A defibrillator is a type of medical equipment whose purpose is to apply electric current to the heart muscle to synchronize and restore the rhythm of contractions. During the procedure, voltages of up to 1000 volts are used.
Defibrillation was first tested in 1899 on animals, and already in 1947 Claude Beck used it to restore the heart rhythm in a 14-year-old patient. In the USSR, electric current treatment began with the suggestion of V. Eskin and A. Klimov. Already by 1959, Baruch Berkowitz and Bernard Lown had determined the optimal time of exposure to electric current for different types of arrhythmia. The portable defibrillator was invented in 1965 by Frank Pantridge. The idea was born against the backdrop of the sad statistics of heart patients dying on the way to a medical facility. Unlike modern devices, the first mobile defibrillator was quite bulky - it weighed about 70 kg, and lead plates were used as “irons”. Despite the massive size of the first portable defibrillator, its functionality was sufficient to help heart patients on the road, which saved many lives.
Defibrillator, what is it? What is a defibrillator? How does he work. Defibrillator device
A defibrillator is a device that delivers a short-term powerful current pulse to the heart to stop heart rhythm disturbances.
Defibrillation is also known as cardioversion. The defibrillator has several electrodes in its device. One of them is attached to the right of the lower third of the sternum under the collarbone, the other - along the left mid-axillary line at the level of the nipple (standard location of the electrodes).
Indications for defibrillation
Main indications for defibrillation:
- ventricular fibrillation,
- arrhythmias.
How does a defibrillator work?
The first attempt at defibrillation should start with 4000 V, with subsequent attempts the charge increases to 5000-7000 V. The electrodes should be moistened and pressed tightly to the chest during the discharge.
During the discharge, safety precautions must be observed, recording devices and artificial lung ventilation devices must be disconnected. To prevent skin burns and reduce intrathoracic resistance, the electrodes must be lubricated with a special paste or gauze pads soaked in saline solution must be placed between the electrodes and the skin.
If the patient has a pacemaker, the electrodes of the device should be located at a distance greater than 12 cm from the pacemaker. While the defibrillator is in operation, it is necessary to ensure that people do not touch metal parts of the bed or the patient.
What is a modern defibrillator?
A modern defibrillator includes the following main parts:
- The defibrillator itself has the ability to discharge from external “spoons”, an electrode and from external adhesive plates;
- Cardioscope, ECG signal is carried out from spoons and from adhesive plates of the defibrillator;
- Pacemaker (pacemaker).
Factors that determine how effective the use of a defibrillator will be:
- correct placement of electrodes;
- discharge power;
- the moment of shock application relative to the phase of the cardiac cycle.
When can we expect Eriksen on the field?
This is not an easy question; on average, recovery takes up to six months. First of all, it was necessary to find out the cause of what happened and eliminate it. After which Eriksen will gradually return to normal training activity. For example, for the same Blind, a couple of months were enough for this.
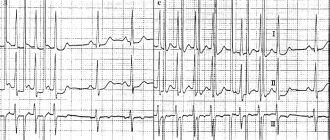
The criterion for return will be normal electrical activity of the heart on the ECG, the absence of pathological changes on the cardiogram after stress tests and the ability to tolerate their standard loads without the occurrence of any negative symptoms.
Moreover, I repeat, IKVD is installed as a last resort, it should not work every training session or game. Therefore, Christian will return to training after a full clinical recovery.
Photo: REUTERS/Wolfgang Rattay TPX IMAGES OF THE DAY, Jonathan Nackstrand, Friedemann Vogel, Hannah Mckay
Defibrillator discharge power. What is this procedure and who performs it?
First, a discharge of 200 joules (J) is applied, then the voltage can reach up to 360 J.
The technique of this procedure is a short-term effect of current on the electrical activity of the heart muscle.
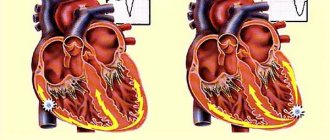
The effect of direct current goes through the anterior chest wall to the myocardium. As a result of this, heart rhythm disturbances are corrected, and the heart begins to work in the correct mode - 60-80 beats per minute and at regular intervals.
Thus, a powerful discharge simply inhibits the activity of abnormal electrical impulses in the myocardium, and brings the rhythm of its contraction to normal - sinus.
An electrical discharge is applied externally using two defibrillator electrodes, generating a bipolar pulse. They are first moistened in a special solution and then applied directly to the patient’s chest.
There are two types of stimulation of cardiac activity using electric current:
- Defibrillation.
- Cardio version.
Defibrillation is done to normalize the ventricular rhythm, and cardioversion is performed to correct the atrial rhythm.
The difference between cardioversion and electrical defibrillation lies in the specifics of the discharges used: in the first case, they are synchronized by the electrocardiogram (ECG) with ventricular complexes, in the second, they are not synchronized.
