Medical editor: Druzhinkina V.Yu., neurologist. November, 2020.
Synonyms: intracranial hypertension, liquor-hypertensive syndrome, liquor hypertension syndrome, intracranial hypertension, intracranial pressure, ICP. ICD-10 code: G93.2.
Intracranial hypertension is an increase in cerebrospinal fluid pressure inside the skull. The leading symptoms are intense headaches in the frontoparietal region and a feeling of pressure on the eyeballs. The basis of therapy is the use of diuretics designed to reduce intracranial pressure due to the excreted fluid.
Intracranial hypertension is not an independent disease; it is a syndrome that accompanies a number of diseases/injuries of the skull and brain. Separately, primary or idiopathic intracranial hypertension is distinguished, the causes of which are not precisely established. This pathology is diagnosed after excluding other possible factors for increased intracranial pressure (ICP).
***
Intracranial pressure is the difference between the pressure in the skull and atmospheric pressure, that is, this term determines the force with which the intracranial fluid presses on the brain. Normal values for this difference are in the range of 5-15 mm Hg. pillar When intracranial pressure increases, they speak of intracranial or intracranial hypertension.
The brain is protected from mechanical stress and shock by the skull, as well as by a liquid medium - cerebrospinal fluid or cerebrospinal fluid. It is located in the subarachnoid, epidural spaces (cavities between the meninges) and in the cerebral ventricles (cavities located in the brain tissue). The brain, cerebrospinal fluid and intravascular blood are in dynamic equilibrium. When the pressure level of one of the components changes, the pressure in the others is transformed, which is ensured by the properties of blood and brain fluid (maintaining acid-base balance), the elasticity of the walls of blood vessels and brain tissue. When exposed to certain causes, the regulation of intracranial pressure occurs, which leads to the development of cerebrospinal fluid hypertension.
General information
Intracranial hypertension is a pathological condition (syndrome) manifested by increased intracranial (intracranial) pressure.
Intracranial hypertension syndrome (syn. liquor-hypertension syndrome) is quite common in adult and pediatric neurology and can be either idiopathic or develop with a variety of brain lesions and skull injuries. The most common cerebral hypertension of unknown origin is idiopathic (primary) intracranial hypertension (ICH), which is classified as benign intracranial hypertension (ICD-10 code: G 93.2). As a rule, this diagnosis is made only after there is no confirmation of the specific causes of hypertension (the presence of a space-occupying formation in the cranial cavity, vein thrombosis, infectious lesions of the brain, etc.).
Determination of intracranial pressure (ICP) and its physiological norm
Intracranial pressure is the difference between atmospheric pressure and pressure in the cranial cavity (epidural/subarachnoid spaces, meningeal sinuses, ventricles of the brain). The level of intracranial pressure is formed by cerebrospinal fluid (CSF) circulating in the structures of the central nervous system and arterial/venous blood entering the brain.
These fluid environments are in constant motion (spinal fluid circulates through the ventricles of the brain/spinal canal, and blood through the vascular bed). Normally, the physiology of the circulation of fluid media in the brain is determined by:
- Mean arterial pressure, i.e. the average value (difference) between the systolic/diastolic blood pressure of arterial blood entering the skull, which is normally 80 mm Hg. Art.
- The average venous pressure at the exit of the skull, which is normally 0 mm Hg. Art., that is, there is no resistance to blood flow.
- The average cerebrospinal fluid pressure in the skull, which is external in relation to the brain and is equal to 10 mm Hg. Art. It is the cerebrospinal fluid pressure that has a constant compressive effect on the brain (creates constant ICP). The biomechanical balance normally present in the skull maintains the average cerebral tissue pressure at a level of 10 mmHg. Art. In a healthy adult, the total volume of circulating cerebrospinal fluid averages 150 ml, while ICP remains normal. Its slight increase is compensated by its resorption by brain tissue and outflow from the cranial cavity to the spinal cord along the liquor subarachnoid ducts through all parts of the spine, up to the sacral outlet openings.
The constant pressure inside the cranium is maintained by the formation of reserve spaces due to a decrease in the volume of CSF, as well as the cerebral blood fraction. In cases of an increase in any of the components occurring against the background of various pathologies (excessive accumulation of CSF, cerebral edema , cerebral hyperemia , impaired venous outflow), as well as with the development of pathological volumes (tumors, hematomas, parenchymal hemorrhage, abscess), a conflict occurs between the intracranial components and hypertension develops .
