the initial part of the pulmonary artery is separated from the chest wall only by a thin edge of the lung.
The aortic valves are located deeper than them, located slightly inward and below the pulmonary artery valves, and are also covered by the sternum. The tone produced when the aortic valves close is transmitted along the blood column and the walls of the aorta. In the 2nd intercostal space, the aorta comes closest to the chest wall. To evaluate the aortic component of the 2nd tone, a phonendoscope should be placed in the second intercostal space to the right of the sternum.
A weakening of the second tone is recognized in the presence of a symptom such as a decrease in the sound of the second tone in comparison with the first tone or when the degree of sonority of both tones is the same at the base of the heart (the place of auscultation of the aorta and pulmonary artery).
Weakening of the second sound over the aorta is very characteristic of heart disease - aortic valve insufficiency. The cause of aortic regurgitation syndrome is the complete or partial destruction of the valve leaflets, their scarring and reduction in area. In the absence of the obturator function of the valve, blood flows back through the gap (regurgitates) from the aorta into the left ventricle. A decrease in the area of the valve leaflets and the absence of a push of blood onto the leaflets leads to a decrease in the sonority of the second sound in the aorta. If the valves are completely destroyed, the second sound in the aorta may not be heard at all.
Weakening of the second tone in the pulmonary artery occurs with rather rare valvular heart defects: pulmonary valve insufficiency and narrowing of its mouth. The mechanism for weakening the tone in these cases is the same conditions as for similar aortic defects.
Strengthening, accent of tone II . Normally, in adults, when listening and comparing the second tone on the aorta and on the pulmonary artery, it is noted that their volume is the same. This is explained by the fact that the pulmonary valve is located closer to the chest than the aortic valve, due to which the transmission of sound phenomena from them is equalized, although the greater blood pressure in the aorta also gives a greater push force on the aortic valve leaflets when they close.
In children and young people, the second tone on the pulmonary artery is often stronger than on the aorta - the emphasis of the second tone on the pulmonary artery. This is explained by the fact that the pressure in the aorta in children is lower than in adults, and the pulmonary artery is located closer to the anterior wall of the chest (the place of auscultation).
Under some pathological conditions, the volume of the second tone in the aorta and pulmonary artery becomes unequal. In cases where the II tone on the aorta significantly prevails over the I, and, in addition, becomes louder than the II tone of the pulmonary artery, they speak of the intensification and emphasis of the II tone on the aorta.
Since the volume of the second tone depends on the strength of the push of blood against the valves of the aorta or pulmonary artery at the beginning of diastole, it increases in parallel with the increase in blood pressure in the vessels.
The emphasis of the second tone on the aorta is observed in arterial hypertension, in hypertension. The emphasis of the second tone on the pulmonary artery is observed with hypertension in the pulmonary artery and high pressure in the pulmonary circulation, for example, with mitral heart defects, when there is stagnation of blood in the pulmonary circulation. An audible accent of the second tone on the aorta in patients without arterial hypertension may indicate atherosclerosis of the aorta, when the dilated aorta and its thickened wall better conduct sounds to the point of auscultation. In the latter case, the sound of tone II may acquire a metallic tint.
Question 5. Splitting, splitting of heart sounds.
Double tone is a condition when, during auscultation of the heart, instead of one continuous sound, two sounds are heard following each other after a short period of time. If the time interval between these two sounds is very small and there is no complete impression of the separateness of the sounds, then they talk about splitting the tone. This condition can occur in both I and II.
Splitting (incomplete separation) and bifurcation (complete separation) of both I and II tones can be physiological, i.e. found in completely healthy people, and pathological, observed in some heart diseases. Physiological separation of tones is more common in young people and is usually associated with the act of breathing, and therefore is not constant.
Splitting and bifurcation of the first tone is caused by non-simultaneous closure of the mitral and tricuspid valves. In healthy people, this phenomenon can sometimes appear during exhalation, when, due to increased pressure in the chest, more blood flows into the left parts of the heart than into the right, which causes asynchronous closure with faster closure of the mitral valve. Therefore, the sound phenomena of the valve component of the AV valves on exhalation are perceived separately, and on inspiration, the first sound is heard as one sound.
Splitting or bifurcation of the first tone in pathological conditions is especially characteristic of blockade of one of the branches of the His bundle, when excitation to one of the ventricles arrives late, which means that the mechanical process of contraction of the ventricles occurs later. The atrioventricular valve of the “blocked” ventricle is delayed in closing. This separation of the first tone does not depend on the phases of breathing - it is constant.