In addition, cardioversion is carried out routinely, in a clinical setting, while electrical defibrillation is a resuscitation method performed to prevent possible cardiac arrest and save lives. You need to act very quickly, as the risk of biological death increases with every minute.
The procedure does not require special preparation, since the primary goal is to preserve the patient's life. It is performed using a defibrillator. All manipulations must be done by an emergency physician, resuscitator or cardiologist. The patient's behavior is characterized by loss of consciousness. First, a discharge of 200 joules (J) is applied, then the voltage can reach up to 360 J.
Biphasic and monophasic defibrillators
Monophasic defibrillators
A single discharge is supplied from one electrode to another. When using a monophasic defibrillator, it is necessary to follow a clear pattern of electrode distribution on the patient's body.
Biphasic defibrillators
When using a biphasic defibrillator, any arrangement of electrodes is allowed. During operation, an electrical discharge is reflected from another. This allows you to receive a double shock through the muscle.
Defibrillator in the heart. What is cardiac defibrillation and how is the procedure performed?
From this article you will learn when and why defibrillation is performed. What is it, what is the algorithm. Are there any contraindications, effectiveness of the procedure, possible complications.
- Types and essence of the procedure
- Indications for use
- Contraindications
- How is emergency defibrillation performed?
- How is elective cardioversion performed?
- Possible complications
- Level of effectiveness and further prognosis
Professional defibrillator
Defibrillation is the application of an electrical shock to the heart area. It is needed to treat serious arrhythmias that cannot be controlled with medications. This procedure is part of a complex of resuscitation actions for severe cardiac arrhythmias. It is performed using a special device – a defibrillator.
Contrary to popular belief, defibrillation is not performed for cardiac arrest. In this case, only cardiopulmonary resuscitation (indirect cardiac massage and artificial respiration) is effective.
Defibrillation is performed by an emergency physician, resuscitator or cardiologist.
There are two types of electrical stimulation of the heart:
- Defibrillation.
- Cardioversion (atrial defibrillation).
Defibrillation is performed to restore ventricular rhythm, and cardioversion is performed to normalize atrial rhythm. In the second case, an electrical discharge is applied simultaneously with the QRS complex or R wave (the procedure is carried out under ECG control).
The shock is applied externally to the patient's chest using two defibrillator electrodes.
There are also implantable cardioverter defibrillators. These are special pacemakers that also have the function of immediately stopping arrhythmias (both atrial and ventricular). They are installed in patients with an increased risk of ventricular or atrial fibrillation.
Differences between cardioversion and defibrillation
Defibrillation is carried out as a resuscitation measure. Cardioversion can be carried out either urgently or plannedly (in the case of long-term attacks of atrial arrhythmias).
Indications for the use of electric shock as emergency medical care:
- Chaotic contractions of the heart (checked specifically on the chest, since there may be no pulse).
- Unconscious state of the patient.
Contraindications
There is only one contraindication to emergency defibrillation – cardiac arrest. In this case, defibrillation is simply ineffective. In case of cardiac arrest, indirect cardiac massage, artificial ventilation, and the administration of atropine and epinephrine are effective as emergency medical care.
If the heart has stopped due to ventricular fibrillation, then after its activity returns, defibrillation is already possible to normalize the rhythm. However, it is performed only after the above resuscitation measures.
Contraindications to elective cardioversion (atrial defibrillation):
- blood clots in the atria;
- accelerated AV nodal rhythm;
- polytopic atrial tachycardia;
- sinus tachycardia;
- glycoside poisoning;
- serious electrolyte disturbances;
- contraindications to the use of anesthesia (severe general condition of the patient, advanced age, etc.).
Emergency defibrillation is carried out as follows:
- The physician determines that the patient has a severe arrhythmia and is unconscious.
- The patient is placed on a hard surface.
- The chest is freed from clothing.
- The defibrillator electrodes are treated with a special conductive gel.
- Next, the electrodes are applied to the patient’s chest according to the instructions: an electrode with the inscription APEX - in the area of the apex of the heart (on the left in the 5th intercostal space), with the inscription SPERNUM - under the right clavicle. If the patient has a pacemaker, then the left electrode is installed so that there is more than 8 cm between it and the pacemaker.
- The electrodes are pressed to the body with a force of 8–10 kg.
- The device is turned on and the required charge is set (the charge power is calculated individually). Some defibrillators automatically calculate the required power.
- While the electrodes are charging, chest compressions and artificial respiration can be performed.
- Before giving a shock, the medic must make sure that no one touches the patient or the surface on which he is lying.
- To deliver a shock, press special buttons.
- After this, the pulse in the carotid artery is checked (if the patient is connected to a machine that takes an ECG, the effect will be visible on it).