An increase/decrease in ICP can be observed both during natural physiological processes in the human body ( coughing , loud screaming, sneezing , crying, straining, physical/nervous strain, sudden bending forward), and indicate pathology. Normally, in an adult, the pressure inside the skull should not exceed 10–15 mmHg. ICH refers to a persistent increase in ICP to a level of 20 mm or higher. rt. Art. The severity of intracranial hypertension is presented in the table below.
How can you measure VD?
In specialized medical institutions, invasive techniques are used to measure the pressure inside the ventricles of the brain using specialized pressure sensors that are inserted into the cerebral ventricles (a catheter is inserted and connected to the sensor). Sensors can also be installed subarachnoidally, subdurally, or epidurally. This procedure has a low risk of brain injury. In practice, intracranial pressure is in most cases measured indirectly using a spinal puncture, measuring it at the level of the lumbar spine in the spinal subarachnoid space.
Why is intracranial hypertension dangerous?
The severity and specificity of disorders in ICH are determined by the degree of increase in ICP, its nature (diffuse/local) and localization, as well as the duration of the impact of increased ICP on brain structures. And if, with a weak and unstable degree of increase in ICP, no significant changes are observed, then in patients with a stable increase in ICP of moderate and severe degrees it can cause serious disorders - headaches (tension, ischemic), disturbances in fine motor skills of the hands, vision, hearing, hypertonicity of the upper muscles / lower extremities, skeletal muscle rigidity, convulsions , paresis , disturbances in emotional manifestations (sleep, behavior), fatigue, delayed speech development, neurogenic disorders of the cardiovascular and respiratory systems (vegetative-vascular dystonia , pain in the heart, bradycardia / tachycardia , arrhythmias , low-grade body temperature , breathing rhythm disturbances - shortness of breath , apnea ) and others.
Benign intracranial hypertension
First of all, what is it? As already noted, benign ICH is a condition characterized by a persistent increase in cerebrospinal fluid pressure in the absence of intracranial mass formation, vein thrombosis and abnormalities in the composition of the cerebrospinal fluid. Since intracranial hypertension of a specific origin can be considered within the framework of a particular pathology/disease, we will consider only idiopathic (benign) ICH.
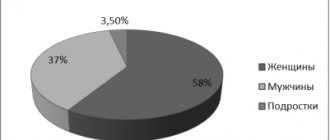
The primary syndrome of idiopathic intracranial hypertension (IIH) today means a condition that is accompanied by an increase in ICP without identified etiological factors (possibly due to obesity ). The incidence rate of IIH is 0.7–2 cases/100,000 population.
This type of hypertension most often occurs in young women who are overweight. Much less common in children and men. The most typical symptoms of idiopathic liquor hypertension are headache and transient (transient) visual disturbances in the form of deterioration in image sharpness, blurring, double vision, and in 30-35% of patients there is a decrease in visual acuity.
Diagnostics
In the diagnosis of pathology, it is important to collect the patient’s complaints and medical history, conduct a neurological (identification of pathological reflexes and symptoms) and ophthalmological examinations. When examining the fundus, dilation and tortuosity of the veins, their plethora, and swelling of the optic disc are revealed.
Instrumental research methods:
- Echoencephalography. Allows you to obtain indirect data on brain function, which should be compared with the clinical picture.
- X-ray of the skull. Signs of intracranial hypertension in the form of digital impressions on the bones of the skull.
- , MRI of the brain. They allow you to evaluate the bones of the skull, brain tissue, its blood supply, identify the presence of infarctions and hemorrhages, neoplasms, expansion of the ventricles of the brain and interthecal spaces.
- Ultrasound of the head and neck vessels. Helps to establish a disorder of the venous outflow from the brain.
For idiopathic intracranial hypertension, a lumbar puncture is performed, followed by a study of the biochemical composition of the cerebrospinal fluid, in which the main indicators (electrolytes, sugar, proteins and cells) exceed the norm. A needle is inserted into the lumbar region to collect cerebrospinal fluid.
Also, the study of cerebrospinal fluid allows us to clarify the genesis of secondary intracranial hypertension (infectious, oncological, vascular).
Important! In case of acute pathology, lumbar puncture is contraindicated due to possible complications.
Differential diagnosis of primary intracranial hypertension is carried out with an epileptic seizure and toxic or metabolic dysfunction of the brain.