The separation of the second tone is heard more often on the pulmonary artery. It is explained by the non-simultaneous closure of the aortic and pulmonary valves. Under physiological conditions, this phenomenon occurs and is more pronounced during inspiration, when, with a decrease in intrathoracic pressure, the suction effect of the chest causes a slightly larger volume of blood to pass through the right than the left parts of the heart. In such a situation, systolic emptying of the right ventricle requires more time than the left. Therefore, the pulmonary component of the second tone is significantly behind the aortic one. This is the mechanism of splitting and bifurcation of the second tone, which is heard during inspiration, especially with deep breathing.
In patients with increased blood pressure in the pulmonary circulation (mitral heart defects, pulmonary hypertension, thromboembolism of the branches of the pulmonary artery), the duration of systole of the right ventricle, in comparison with the left, also increases, which causes a significant lag of the pulmonary component of the second sound from the aortic component. This is the most common mechanism of splitting and bifurcation of the second tone.
In patients with bundle branch block, especially the right bundle branch, splitting of the second sound is also possible due to asynchrony of the end of systole of the right and left ventricles. With right bundle branch block, the onset of right ventricular diastole, manifested by the pulmonary component of the second sound, occurs significantly later than the onset of left ventricular diastole. Moreover, with such a pathology, both heart sounds may be split.
“Tripartite rhythms” associated with the appearance of additional diastolic or systolic sounds should be distinguished from bifurcation of heart sounds.
Reasons and mechanism for the formation of accent of the II tone, splitting of the II tone
P tone accent. It is assessed by comparing the volume of the second tone in the second intercostal space at the edge of the sternum, respectively, on the right or left. The emphasis is noted where the tone is louder, and may be on the aorta or pulmonary trunk. Acceptance of tone II can be physiological and pathological. The physiological emphasis is age-related. It is heard on the pulmonary trunk in children and adolescents. It is usually explained by the closer location of the pulmonary trunk to the site of auscultation. The emphasis on the aorta appears by the age of 25-30 and somewhat intensifies with age due to the gradual thickening of the aortic wall. We can talk about a pathological accent in two situations:
1) when the accent does not correspond to the proper point of auscultation corresponding to age (for example, loud volume II on the aorta in a young man) and
2) when the volume of the second tone is greater at a point, although corresponding to the age, but it is too high in comparison with a healthy person of this age and physique, or the second tone has a special character (ringing, metallic)
The reason for the pathological acceptance of the second tone in the aorta is an increase in blood pressure and (or) compaction of the valve leaflets and the aortic wall. The emphasis of the second tone on the pulmonary trunk is usually observed in pulmonary arterial hypotension (mitral stenosis, cor pulmonale, left ventricular failure)
Physiological splitting of the second tone is heard exclusively at the base of the heart during inhalation and exhalation or during physical activity. At the end of a deep inhalation, when the chest expands due to a decrease in pressure in it, the blood is somewhat retained in the dilated vessels of the small circle and therefore flows in smaller quantities into the left atrium, and from there into the left ventricle. The latter, due to less blood filling, ends systole earlier than the right one, and the closure of the aortic valve precedes the closure of the pulmonary valve. During exhalation, the opposite conditions are created. In the case of increased pressure in the chest, blood, as if squeezed out of the vessels of the pulmonary circle, enters in large quantities into the left part of the heart, and the systole of the left ventricle, and therefore the beginning of its diastole, occurs later than the right.
At the same time, a split second tone may be a sign of serious pathological changes in the heart and its valves. Thus, a bifurcation of the second sound at the base of the heart (second intercostal space on the left) is heard with mitral stenosis. This is due to the fact that the hypertrophied and blood-filled right ventricle ends systole later than the left. Therefore, the aortic component of the second sound occurs earlier than the pulmonary one. Bifurcation or splitting of the second sound in bicuspid valve insufficiency is associated with greater blood filling of the left ventricle than normal, which leads to prolongation of its systole, and the diastole of the left ventricle begins later than the right. Because of this, the aortic valve closes later than the pulmonary valve.
Emphasis and weakening of the second tone on the pulmonary artery or aorta.