- If the first discharge is ineffective, a second one with greater power is possible. While the electrodes are charging, perform cardiopulmonary resuscitation (indirect cardiac massage, artificial ventilation).
When the procedure is not done
The only contraindication to using a defibrillator is cardiac arrest. In such cases, a procedure using electric current will simply be useless. It would be better to spend this time on other, more effective methods of resuscitation in such a situation.
In case of cardiac arrest, doctors usually try to save the patient with chest compressions and artificial ventilation; the patient is administered epinephrine, adrenaline, atropine, and sodium bicarbonate.
Contraindications to elective defibrillation:
- the presence of blood clots in the atria;
- sinus or polytopic atrial tachycardia;
- electrolyte disturbances;
- contraindications to anesthesia;
- glycoside poisoning.
Defibrillator current strength.
- a medical device for influencing the heart with a short-term powerful current pulse to stop cardiac arrhythmias. The main indications for defibrillation: ventricular fibrillation, arrhythmias. The first attempt at defibrillation should start with 4000 V, with subsequent attempts the charge increases to 5000-7000 V. The electrodes should be moistened and pressed tightly to the chest during the discharge. During the discharge, safety precautions must be observed, recording devices and artificial lung ventilation devices must be disconnected. To prevent skin burns and reduce intrathoracic resistance, the electrodes must be lubricated with a special paste or gauze pads soaked in saline solution must be placed between the electrodes and the skin. If the patient has a pacemaker, the electrodes of the device should be located at a distance greater than 12 cm from the pacemaker. While the defibrillator is in operation, it is necessary to ensure that people do not touch metal parts of the bed or the patient. Defibrillation is also known as cardioversion.
Factors that determine how effective the use of a defibrillator will be
- correct placement of electrodes
- discharge power
- moment of shock application relative to the phase of the cardiac cycle
Story
In 1899 J.-L. Prévost and Frederic Batelli published the results of their research on stopping heartbeats in dogs using electric shock, including the ability to stop fibrillation. Prévost and Batelli were studying electrocution rather than defibrillation (the nature of fibrillation was only vaguely known at the time), but by 1932, D. R. Hooker and co-authors had conducted a series of shock resuscitation experiments and demonstrated the feasibility of electroshock defibrillation. Somewhat later in the USSR, in experiments on animals (dogs, cats, frogs), N. L. Gurvich and G. S. Yunyev also showed the possibility of both inducing and stopping fibrillations through the influence of current: inducing fibrillations - with a sinusoidal current, defibrillation - with a capacitor discharge , and proposed using the electrical method to restore normal activity of a fibrillating heart.
However, until the mid-1950s, cardiac fibrillation was treated worldwide only with medications (for example, the administration of potassium and calcium salts).
In 1956, Paul Zoll not only proposed the use of electric current to affect the heart muscle in cases of fibrillation, but also demonstrated the first successful experience in open heart surgery in a person using 110 volt alternating current directly to the heart muscle. Around the same time V. Ya. Eskin and A. M. Klimov manufactured the first autonomous defibrillator DPA-3 in the USSR, but reports were published only in 1962. There is also information that defibrillators have been developed in the USSR since 1952 (according to the scheme proposed by N.L. Gurvich) and have been used experimentally since 1953, but such evidence appeared in print decades later.
In 1959, based on Zoll’s publication, Bernard Lown set the goal of achieving a more effective and less traumatic effect of electric current, for which he began conducting experiments on animals. The result of his research was a monophasic form of a single pulse, later known as “English”. Lown waveform" - a single sinusoidal pulse with a half-cycle of about 5 milliseconds. In the serial device, the pulse was generated by discharging capacitors precharged to 1000 Volts through inductance and electrodes.
Continuing his research, Lown brought in the cooperation of engineer Baruch Berkowitz, who, according to the specifications presented by Lown, developed the first prototype of a defibrillator, called a “cardioverter.” This device, weighing 27 kg, provided a 100-joule pulse for open-heart use and a variable 200-400-joule pulse for closed-chest use.
But athletes constantly undergo examinations. How did it happen that a healthy person almost died?
Eriksen underwent a full range of examinations in the hospital: ECG, cardiac ultrasound (ECHOCG), electrophysiological study (EPS). The latter makes it possible to establish as accurately as possible the possible cause of electrical instability of the heart, if it is associated with pathology of the conduction system.
This is a rather complicated procedure that requires special equipment. During it, unlike a conventional ECG, the electrical activity of the heart is read directly from different parts of the heart, and not indirectly through soft tissue, which makes it possible to more accurately diagnose any disturbances in the functioning of the conduction system.
Yes, there are simpler options like transesophageal EPI, but this is still a fairly highly specific method, and, according to the latest recommendations, it remains auxiliary, that is, it is used to clarify the diagnosis when the patient has already identified any symptoms.