In epilepsy, there is a cyclical pattern of convulsive seizures, which are visible during echoencephalography. Convulsions are clonic in nature, there are sudden unstable changes in heart rate and blood pressure. Also, seizures in epilepsy are accompanied by salivation without swallowing (foaming from the mouth), and there is a history of epileptic seizures.
In acute poisoning and generalized infections, incoherent speech, confusion and disorientation, and anxious agitation are observed.
Pathogenesis
The pathogenesis of increased ICP in adults may be based on various mechanisms - edema/swelling of the brain, an increase in the mass of the contents of the cranium ( tumor , hematoma , abscess ), difficulty in the outflow of cerebrospinal fluid, disturbances in the venous outflow of the cerebral blood fraction). Within one article, it is not possible to consider the pathogenesis of high-frequency hypertension in a particular pathology, so we will only consider the pathogenesis of the development of high-frequency hypertension with cytotoxic cerebral edema .
Understanding the development of increased intracranial pressure (ICP) is based on a model of progressive cerebral edema, based on the theoretical Monroe-Kelly model, which is based on the thesis of a close relationship between the rigid cranium of an adult and components such as the brain, blood, and cerebrospinal fluid. The basis of such a connection is the interaction of any of the components with the others, manifested by a reaction to an increase in one of them by a corresponding (proportional) decrease in the volume of the other, due to which the constancy of intracranial pressure is maintained.
cytotoxic edema due to disruption of the transmembrane transport of electrolytes . Edema cells, due to their increased volume, exert a compressive effect (pressure) on neighboring cells, thereby promoting the spread of edema to intact cells (mass effect).
As the pathological volume of cells with cytotoxic edema increases, compression develops in the capillary-pial bed system, which leads to disruption of microcirculation and the development of hypoxemia / ischemia in areas of the brain that are not directly related to the primary mass effect, that is, this leads to pathological separation of different sections of the contents of the cranium. As a result, the pressure created by the pulse oscillations of the arteries and the cerebrospinal fluid loses the ability to spread freely along the tissues and spaces of the cerebrospinal fluid located inside the skull/spinal canal. This leads to the emergence of a difference in parenchymal pressure between intact and those involved in edema of the brain structures, which initiates its dislocation in the direction of relatively low pressure.
As a result of this process, diffuse edema of the entire brain develops and its gradual dislocation (movement in the direction of the foramen magnum (the only open exit from the cranium). As a result, various types of dislocation occur. More often, this is a hernial protrusion into the tentorial notch of the middle-basal parts of the temporal lobes and compression of the mesencephalic structures of the brain stem with inhibition of the primary circulatory/respiratory centers and a sharp disruption of brain function, up to the cessation of its vital activity. Neurological symptoms manifest themselves at the stages of cerebrovascular accident. The figure below shows a diagram of the progression of ICP and the stages of the cerebral protection mechanism.
Causes of development and risk factors
Due to its occurrence, intracranial hypertension is divided into:
- primary (idiopathic);
- secondary.
According to the speed of occurrence, the pathology can be
- acute, when an increase in intracranial pressure develops rapidly (brain infection, trauma, acute circulatory disorder);
- chronic - intracranial pressure increases gradually as the brain tumor grows or due to residual effects after trauma, surgery, or stroke.
An increase in intracranial pressure is facilitated by an increase in the volume of any structure that is located in the cranium (vessels, brain tissue, cerebrospinal fluid depot and the cerebrospinal fluid itself). As a result, compression of the brain occurs, which leads to metabolic disorders in its cells, displacement of brain structures and disruption of vital functions (respiratory, cardiac). This happens due to compression of the brain stem, which contains the respiratory and cardiovascular centers.
Photo: example of compression of the brain in the case of hydrocephalus
In this regard, all triggers leading to intracranial hypertension are divided into 4 groups.
Vascular pathology
Conditions that cause excessive blood filling of the brain:
- increased temperature (hyperthermia);
- hypercapnia (excess CO2, for example, in case of impaired pulmonary ventilation, poisoning with drugs, alcohol, toxic substances).
Conditions that interfere with the flow of blood from the brain:
- encephalopathy;
- cervical osteochondrosis.
Edema of the brain or its membranes
It can be diffuse (widespread) and local (local).
Observed in the following conditions:
- brain contusions;
- ischemic stroke (due to hypoxia);
- infectious diseases (encephalitis, arachnoiditis, meningitis);
- severe hypoxia caused by any pathologies;
- hepatic encephalopathy.