The second tone is heard at the base of the heart, where normally it is louder than the first tone and is equal in strength in the second intercostal space on the right and left. Weakening - if the second tone is equal in volume to the first or quieter. Occurs with low pressure in large vessels, a decrease in their blood supply, with damage to the aortic and pulmonary valves, which leads to a violation of their slamming. Above the aorta - with the deposition of calcium salts, which leads to a decrease valve mobility. Above the pulmonary artery - with a large thickness of the chest. Strengthening - The emphasis of the second tone on the aorta may occur due to its intensification at this point, or weakening in the pulmonary artery. Increased blood pressure in the systemic circle with mitral disease and cor pulmonale, thickening of the aortic walls (atherosclerosis), pulmonary valve insufficiency, decreased pressure in the pulmonary artery (pulmonary artery stenosis). The emphasis of the second tone on the pulmonary artery may be due to its intensification in the pulmonary artery or weakening in the aorta. Increased blood pressure in the pulmonary artery, thickening of the pulmonary artery wall, aortic valve insufficiency, decreased pressure in the pulmonary artery. In childhood and adolescence, the second tone on the pulmonary artery is louder than on the aorta. In adulthood, their volume is the same; in the elderly, the second tone is louder on the aorta due to its compaction during atherosclerosis.
24.III and IV heart sounds.Ri.
The third tone comes after the second in 0-15 seconds. It is low, dull, heard at the apex in the position of the patient lying on the left side. Normally it occurs in children under 6 years old, in asthenic adults up to 35-40 years old, in pregnant women in the third trimester ( due to imperfect regulation of myocardial tone). Caused by fluctuations of the myocardium of the left ventricle during its rapid passive filling with blood at the beginning of diastole. In pathology, in persons over 40 years of age with a decrease in the contractile activity of the myocardium (chronic heart failure), with overload of the ventricles with blood volume (insufficiency mitral or tricuspid valve). The fourth sound comes before the first sound at the beginning of diastole. It is low, dull, and is associated with rapid filling of the left ventricle due to contractions of the left atrium. Normally, in the elderly there are no changes in the heart, in trained people. In pathology, hypertension, aortic stenosis, cardiomyopathy. The gallop rhythm occurs before the first tone, or after the second, is associated with the appearance of the third or fourth tone, reminiscent of the clatter of the hooves of a galloping horse. It is caused by a decrease in the tone of the heart muscle, changes in the properties of the myocardium, and a decrease in its contractility (with dilatation of the left ventricle, heart failure). Three-member rhythm with an additional III sound it forms a proto-diastolic gallop rhythm, and with a IY tone it forms a presystolic rhythm. It is found at the apex of the heart or in the 3-4th intercostal space on the left at the sternum, heard against the background of tachycardia and weakening of the I tone.
Split heart sounds. Mitral valve opening tone.
Bifurcation of the second tone is associated with the non-simultaneous closure of the valves of the aorta and pulmonary artery due to different durations of contractions of the left and right ventricles, respectively, changes in the large and small circle. With increased pressure, increased blood filling in the small or large circle. Normally, there may be a slight bifurcation ( at the base of the heart - in the 2nd intercostal space) - in young people with deep inspiration (due to increased blood flow to the right heart, the systole of the right ventricle is prolonged, above the pulmonary artery - splitting. Its second component is associated with the slamming of the aortic valve. In pathology - with dilatation of the right ventricle against the background of pulmonary artery stenosis, in case of disruption of the conduction of excitation along the right leg of the atrioventricular bundle of His (later closure of the pulmonary valve). With an atrial septal defect, an increase in the volume of the cut in the right atrium, then in the right ventricle, which leads to overload blood of the pulmonary circle (the splitting is strong, above the pulmonary artery does not depend on the phases of breathing). For pulmonary hypertension in patients with chronic lung diseases (the splitting is less pronounced and distinct, because the right ventricle is hypertrophied and its systole is not prolonged. Bifurcation of the first tone is normal along the left edge of the sternum (a tricuspid component is heard), sometimes at the apex along with the fourth sound and an early systolic click. In pathology, when intraventricular conduction along the branches of the His bundle is impaired, which leads to a delay in the systole of one of the ventricles.
The opening tone of the mitral valve comes after the second tone, at the apex of the heart (medially and along the left edge of the lower third of the sternum) with the patient in the position on the left side. It is high and clicking. In patients with mitral stenosis (with sclerosis and fusion of the leaflets), their opening at the beginning of diastole is limited, so the blood flow causes these valves to oscillate (they bend towards the left ventricle under the influence of high pressure in the left atrium).
Heart murmurs. Classification.
Types: 1. Intracardiac: A-organic (valve, muscle) B-functional
(high-speed - due to an increase in blood flow speed during thyrotoxicosis and fever, anemic - due to a decrease in blood viscosity, dystonic - due to changes in the tone of the papillary muscles). 2. Extracardial: A-pericardial B-pleurocardial.