True, even cardiologists themselves note that methods for diagnosing cases of sudden cardiac death (as episodes similar to Eriksen’s case are called, when a clinically healthy person suddenly dies) are not enough. Simply put, even with the modern level of medicine and diagnostics, there is no 100% way to exclude cases of sudden cardiac death.
But why then annual medical examinations? Cases like Eriksen’s are 1-2 per 100,000 people on average for the entire population, and some attacks are prevented even during the examination. In-depth diagnostics allows us to identify most heart pathologies - arrhythmias, changes in heart muscle tissue (cardiomyopathy) and other diseases.
But it is impossible to achieve one hundred percent effectiveness in medicine, and some cases that do not manifest themselves for years or decades will naturally be missed. How to find something that doesn't show itself? And yes, that’s why the disease has such a formidable and mysterious name “sudden cardiac death”; in some cases, it is not possible to find out the cause of what happened even at an autopsy.
There are cases like Daley Blind - his arrhythmia appeared as a long-term consequence of myocarditis.
Conclusion? A helmet at a construction site won't save you from falling concrete slabs, but that doesn't mean you shouldn't wear one. In medicine it is impossible to achieve one hundred percent results, but it certainly does not stand still, and new technologies make it possible to identify more and more such patients.
Moreover, as we see, the precautionary measures are working, even the most extreme ones - the defibrillator was literally on the edge of the field, as was the resuscitation team.
A defibrillator does not restart a stopped heart. Defibrillator starting a stopped heart
If the heart has stopped, it can be started again using a defibrillator. Such scenes in Hollywood movies always end well. The hero lies on a hospital bed without moving and only rhythmic sound signals notify that all is not lost. And then, suddenly, the signal gets stuck on one note, and an ominous straight line appears on the monitor. Doctors burst in. One of them constantly shouts: “Defibrillator! We are losing him! And here are a few discharges, dramatic music, certainly someone’s cry “LIVE, DAMMIT YOU!”, and miraculously the heart begins to beat. The hero is saved!
And everything would be fine, but... the problem is that a defibrillator cannot be used to restart a stopped heart. Alas.
In medicine, a straight line on the monitor is called asystole and means the absence of heart contractions. The idea that these contractions can be restored by electric shock seems absolutely sound.
In order to understand why this is not so, we must first understand how the heartbeat occurs.
The heart typically receives 60-100 beats per minute from stimulating cells in the upper wall of the right atrium (sinoatrial node). These specialized cells create an electrical differential between the inside and outside of the cell membrane. At a certain moment, an impulse is sent down the heart muscle, causing it to contract. This electrical signal travels throughout the heart.
If someone goes into cardiac arrest and has no pulse, an electric shock may be needed, depending on how the conduction system works. During cardiac arrest, there may be several types of electrical rhythms.
The most common heart rhythm during cardiac arrest is called ventricular fibrillation (arrhythmic contraction of the muscle fibers of the atrium). When the sinoatrial node fails to fire, many other heart cells try to do so. As a result, multiple areas of the heart are shaken simultaneously from different directions. Instead of measured beats, we see a heart attack.
Fibrillation
With this rhythm, the heart cannot pump blood through itself. The only way to get all these different areas of the heart to work in unison again is to deliver an electrical shock more powerful than the ones they create.
When you run that kind of electricity through those cells, it activates all the electrolytes from the cells at the same time. The only hope (and this is really just a hope) is that the normal functioning of cardiac electrolytes, flowing through cell membranes in an orderly manner, will resume.
In a state of asystole, a person does not have such an electrical differential that can be shown by a heart monitor. In reality, there are simply no electrolytes inside the cell that can create an impulse. In such a situation, the discharge will not help. Thus, if asystole (the complete absence of ventricular contractions) occurs before you can use a defibrillator, all you can do is burn the heart with a high temperature from the discharge.
What does the heart need to beat?
On average, the human heart contracts 60 to 100 times per minute. This occurs due to the work of special stimulating cells in the upper wall of the right atrium (the so-called sinoatrial node). Thanks to them, an electrical differential is created between the outer and inner sides of the cell membrane. At some point, they send an impulse through the entire heart muscle to its lower part, causing the muscle to contract. It would seem that since the heart works from the impulses sent, then what is wrong with electrical stimulation from the outside? To understand this, let's move on.
The electrical differential in the sinoatrial node is created for a reason, but thanks to the presence of electrolytes potassium, sodium and calcium. The electric charge from them passes through the cell walls through special channels (each has its own). An instant before the heart muscle contracts, potassium is contained inside the cells, and calcium and sodium are outside. When sodium enters the cell, it begins to squeeze potassium out, thereby creating an electrical potential. Then channels for calcium open and it also breaks through. This creates the charge necessary for the impulse. Then the impulse from the sinoatrial node goes to the atrium, and then a pulse originates in another node (atrioventricular). Thanks to this complex circuit, blood is pumped from the upper part of the heart to the lower part, and the impulse spreads to other parts of the heart muscle. And only the correct operation of this entire mechanism can create a heartbeat.