Volumetric formations in the skull
The most common reasons:
- brain tumor (primary or metastatic);
- cyst, including parasitic origin (echinococcosis);
- aneurysms of cerebral vessels;
- brain abscess.
Liquorodynamic disorders (cerebrospinal fluid hypertension)
May be caused by excess production of cerebrospinal fluid, impaired absorption or circulation disorders (hydrocephalus).
Factors contributing to the occurrence of primary cerebrospinal fluid hypertension have not been sufficiently studied. Most often this pathology is diagnosed in women and is caused by weight gain. Intracranial hypertension is also observed in overweight teenage girls, in the case of venous sinus thrombosis due to hemorrhagic diathesis, when taking vitamin A in increased dosages, treatment with tetracycline, penicillins or after discontinuation of glucocorticoids, with hypo- and hyperthyroidism, pregnancy, cycle disorders.
Causes
Intracranial hypertension in adults can be caused by many different causes, the diversity of which can be grouped according to the mechanism of development of the pathology:
- Intracranial space-occupying formations causing an increase in ICP ( benign/malignant tumor intracranial hematoma , parasitic cyst , abscess );
- Cytotoxic cerebral edema caused by hypoxic damage to cells of brain structures (severe respiratory failure after cardiac arrest), early stage cerebral ischemia hepatic / renal encephalopathy , hyponatremia , Reye's syndrome , syndrome of inadequate production of andidiuretic hormone ).
- Vasogenic cerebral edema caused by damage to the blood-brain barrier (infectious diseases - meningitis / encephalitis , intracranial trauma - bruises, concussions, birth injuries), hematomas , ischemic / hemorrhagic stroke .
- Interstitial edema caused by impaired outflow of cerebrospinal fluid ( occlusive hydrocephalus ).
Symptoms
The formation of clinical hypertension syndrome and the nature of its manifestations depend on the localization of the pathological process, its prevalence and speed of development.
Intracranial hypertension syndrome manifests itself with the following symptoms in adults:
- Headache of increased frequency or severity (increasing headache), sometimes awakening from sleep, often forced positioning of the head, nausea, and repeated vomiting. It can be complicated by coughing, a painful urge to urinate and defecate, and actions similar to the Valsalva maneuver. Possible disturbances of consciousness and convulsive seizures. With prolonged existence, visual impairment occurs.
- History may include trauma, ischemia, meningitis, cerebrospinal fluid shunt, lead intoxication or metabolic disorder (Reye's syndrome, diabetic ketoacidosis). Newborns with cerebral ventricular hemorrhage or meningomyelocele are predisposed to intracranial hydrocephalus. Children with blue heart disease are predisposed to an abscess, and children with sickle cell disease may have a stroke leading to intracranial hypertension.
Objective signs of intracranial hypertension are swelling of the optic disc, increased cerebrospinal fluid pressure, increased osmotic pressure of the extremities, and typical x-ray changes in the bones of the skull. It should be borne in mind that these signs do not appear immediately, but after a long time (except for increased cerebrospinal fluid pressure).
There are also signs such as:
- loss of appetite, nausea, vomiting, headache, drowsiness;
- inattention, decreased ability to awaken;
- papilledema, upward gaze paresis;
- increased tone, positive Babinski reflex;
With a significant increase in intracranial pressure, disturbances of consciousness, convulsive attacks, and visceral-vegetative changes are possible. With dislocation and herniation of brain stem structures, bradycardia, respiratory failure occur, pupillary response to light decreases or disappears, and systemic blood pressure increases.
Symptoms of increased intracranial pressure
Symptoms of intracranial hypertension in adults are manifested mainly by headaches of varying intensity. The pain syndrome is characterized by pronounced intensity in the morning, increased pain when tilting the head/coughing, sometimes the pain can be accompanied by nausea and, less often, vomiting.
Visual disturbances are especially characteristic of idiopathic ICH, which manifest themselves as transient darkening (fogging) of the eyes and are present in 48-55% of cases. Many patients complain of pain behind the eyeballs/pain when moving the eyeballs. Sometimes visual disturbances can be precursors to headaches. Signs of intracranial hypertension may also include complaints of noise in the head, photopsia , diplopia (double vision) and progressive decrease in vision.
Acute, rapidly increasing intracranial hypertension often leads to short-term loss of consciousness up to coma . With chronic ICH, there is a progressive deterioration in the general condition in the form of sleep disturbances, irritability, and mental/physical fatigue. Indirect signs of hypertension include increased meteosensitivity (reaction to weather changes), rapid heartbeat, increased sweating , loss of appetite , and drowsiness . The severity of clinical manifestations is largely determined by the nature/severity of the underlying disease, as well as the rate of increase in ICP.