1. Intracardial - occur due to organic changes in the valves or heart muscle. Organic changes in the heart valves lead to stenosis of the orifice or valve insufficiency. With stenosis, the valve leaflets fusion (reduction of the orifice), which makes it difficult for blood to pass into the ventricle of the heart or aorta. With insufficiency, wrinkled and the shortened valves do not completely close the hole and blood rushes past the damaged valves in the opposite direction (regurgitation). Due to the narrowing of the hole, the laminar movement of blood becomes turbulent, creating noise. The intensity of the noise is greater, the greater the degree of narrowing and the speed of blood movement.
A-Organic occurs when the volume of blood does not correspond to the size of the hole through which it flows, against the background of other signs of cardiovascular pathology. They can be systolic and diastolic. They are louder and rougher than functional ones, more durable, carried out to other areas, do not disappear when changing position body, deep breathing, intensifies with physical activity. Muscular occurs when the papillary muscles are damaged. Valvular - with myocarditis, myocardial dystrophy, cardiomyopathy, cardiosclerosis - when dilation of the heart cavities and expansion of the valve ring occurs, which leads to incomplete closure of the valve leaflets. B-Functional are determined in the absence of signs of damage to the heart valves and myocardium. They are systolic, heard at the apex of the heart or on the pulmonary artery - gentle, blowing, quiet, short, not conducted outside the heart area. May disappear with changes in body position, physical activity, deep breathing.
2. Extracardial (extracardiac) - occur in connection with contractions of the heart or damage to neighboring organs. A-Pericardial - rough, scraping, scratching, occurs in the presence of inflammation of the pericardial layers with fibrin deposition (dry pericarditis). It is better heard in the zone of absolute dullness and at the base of the heart, is not carried out to other areas, intensifies when the body is tilted forward, pressing with a stethoscope ,sometimes determined by palpation. B-Pleurocardial - occurs with dry pleurisy in the area of contact of the pleura to the heart. Contraction of the heart increases the contact of the pericardium and pleura, which contributes to the appearance of friction noise. It is distinguished from pericardial friction noise by intensification during inspiration and localization along the left contour of the heart.
When listening to a murmur, it is necessary to determine its relationship to the phases of the cardiac cycle (systole or diastole), its properties (strength, duration, timbre), the place of best listening, the direction of its conduction (outside the heart area).
Murmurs that appear during systole (between the I and II sounds) are systolic, between the II and I sounds are diastolic. Systolic is heard with narrowing of the aortic mouth and the mouth of the pulmonary artery, with insufficiency of the bicuspid and tricuspid valves, with congenital heart defects. Diastolic is heard with insufficiency of the aortic and pulmonary valves, with stenosis of the left and right atrioventricular orifices.
Organic noises.
belong to intracardiac, arise due to organic changes in the valves or heart muscle. Organic changes in the heart valves lead to stenosis of the opening or valve insufficiency. With stenosis, the valve leaflets fusion (reduction of the opening), which makes it difficult for blood to pass into the ventricle of the heart or aorta. With insufficiency, wrinkled and the shortened valves do not completely close the hole and blood rushes past the damaged valves in the opposite direction (regurgitation). Due to the narrowing of the hole, the laminar movement of blood turns into turbulent, creating noise. The intensity of the noise is greater, the greater the degree of narrowing and the speed of blood movement are associated with anatomical changes in valve leaflets. Organic noises occur when the volume of blood does not correspond to the size of the hole through which it flows, against the background of other signs of cardiovascular pathology. They can be systolic and diastolic. They are louder and rougher than functional ones (functional - gentle, blowing, quiet, short) , longer lasting, carried out in other areas, do not disappear with changes in body position, deep breathing, intensify with physical activity. 1. Muscular occurs when the papillary muscles are damaged. 2. Valvular - with myocarditis, myocardial dystrophy, cardiomyopathy, cardiosclerosis - when dilation of the heart cavities and expansion of the valve ring occurs, which leads to incomplete closure of the valve leaflets.
Functional noise.
belong to intracardiac, arise due to organic changes in the valves or heart muscle. Organic changes in the heart valves lead to stenosis of the opening or valve insufficiency. With stenosis, the valve leaflets fusion (reduction of the opening), which makes it difficult for blood to pass into the ventricle of the heart or aorta. With insufficiency, wrinkled and the shortened valves do not completely close the hole and blood rushes past the damaged valves in the opposite direction (regurgitation). Due to the narrowing of the hole, the laminar movement of blood turns into turbulent, creating noise. The intensity of the noise is greater, the greater the degree of narrowing and the speed of blood movement are associated with anatomical changes in the valve leaflets. They are determined in the absence of signs of damage to the heart valves and myocardium. They are systolic, heard at the apex of the heart or on the pulmonary artery - gentle, blowing, quiet, short, not conducted outside the heart area. May disappear with changes in body position, physical activity , deep breathing. Types: 1. high-speed - due to an increase in blood flow speed during thyrotoxicosis and fever 2. anemic - due to a decrease in blood viscosity 3. dystonic - due to changes in the tone of the papillary muscles.