If the system fails, different consequences are possible. But we are now interested in the state of fibrillation. This happens if the sinoatrial node does not produce the impulse necessary for the heart. Then the cells of the heart muscle try to create the necessary impulse themselves for some time, but in this case, the contraction of different parts of the heart occurs at odds (fibrillation begins) and the muscle loses its ability to pump blood. It is clear that this cannot continue for long and cardiac arrest soon occurs. But while the muscle is still in a state of fibrillation, there is hope for a defibrillator.
What is a defibrillator
A defibrillator is a medical device designed to apply electric current to the heart muscle in order to restore and synchronize its rhythm. The procedure uses high voltage (about 1000 volts). During “shock therapy,” the patient’s heart receives approximately 300 J of electricity (approximately the same amount is used by a 100-watt lamp in 3 seconds).
The defibrillation method was first used in 1899. This was a scientific study on animals. Two physiologists from the University of Geneva discovered that applying a small electrical discharge to the heart can cause ventricular fibrillation, while a more powerful current, on the contrary, eliminates this process.
The first person to experience the effect of the electric discharge procedure was a 14-year-old boy. In 1947, professor of surgical sciences Claude Bec used electric current to restore normal heart rhythm in a child. In the Soviet Union, electric current treatment was initiated by V. Eskin and A. Klimov. In 1959, Bernard Lown and Baruch Berkowitz determined the optimal procedure time for various cases of arrhythmias.
The first portable defibrillator was created in 1965. The device was invented by a professor from Northern Ireland, Frank Pantridge.
The doctor was prompted to create the device by the fact that in the 1960s, defibrillators could only be used in medical institutions, but many patients with heart disease died on the way to the hospital. Pantridge's invention was very different from modern portable devices. The device weighed about 70 kilograms, and the “irons” in it were huge lead plates. But even such a device could already be transported in ambulances, and this was its huge advantage.
Living with an ICD
Your ICD. Some facts
- The human heart is a muscle approximately the size of a fist. The heart has a complex electrical system. It produces its own electricity, which causes the heart to contract and relax at the correct rhythm. Thanks to this, the heart muscle is able to pump blood throughout the body.
- For the heart to work properly, the chambers must contract in a coordinated manner and the resting heart rate must be between 60 and 100 beats per minute.
- Electrical signals may be blocked or arrive irregularly. This causes the heart to beat too fast (tachycardia or fibrillation) or too fast (bradycardia).
- Implantable cardioverter defibrillators (ICDs) are miniature computers that fit in the palm of your hand. Typically, they are implanted under the skin in the chest area.
- ICDs help cope with dangerous disorders that result in accelerated rhythm. These disorders occur in the lower chambers of the heart (the ventricles) and are called ventricular tachycardia (VT) and ventricular fibrillation (VF).
- In ventricular fibrillation, the heart beats so fast that it flutters and loses its ability to pump blood. This condition leads to sudden cardiac arrest. If the heart is not immediately made to beat, the person will die.
- If ventricular fibrillation occurs, the ICD can send a shock to the heart muscle to stop the fibrillation or fibrillation muscle contractions.
- ICDs have saved hundreds of thousands of lives and reduced the risk of sudden cardiac arrest for patients.
Living with an ICD
An ICD is a small implantable device that looks similar to a pacemaker (pacemaker). Typically, the ICD fits easily in the palm of your hand. While pacemakers speed up slow heart rates, ICDs are designed to slow down fast rates and provide life-saving therapy when the rate is dangerously fast. ICDs have saved hundreds of thousands of lives and reduced the risk of sudden cardiac arrest for patients.
Why do I need an ICD?
The heart has a complex electrical system. It constantly produces its own electricity, which causes the heart to contract and relax at the correct rhythm. Thanks to this, the heart muscle is able to pump blood throughout the body. Electrical signals may be blocked or arrive irregularly. This causes the heart to beat too fast (tachycardia) or too slow (bradycardia). For the heart to work properly, the chambers must contract in a coordinated manner and the resting heart rate must be between 60 and 100 beats per minute.
ICDs are intended for the treatment of dangerous disorders characterized by accelerated rhythm. These disorders occur in the lower chambers of the heart (the ventricles) and are called ventricular tachycardia (VT) and ventricular fibrillation (VF). If the ventricles fibrillate, they do not contract in a normal rhythm and efficient pumping of blood is impossible. Ventricular fibrillation becomes permanent and effective pumping of blood ceases. Most doctors believe that ventricular fibrillation is a condition in which the heart beats at least 300 beats per minute. If the heart muscle flutters, it is no longer able to pump blood. If in this case measures are not taken immediately, the patient may die.