Prognosis and prevention
The prognosis of liquor hypertension depends on the rate of increase in intracranial pressure, timely and adequate treatment, as well as on the individual compensatory characteristics of the brain. With the development of dislocation syndrome, the prognosis is unfavorable, with a high probability of death.
With regard to idiopathic intracranial hypertension, with regular courses of lowering ICP, the prognosis is favorable, in some cases spontaneous remission is observed.
Foreign studies show that moderate weight loss (5-10%) may be sufficient to reduce the signs and symptoms of intracranial hypertension. If lifestyle changes do not lead to weight loss and ICP reduction, then weight loss surgery may be recommended for patients with a BMI over 40.
Prevention measures include a timely visit to the doctor if a headache, a feeling of pressure on the eyes, deterioration of vision occurs, normalization of sleep, rest, elimination of stress and bad habits, and maintaining a healthy lifestyle.
Sources:
- 1, 3. Idiopathic Intracranial Hypertension. — National Eye Institute, USA, 2014.
- Dr. Michael Wall. Idiopathic Intracranial Hypertension Treatment Trial (IIHTT). — University of Iowa Hospitals and Clinics, 2009-2018.
Intracranial hypertension in children
Increased HF in infants and children of the first years of life can be caused by: unfavorable course of pregnancy (infectious diseases of the woman during this period, intrauterine hypoxia), difficult birth accompanied by birth injuries, oxygen starvation during childbirth, congenital anomalies/malformations ( hydrocephalus ), prematurity, neuroinfections, inflammatory diseases of the membranes of the brain ( encephalitis , meningitis ).
As a rule, ICH in children of the first years of life is manifested by regurgitation, general anxiety, autonomic disorders (increased sweating , marbling of the skin, etc.), sleep disturbances, rapid increase in head circumference, pulsation/tension of the large fontanel, tremor of the chin/hands, weather sensitivity, symptom Graefe (when moving the gaze downward, a lag of the upper eyelid from the iris is noted). If such symptoms are present, parents should contact a pediatric neurologist.
Complications
The brain is a vulnerable organ. Prolonged compression leads to atrophy of the nervous tissue, which means that mental development and the ability to move suffer, and autonomic disorders occur.
If you do not contact a specialist in time, compression will occur. The brain may be forced into the foramen magnum or into the notch of the tentorium cerebellum. This compresses the medulla oblongata, where the centers of respiration and circulation are located. This will lead to the death of a person. Pressing into the notch of the tentorium is accompanied by constant drowsiness, yawning, breathing becomes deep and rapid, the pupils are noticeably constricted. Wedging of the hippocampal hook occurs, a symptom of which is dilation of the pupil or the absence of a light reaction on the side of the damage. An increase in pressure will lead to dilation of the second pupil, disruption of the breathing rhythm and coma.
High intracranial pressure is always accompanied by loss of vision due to compression of the optic nerve.
Consequences and complications
A long-term (chronic) increase in ICP, even with minor deviations from the norm, negatively affects the function of the central nervous system and is manifested by signs of nervous exhaustion: irritability , frequent headaches, sleep disturbances, increased fatigue, decreased physical/intellectual performance, decreased cognitive functions (decreased concentration, memory , weakening of intelligence). With a significant increase in ICP, there is a high risk of developing visual impairment and epileptic seizures.
List of sources
- Skvortsov I.A. Developmental neuroscience: a guide for clinicians. M.: Litterra, 2008. - 544 p.
- Bashkirov M.V., Shakhnovich A.R., Lubnin A.Yu. Intracranial pressure and intracranial hypertension // Ros. magazine anesthesiol. and intensive ter. - 1999. - No. 1. - P. 4-11.
- Krylov V.V., Talypov A.E., Puras Yu.V. Intracranial pressure in brain injuries // Neurosurgery: scientific and practical. magazine - 2007. - No. 4. - P. 12-19.
- Gasparyan S.S., Eliseeva N.M., Tanyashin S.V. Clinical recommendations. Diagnosis and treatment of benign intracranial hypertension. M. 2015. 17 p.
- Sergeev A.V. Idiopathic intracranial hypertension. Journal of Neurology and Psychiatry. S.S. Korsakov. 2016; 116(5): 93–97.