Systolic murmurs.
appear during systole, between the first and second sounds, are heard during narrowing of the aortic orifice and the pulmonary artery, with insufficiency of the bicuspid and tricuspid valves, with congenital heart defects.
Diastolic murmurs.
appear during diastole, between the II and I sounds, are heard with insufficiency of the aortic and pulmonary valves, with stenosis of the left and right atrioventricular orifices.
Extracardiac murmurs.
occur due to contractions of the heart or damage to neighboring organs. A-Pericardial - rough, scraping, scratching, occurs in the presence of inflammation of the pericardial layers with fibrin deposition (dry pericarditis). It is better heard in the zone of absolute dullness and at the base of the heart, is not carried out to other areas, intensifies when the body is tilted forward, pressing with a stethoscope ,sometimes determined by palpation. B-Pleurocardial - occurs with dry pleurisy in the area of contact of the pleura to the heart. Contraction of the heart increases the contact of the pericardium and pleura, which contributes to the appearance of friction noise. It is distinguished from pericardial friction noise by intensification during inspiration and localization along the left contour of the heart.
When listening to a murmur, it is necessary to determine its relationship to the phases of the cardiac cycle (systole or diastole), its properties (strength, duration, timbre), the place of best listening, the direction of its conduction (outside the heart area).
Pulse.
These are rhythmic vibrations of the artery wall caused by changes in its blood supply as a result of heart contractions.
Symmetry - comparison of the filling (height) of the pulse on both radial arteries is carried out simultaneously with both hands. Normally, it is the same. If not, there are developmental anomalies, obliteration or traumatic damage to large vessels extending from the aorta. With stenosis of the left atrioventricular orifice, the amplitude of pulse waves is the left radial artery is smaller due to compression of the left subclavian artery by the enlarged left atrium. Rhythmicity - equal intervals between pulse waves. Normally, regular or rhythmic. In pathology, it can be irregular (intervals between pulse waves are not the same) - with arrhythmias (extrasystolic, atrial fibrillation). Frequency - normally 60-80 beats per minute. May be rare - in athletes, with aortic stenosis, complete atrioventricular block. Increased frequency (tachycardia) - with physical activity, vascular insufficiency, myocardial lesions, fever. If the pulse is rhythmic, count for 15 seconds, for arrhythmia - for a minute. Filling is determined by the magnitude of the oscillations of the palpated artery during the period of its filling, depending on the stroke volume of the left ventricle. To determine, you need to squeeze the radial artery with a proximally located finger (until the pulse wave disappears), then stop the pressure and use the distal finger to evaluate the amplitude of the emerging pulse wave. Normally - satisfactory filling. Full - with large cardiac output (aortic valve insufficiency). Small (weak) - with low cardiac output (significant myocardial damage). Thread-like (barely palpable) - with acute vascular insufficiency (fainting, collapse, shock). With atrial fibrillation arrhythmia, which is characterized by the absence of atrial systole and different diastolic filling of randomly contracting ventricles; successive pulse waves are not the same in filling. The weakest ones do not reach the radial artery, therefore the pulse rate is less than the heart rate (pulse deficiency). Tension is determined by the level of blood pressure and is characterized by the force required to compress the artery (with a finger located proximally, the artery is completely compressed. The cessation of pulsation is determined by the middle finger). Normally, the pulse is not tense. At low blood pressure, it is soft, at high blood pressure, it is hard. The state of the vascular wall outside the pulse wave is determined by clamping the radial artery with the ring and index fingers until the pulsation stops. The artery is palpated with the middle finger. Normally, it is not there; with atherosclerosis, due to compaction of the arterial wall, it is in the form of a dense cord. The size, shape - increased filling and tense - large, weak filling and soft - small. Fast and high is a pulse with a sharp rise and rapid decline of the pulse wave, greater than normal amplitude (with aortic valve insufficiency, hyperthyroidism). With a slow rise and fall of the pulse wave - slow (with stenosis of the aortic mouth).
Change in heart sounds
A change in heart sounds can primarily be expressed in a weakening or strengthening of the sonority of one or both of them, in a change in timbre, duration, in their splitting or bifurcation, in some cases - in the appearance of additional tones. In this case, determining the place of best listening to pathological sound phenomena is of diagnostic importance. Strengthening of the second tone in the 2nd intercostal space on the left
speaks of its emphasis on the pulmonary artery (determined by comparing its volume and timbre on the pulmonary artery and aorta).