Typically, ventricular fibrillation leads to sudden cardiac arrest. It should be noted that, if assistance is provided immediately, some people can be brought out of the state of sudden cardiac arrest, despite such a formidable name. Immediate care includes cardiopulmonary resuscitation. Its task is to maintain the blood pumping process. In addition, the erratic electrical activity of the heart should be stopped, the heart's normal rhythm should be restored, and serious complications that occur during periods of significant reduction in blood flow should be prevented. This requires a four to six minute shock from an external defibrillator or implantable cardioverter defibrillator (ICD).
How does an implantable cardioverter defibrillator (ICD) work?
An ICD is a medical device that is implanted in the body to monitor the rhythm of the heart and detect certain types of potentially dangerous rhythm disorders that cause very rapid heartbeats. The ICD is implanted under the skin and connected to one or two electrodes (thin insulated wires) that are placed in or on the heart muscle. Once ventricular fibrillation occurs, the ICD can send a shock to the heart muscle to stop the fibrillation or fibrillary muscle contractions.
How does a shock restore heart rhythm?
The pattern of electrical impulses in the heart is called the heart rhythm. The ICD tracks every beat of your heart. When it senses a dangerously fast rhythm, the ICD delivers an electrical shock. This interrupts the abnormal rhythm pattern and gives the heart the opportunity to restore its normal heart rate.
What other therapy does an ICD perform?
Defibrillation is the most important function that an ICD performs. Some ICDs are also capable of performing low-energy therapy to treat less severe rhythm disorders. This type of therapy is called anti-tachycardia pacing (ATP). In addition, an ICD can stimulate the heart in the same way as a pacemaker. These devices not only help maintain your heart rate, but also store a lot of information about your heart. The collected information can be obtained by the attending physician. They will help the doctor program the device so that the therapy performed best suits your condition.
What sensations accompany the discharge?
Different people perceive shock differently, so the experience of an ICD shock varies greatly. Some people don't even feel it. Some people experience moderate intensity sensations. Others describe the shock as a shock to the chest. Although the shock may cause discomfort, it means that the ICD has responded to a very dangerous heart rhythm disorder.
How often will I receive a shock?
It depends on the characteristics of the patient. Some people live for years with an implanted ICD and have never received a shock. Others receive shocks more often. It is not unusual for ICD patients to receive one or two shocks over many years. Ask your doctor about what to prepare for, but keep in mind that even he is not able to absolutely accurately predict what kind of therapy you will need.
What to do after the discharge?
The best thing is to find a place where you can sit down and catch your breath. Very soon the normal heart rate will be restored. You may feel slightly dizzy or disorientated for a short time. Do not worry. Some patients require only a few minutes to recover, while others require several hours. Most doctors ask patients to contact them after shock. The attending physician may ask you to come to him after the discharge for control. Because your healthcare provider is aware of your clinical condition, it is best to contact your healthcare provider for instructions about post-shock behavior.
How will the ICD “understand” that a shock is not needed if the heart is beating rapidly for a natural reason?
Any person leading an active life will experience tachycardia under stress. This is fine. After stopping physical activity, a healthy heart gradually restores its normal rhythm of contractions.
Most modern ICDs are capable of distinguishing natural from pathological tachycardia. Medically speaking, a fast heart rate caused by exercise differs from a potentially dangerous fast heart rate in the area where electrical impulses are generated in the heart. During physical activity, a healthy heart generates electrical impulses in its upper chambers. After this, the impulses are transmitted along the conduction pathways of the heart to the lower chambers, causing them to contract. Dangerously fast rhythms originate in the ventricles. To distinguish between these pulses, ICDs use formulas called “discriminators.”
How is an ICD implanted?
Generally, cardiac device implantation does not require general anesthesia. Usually, pain relief while maintaining consciousness is sufficient for implantation. You will receive medication to help you relax, but during the procedure you will remain aware of everything that is happening and will be able to hear and even talk to the doctor and nurses. Several medications will be administered when the incision is made. Although the local anesthetic will prevent severe pain, you may feel some pressure when the device is implanted.
What to expect during ICD implantation surgery?
First, the doctor will make a small incision in the upper chest and find a vein. A small puncture will be made in the vein, and then long flexible wires will be passed through the vein into the heart. The operating team monitors the progress of the electrode using a high-mounted monitor called a fluoroscope. The monitor shows a moving image in the X-ray part of the spectrum. Often the placement of the electrodes is the longest part of the operation. Once the electrodes are placed, your doctor will check them to make sure the electrodes are positioned optimally to deliver energy to the heart.