This indicates an increase in pressure in the pulmonary circulation, which can be observed in diseases of the heart, as well as the respiratory system (mitral defects, emphysema, pneumosclerosis, chronic pneumonia). The intensification of the second tone in the second intercostal space on the right
indicates its emphasis on the aorta, which is observed with an increase in blood pressure in the systemic circulation (arterial hypertension), as well as in the case of hardening of the wall and valve of the aorta in atherosclerosis and a number of other diseases.
Strengthening the first sound at the apex of the heart
most often occurs with narrowing of the left atrioventricular orifice (mitral stenosis), tachycardia. This is due to the fact that with this defect, during diastole, less blood flows into the left ventricle than normal, and it contracts more quickly (transition from a relaxed to a tense state). In addition, with mitral stenosis, the timbre of the first tone changes due to vibrations of the sclerotic cusps of the mitral valve. It takes on a crackling tone, reminiscent of the sound of a flag flapping in the wind. This sound at the apex of the heart with mitral stenosis is called “popping”.
Intensity of tone I (English):
Weakening of the first sound at the apex of the heart
can be observed during inflammatory processes of its muscles (myocarditis), cardiosclerosis (scar changes in the heart muscle), and damage to the valve apparatus (bicuspid and tricuspid, as well as aortic).
Weakening of the second sound on the aorta
possible with aortic defects (aortic valve insufficiency or stenosis of its mouth).
Weakening of the second tone on the pulmonary artery
occurs when the valve is insufficient or its opening is narrowed (stenosis).
If during auscultation of the heart, instead of one of the tones, two short ones are heard, following each other after a short period of time, then this indicates a split tone
.
If the difference in the time of occurrence of these components is insignificant and the impression of splitting is not created, we are talking about tone splitting
. Thus, there is no fundamental qualitative difference between bifurcation and splitting of tones. There is only some quantitative difference: splitting is the initial phase, and bifurcation is a more pronounced degree of disruption of the unity of tones.
Bifurcation and splitting of tones can be physiological and pathological. For example, the bifurcation of the first tone may depend on the non-simultaneous closure of the bicuspid and tricuspid valves as a result of changes in pressure in the chest during different phases of breathing. But more often, a split in the first tone indicates pathological changes in the heart. It occurs, as a rule, when one of the legs of the atrioventricular bundle (bundle of His) is blocked, which leads to non-simultaneous contraction of the right and left ventricles of the heart. This can occur with significant blockade of the atrioventricular (atrioventricular) node, with sclerosis of the initial part of the aorta.
Physiologically split I tone (English):
Forked I tone (English):
In case of severe heart damage, a three-part rhythm can be heard. It is caused by weakening of the myocardium (inflammation, degenerative changes, toxic lesions) of the left ventricle and occurs as a result of rapid stretching of its walls under the pressure of blood flowing from the atrium. This creates the melody of a three-part rhythm (first, second and additional third tones), reminiscent of the clatter of a galloping horse - the “ gallop rhythm.”
" It is also figuratively called the “cry of the heart for help,” since it is a sign of severe heart damage. The rhythm of the gallop is best heard directly by the ear (along with the sound, a slight impulse is perceived, transmitted from the heart to the chest in the diastole phase) in the area of the apex of the heart or the third-fourth intercostal space on the left. It can be heard especially clearly when the patient is lying on his left side. But this creates inconvenience for direct listening with the ear. In such cases, a phonendoscope is used.
There are protodiastolic, mesodiastolic and presystolic gallop rhythms (depending on the diastole phase, during which the pathological third sound appears).
Translation: gallop rhythm
heard as a three-membered or four-membered rhythm. Additional sounds appear in diastole and are caused either by atrial contraction, or early rapid filling of the ventricle, or a combination of both mechanisms (summation gallop).
Quadruple rhythm (English):
Much more common are bifurcation and splitting of the second tone, caused by non-simultaneous closure of the pulmonary artery and aortic valves due to increased pressure in the pulmonary or systemic circulation. Bifurcation and splitting of the second tone can also be physiological and pathological.
Physiological splitting of the second tone is heard exclusively at the base of the heart during inhalation and exhalation or during physical activity. At the end of a deep inhalation, when the chest expands due to a decrease in pressure in it, the blood is somewhat retained in the dilated vessels of the small circle and therefore flows in smaller quantities into the left atrium, and from there into the left ventricle. The latter, due to less blood filling, ends systole earlier than the right one, and the closure of the aortic valve precedes the closure of the pulmonary valve. During exhalation, the opposite conditions are created. In the case of increased pressure in the chest, blood, as if squeezed out of the vessels of the pulmonary circle, enters in large quantities into the left part of the heart, and the systole of the left ventricle, and therefore the beginning of its diastole, occurs later than the right.
Paradoxical splitting of the second tone (English):
Pathological bifurcation of the second tone (English):
Fixed splitting of the 2nd tone (English):
At the same time, a split second tone may be a sign of serious pathological changes in the heart and its valves. Thus, a bifurcation of the second sound at the base of the heart (second intercostal space on the left) is heard with mitral stenosis. This is due to the fact that the hypertrophied and blood-filled right ventricle ends systole later than the left. Therefore, the aortic component of the second sound occurs earlier than the pulmonary one. Bifurcation or splitting of the second sound in bicuspid valve insufficiency is associated with greater blood filling of the left ventricle than normal, which leads to prolongation of its systole, and the diastole of the left ventricle begins later than the right. Because of this, the aortic valve closes later than the pulmonary valve.
One should distinguish from the true splitting of the second tone its sound melody, which only superficially resembles splitting. An example is the additional tone that occurs during the opening of the bicuspid (mitral) valve with mitral stenosis. It has a high-pitched clicking tone and is perceived as a loud echo following the second tone. The additional tone, together with the clapping first and second, form a peculiar melody, reminiscent of the cry of a quail. Hence the name of this sound phenomenon, heard with mitral stenosis at the apex of the heart - “ quail rhythm”
" Its distribution area is extensive - from the apex of the heart up and into the axillary fossa.
Sometimes, when listening to the heart, against the background of rare and dull tones, a lonely, very loud tone appears, the so-called “gun tone” Strazhesko
. It is caused by the simultaneous contraction of the atria and ventricles, which is observed with complete atrioventricular block, i.e. when impulses from the atria do not reach the ventricles and they each contract in their own rhythm (the atria contract more often), but in some cycle their contractions coincide.
Changes in heart sounds in pathology
Previously: heart sounds.
A change in heart sounds can primarily be expressed in a weakening or strengthening of the sonority of one or both of them, in a change in timbre, duration, in their splitting or bifurcation, in some cases - in the appearance of additional tones. In this case, determining the place of best listening to pathological sound phenomena is of diagnostic importance. Strengthening of the second tone in the 2nd intercostal space on the left
speaks of its emphasis on the pulmonary artery (determined by comparing its volume and timbre on the pulmonary artery and aorta).
This indicates an increase in pressure in the pulmonary circulation, which can be observed in diseases of the heart, as well as the respiratory system (mitral defects, emphysema, pneumosclerosis, chronic pneumonia). The intensification of the second tone in the second intercostal space on the right
indicates its emphasis on the aorta, which is observed with an increase in blood pressure in the systemic circulation (arterial hypertension), as well as in the case of hardening of the wall and valve of the aorta in atherosclerosis and a number of other diseases.
Strengthening the first sound at the apex of the heart
most often occurs with narrowing of the left atrioventricular orifice (mitral stenosis), tachycardia. This is due to the fact that with this defect, during diastole, less blood flows into the left ventricle than normal, and it contracts more quickly (transition from a relaxed to a tense state). In addition, with mitral stenosis, the timbre of the first tone changes due to vibrations of the sclerotic cusps of the mitral valve. It takes on a crackling tone, reminiscent of the sound of a flag flapping in the wind. This sound at the apex of the heart with mitral stenosis is called “popping”.
Weakening of the first sound at the apex of the heart
can be observed during inflammatory processes of its muscles (myocarditis), cardiosclerosis (scar changes in the heart muscle), and damage to the valve apparatus (bicuspid and tricuspid, as well as aortic).
Weakening of the second sound on the aorta
possible with aortic defects (aortic valve insufficiency or stenosis of its mouth).
Weakening of the second tone on the pulmonary artery
occurs when the valve is insufficient or its opening is narrowed (stenosis).
If during auscultation of the heart, instead of one of the tones, two short ones are heard, following each other after a short period of time, then this indicates a split tone
.
If the difference in the time of occurrence of these components is insignificant and the impression of splitting is not created, we are talking about tone splitting
. Thus, there is no fundamental qualitative difference between bifurcation and splitting of tones. There is only some quantitative difference: splitting is the initial phase, and bifurcation is a more pronounced degree of disruption of the unity of tones.