Once the electrodes are placed, your doctor will connect you to the implantable device. Then the doctor, separating the skin and underlying tissue from the underlying muscle, will form a “pocket.” Once the ICD is connected to the leads, it is placed in a pocket. After placing the device, the doctor will stitch the incision.
After the incision has healed, many people barely notice the small scar and slight protrusion. However, if the patient is short or thin, the device may protrude a little more. If you are concerned about how you will look after surgery, discuss this with your doctor. Sometimes the device can be placed in another place where it will not be so noticeable.
The length of surgery depends on the type of device being implanted, as well as your anatomy and the time spent determining the optimal position of the electrodes. Typically, ICD implantation lasts several hours.
What to expect after surgery?
Immediately after surgery, you will be taken to the intensive care unit. You may experience increased sensitivity at the implantation site for some time. You will stay in the hospital for anywhere from several hours to several days. Discuss the specifics of your case with your doctor.
During the postoperative period, carefully follow all instructions from your doctor. First, be sure to report any redness, tenderness, or tenderness near the implant site. If you notice redness or tenderness around your scar after leaving the hospital, contact your doctor immediately without waiting for your appointment.
How long will the recovery period last?
Because every patient is different, it will be difficult to accurately determine the length of the recovery period in your specific case. Follow your doctor's instructions carefully. For some time after surgery, your usual activities will be limited. Once your recovery period is complete, your doctor will be your best source of advice on how to resume your normal lifestyle.
What are the risks of using an ICD?
Your doctor is the best person to tell you about the risks of using an ICD. Do not forget to ask him all the questions you have and share all your doubts. A small number of patients with ICDs develop complications related to the implantation procedure. These complications include infection, a reaction to drugs used during surgery or to the device itself, blood loss, or damage to a blood vessel, heart wall, or other organs.
After the operation, you will experience some discomfort and loss of strength. Once you recover, you will feel better. However, some patients continue to experience discomfort at the ICD implantation site. If you also feel discomfort, tell your doctor about it. After ICD implantation, it is important to take certain precautions. You can safely use most appliances that are in working order and properly grounded, but you should avoid strong magnetic fields, including MRI devices. Your doctor will discuss any necessary precautions with you. In addition, you should carefully read all brochures supplied with your product, paying particular attention to the “Caution” and “Attention” sections. These sections contain important safety information.
ICD therapy may not stop the arrhythmia. Moreover, there is a possibility that therapy will make it worse. However, in an attempt to control the arrhythmia, the ICD will deliver more intensive therapy. There is a small risk that the ICD may fail to deliver needed therapy or provide therapy when it is not needed. An ICD does not always eliminate all symptoms of an arrhythmia. You may continue to feel dizzy or faint.
How often should I visit my doctor after implantation?
For routine check-ups, you will need to see a cardiologist or GP regularly. Immediately after surgery, you may need to visit your doctor several times. All of these visits are very important because they will allow the doctor to ensure that the implanted device is functioning correctly. The necessary adjustments are made painlessly in the doctor's office using a desktop computer called a programmer. Your doctor will also check whether your incision is healing. After this, you will visit your doctor regularly for follow-up examinations. Your doctor will advise you how often to do them. If the situation is stable, your doctor may suggest that you visit him once or twice a year or after you receive a shock. Your doctor may also need to see you if your family or GP has any concerns.
If many changes were made during your visit to the doctor, you may need to make your next visit a shorter period of time to ensure that the changes are effective and that there are no problems associated with them.
How is the inspection carried out?
The follow-up examination is absolutely painless and usually takes less than half an hour. During the examination, the doctor or nurse will place a sensor on the area of skin located over the implanted device. This sensor is similar in size and shape to a TV remote control.
Some devices do not require a sensor because they transmit information remotely. The device reports battery status information to the programmer, performs other system checks, and reports your heart rate information accumulated since your previous health check. If you have experienced a shock or therapy in the past time, the programmer will receive this information.
If necessary, the doctor can change some device settings to optimize therapy. For these reasons, it is very important that you follow your follow-up inspection schedule.
How will the doctor replace the battery in my device?
Implanted devices are powered by special batteries that are designed to last for a long time. These batteries do not die suddenly like flashlight batteries, but provide multiple warnings that the end of their life is approaching. Monitoring the condition of the batteries by the attending physician is part of the routine follow-up examination. Most devices' batteries last between three and six years, although this depends on the device and how often it sends electrical impulses to the heart. Once the device warns that the battery is low, your healthcare provider will schedule a replacement. Implantable devices are sealed, so batteries cannot be replaced. Instead, the doctor implants a new device. As a rule, this operation takes less time than the first one, since the doctor only needs to connect the new device to the existing cardiac electrodes.
Will an implantable device change my life?
You can live longer, healthier, more productive and happier. After surgery, you should limit your exercise for a while. Make sure you carefully follow all your doctor's instructions. Very soon you will be able to do everything you did before, and even more.