Bifurcation and splitting of tones can be physiological and pathological. For example, the bifurcation of the first tone may depend on the non-simultaneous closure of the bicuspid and tricuspid valves as a result of changes in pressure in the chest during different phases of breathing. But more often, a split in the first tone indicates pathological changes in the heart. It occurs, as a rule, when one of the legs of the atrioventricular bundle (bundle of His) is blocked, which leads to non-simultaneous contraction of the right and left ventricles of the heart. This can occur with significant blockade of the atrioventricular (atrioventricular) node, with sclerosis of the initial part of the aorta.
In case of severe heart damage, a three-part rhythm can be heard. It is caused by weakening of the myocardium (inflammation, degenerative changes, toxic lesions) of the left ventricle and occurs as a result of rapid stretching of its walls under the pressure of blood flowing from the atrium. This creates the melody of a three-part rhythm (first, second and additional third tones), reminiscent of the clatter of a galloping horse - the “ gallop rhythm.”
" It is also figuratively called the “cry of the heart for help,” since it is a sign of severe heart damage. The rhythm of the gallop is best heard directly by the ear (along with the sound, a slight impulse is perceived, transmitted from the heart to the chest in the diastole phase) in the area of the apex of the heart or the third-fourth intercostal space on the left. It can be heard especially clearly when the patient is lying on his left side. But this creates inconvenience for direct listening with the ear. In such cases, a phonendoscope is used.
There are protodiastolic, mesodiastolic and presystolic gallop rhythms (depending on the diastole phase, during which the pathological third sound appears).
gallop rhythm
an auscultatory finding of three (triple r.) or four (quadruple r.) heart sounds;
the extra sounds occur in diastole and are related either to atrial contraction (S), to early rapid filling of a ventricle (S), or to concurrence of both events (summation gallop) . Translation: The gallop rhythm
is heard as a three-part or four-part rhythm. Additional sounds appear in diastole and are caused either by atrial contraction, or early rapid filling of the ventricle, or a combination of both mechanisms (summation gallop).
Much more common are bifurcation and splitting of the second tone, caused by non-simultaneous closure of the pulmonary artery and aortic valves due to increased pressure in the pulmonary or systemic circulation. Bifurcation and splitting of the second tone can also be physiological and pathological.
Physiological splitting of the second tone is heard exclusively at the base of the heart during inhalation and exhalation or during physical activity. At the end of a deep inhalation, when the chest expands due to a decrease in pressure in it, the blood is somewhat retained in the dilated vessels of the small circle and therefore flows in smaller quantities into the left atrium, and from there into the left ventricle. The latter, due to less blood filling, ends systole earlier than the right one, and the closure of the aortic valve precedes the closure of the pulmonary valve. During exhalation, the opposite conditions are created. In the case of increased pressure in the chest, blood, as if squeezed out of the vessels of the pulmonary circle, enters in large quantities into the left part of the heart, and the systole of the left ventricle, and therefore the beginning of its diastole, occurs later than the right.
At the same time, a split second tone may be a sign of serious pathological changes in the heart and its valves. Thus, a bifurcation of the second sound at the base of the heart (second intercostal space on the left) is heard with mitral stenosis. This is due to the fact that the hypertrophied and blood-filled right ventricle ends systole later than the left. Therefore, the aortic component of the second sound occurs earlier than the pulmonary one. Bifurcation or splitting of the second sound in bicuspid valve insufficiency is associated with greater blood filling of the left ventricle than normal, which leads to prolongation of its systole, and the diastole of the left ventricle begins later than the right. Because of this, the aortic valve closes later than the pulmonary valve.
One should distinguish from the true splitting of the second tone its sound melody, which only superficially resembles splitting. An example is the additional tone that occurs during the opening of the bicuspid (mitral) valve with mitral stenosis. It has a high-pitched clicking tone and is perceived as a loud echo following the second tone. The additional tone, together with the clapping first and second, form a peculiar melody, reminiscent of the cry of a quail. Hence the name of this sound phenomenon, heard with mitral stenosis at the apex of the heart - “ quail rhythm”
" Its distribution area is extensive - from the apex of the heart up and into the axillary fossa.
Sometimes, when listening to the heart, against the background of rare and dull tones, a lonely, very loud tone appears, the so-called “gun tone” Strazhesko
. It is caused by the simultaneous contraction of the atria and ventricles, which is observed with complete atrioventricular block, i.e. when impulses from the atria do not reach the ventricles and they each contract in their own rhythm (the atria contract more often), but in some cycle their contractions coincide.
Next: heart murmurs.
In English:
All heart sounds (English):