Should I stay away from devices like microwaves, magnets, and strobe lights?
Implantable devices cannot be damaged by working appliances such as microwave ovens, electric blankets, and most power tools. Using electric arc welding equipment or working with vehicle ignition systems will also not cause harm to the ICD. However, they may cause short-term interference with the proper operation of the device. Some medical equipment may also interfere with ICD operation. If you experience dizziness or palpitations (fast, irregular heartbeats), simply turn off the electrical equipment or move away from it. After this, the implanted device will restore normal functioning. If you must use equipment that may cause EMF, consult your healthcare professional. You can also request instructions from the equipment manufacturer.
Will medical equipment interfere with my ICD?
Although medical equipment generally does not interfere with ICD function, some devices can interfere with its function. Before you undergo any medical, including dental, procedure or test, such as electrosurgery, electrocautery, lithotripsy, or radiation therapy, tell your healthcare provider that you have an ICD implant.
Even with the ICD turned off, any diathermy is contraindicated for you. This procedure can damage the tissue around the implanted leads or permanently damage the ICD. Try to stay away from transcutaneous neuro- and myostimulation (TENS) devices. They may interfere with the operation of the ICD. Magnetic resonance imaging (MRI) scanners can seriously damage the ICD. When approaching or standing in the MRI room, the ICD may not function properly.
Can I use a mobile phone?
Mobile phones that send electromagnetic pulses can interfere with the normal functioning of the device. However, you can minimize the risk by taking simple precautions, such as not carrying your phone in your chest pocket above the ICD and keeping the device near the ear farthest from the ICD. ICDs contain special filters that protect devices from interference generated by mobile phones.
Will my iPod® or other portable media player affect the performance of my ICD?
There is no evidence that a portable media player such as an iPod or MP3 interferes with the normal functioning of the devices.
When can I resume physical activity?
Ask your doctor if you can resume physical activity. It is important to avoid shock to the area of the implanted device. So it's best to avoid contact sports like football. Otherwise, the device or electrodes may be damaged. After implantation, you may have more energy. Many people believe that by reducing the severity of symptoms, strength increases.
Can I do activities that require intense physical activity, such as hiking, skiing, or jogging?
It is best to always discuss your plans with your doctor. The doctor will give you advice about intense physical activity based on knowledge of your capabilities and condition. If the sport you play involves stress on your arm or chest (such as swimming or golf), you may want to discuss your pre-implant exercise with your doctor. This may influence the choice of device type and implantation site.
Is sex safe for me?
Typically, the implanted device does not have a negative impact on the patient's sex life except for a short period of hospital stay and recovery. However, it is important to follow your doctor's instructions about resuming physical activity.
Will I be able to drive a car?
Talk to your doctor about this. Keep in mind that although an ICD can stop fast heartbeats, it may not be able to prevent symptoms associated with the rhythm (such as dizziness and fainting). Before driving again, discuss the advisability of doing so with your doctor.
Can I travel?
Your doctor will best answer this question. Many ICD patients find that with a little more care and planning, they can enjoy traveling to many parts of the world. It always makes sense to plan your route carefully and leave a copy of the program with your loved ones. Just in case of difficulties along the way.
Will airport security systems affect the performance of my device?
Many patients are concerned about the security systems used at airports. They worry in vain. Indeed, security rules at airports have become stricter, but having an implanted device will not bring any additional inconvenience. It is best to go through the airport metal detector at normal speed. If an alarm sounds (which is completely optional), this only means that the system has detected the presence of metal in the implanted device.
Please present your patient card for screening. Ask for a manual search.
A security officer may use a hand-held metal detector. In this case, be sure to inform the supervisor that this procedure must be performed quickly and the sensor should not be held over the implanted device for more than a second.
What else should I know about traveling if I have an implanted device?
When traveling, be sure to carry important medical information with you, such as the names and dosages of medications, the name and telephone number of your doctor, and emergency medical care information. Also ask your healthcare provider for a copy of the most recent printout of the programmer test data and settings made during the last test. If you are traveling to a country that speaks Spanish, French or German, your doctor may be able to give you a printout in the appropriate language. (Some devices may soon be able to print in Italian, Japanese and Chinese.) Carry enough medications with you. If you are traveling by train or plane, keep some of your medications in your carry-on luggage and some in your suitcase.
Finally, let the attendants know if you have special dietary needs and develop healthy eating habits while on the road.
Do I need to take medications after ICD implantation?
Ask your doctor this question. Typically, an implanted device does not replace medications. Instead, the drugs and the implanted device work together. However, your doctor may adjust the dose.
Are there any food restrictions?
In general, to keep your heart healthy, doctors recommend eating foods that are low in sodium, fat, and sugar and rich in fiber and carbohydrates.