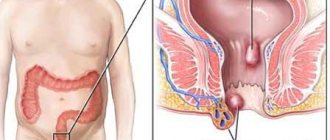
Anal fissure: forms of the disease
There are acute and chronic anal fissures. If a rectal fissure exists for more than 4 weeks, then this is a chronic form of the disease. Morphological changes occur: the edges of the crack thicken, scars and tubercles appear. Chronic anal fissure cannot be cured using conservative treatment methods; surgical methods are required.
Chronic anal fissure is a fairly common disease. It occurs in 2-2.5% of adults. It accounts for 12-15% of all proctological diseases (this is 3rd place after hemorrhoids and paraproctitis).
What is important to know about therapy?
The use of minimally invasive techniques is the main standard of modern proctology, since in most cases they allow you to get rid of hemorrhoids and anal fissure in one visit. A full examination and laboratory tests must be carried out first. To ensure maximum comfort during a proctological examination and obtain reliable medical information, special preparation is recommended. To do this, you need to cleanse the intestines with an enema or special laxatives prescribed by your doctor. After this, he will determine how to treat hemorrhoids and anal fissures, taking into account the existing indications.
Possible complications of anal fissure
An anal fissure left untreated can cause the following complications:
- massive bleeding;
- rectal fistula;
- ascending (moving up the intestines) inflammation of the mucous membrane (sphincter, rectum, sigmoid colon);
- paraproctitis (inflammation of fatty tissue around the rectum);
- in men – prostatitis (if inflammation has spread to the prostate gland).
What is excision of a rectal fissure, and how does it happen during surgery?
In order to better understand what evaporation of an anal fissure is and how it happens during the operation, you should familiarize yourself a little with the principles of the impact of various energies (laser, radio frequency) on living tissue.
In hardware medicine, which now rightfully occupies a leading position not only in the aesthetic sphere, but also in general medical practice, there is such a concept: selective thermolysis. Selective means selective. Lysis means destruction. Purposeful destruction of what the patient came to get rid of. Thermolysis means destruction under thermal (thermal) influence. But unlike classical surgical excision with a scalpel, such destruction of any defect is gentle, gentle in relation to healthy tissues in particular, and the entire body as a whole.
Radiosurgical excision of an anal fissure involves exposing the altered scar tissue, including the fissure itself and painful areas around the anus, to high-frequency radio waves - about 3.8-4 MHz. The surrounding healthy tissue remains intact. But rough fibrous scars, a crack, a sentinel polyp - all this is evaporated by water under the influence of heat.
A radioknife is not a scalpel that sheds blood and damages healthy areas, which subsequently leads to the formation of a rough postoperative scar. It works cleanly, bloodlessly, contactlessly. No infection for you. Therefore, excision of the anal fissure with a radiofrequency scalpel is the optimal choice for both the modern surgeon and the modern patient.
Causes of anal fissure
An anal fissure can be caused by:
- defecation with very hard stools;
- anal sex;
- straining with constipation;
- inflammation in the anorectal region (the area of the anal sphincter and rectum), for example, proctitis.
To summarize, we can say that anal fissures occur either as a result of trauma to the anal canal (most often) or due to thinning of the mucosa.
Factors contributing to the formation of anal fissures are:
- sedentary lifestyle;
- staying in a sitting position for a long time (sedentary work);
- heavy physical work (weight lifting);
- poor nutrition. This is a common cause of constipation. For example, an insufficient amount of fluid consumed leads to excessive thickening of stool, and an insufficient amount of dietary fiber (fiber) slows down the passage of food through the gastrointestinal tract, as a result of which stool accumulates in the rectum;
- haemorrhoids.
During certain periods, the risk of anal fissures increases:
- in infancy (anal fissures are quite often observed in children aged 6 to 24 months. It is believed that the main reason for their formation is constipation);
- in old age (cause - impaired blood microcirculation in the anal area, constipation and intestinal dysfunction);
- during childbirth (due to pushing).
What is easier to cure – hemorrhoids or anal fissure?
The method of treating anal fissure, like the treatment of hemorrhoids, is determined in each specific case and depends on the severity of the pathology. Very often, an anal fissure occurs as a result of the development of hemorrhoids and then treatment must be comprehensive. Treatment of anal fissure is very different from the treatment of hemorrhoids: as a rule, to treat fissures at an early stage of development, non-surgical correction of the disease that has arisen is used, and only if therapy does not give the desired result, radical methods are used - surgical excision of the anal fissure. The most modern and painless method of excision today is radio wave surgery, thanks to which the pathology is eliminated.
Symptoms of anal fissure
First of all, the manifestations of an anal fissure are pain and bleeding.
Rupture of the mucous membrane leads to the fact that during defecation, the nerve endings of the muscle ring that holds back feces are irritated. As a result, a spasm of the anal sphincter occurs (this is the name of this muscle ring) - it increases pain, which can persist for a long time. Sphincter spasm also makes defecation difficult.
The symptoms of an anal fissure are largely the same as those of hemorrhoids. At the same time, hemorrhoids are a factor contributing to the formation of anal fissure, and quite often these two diseases occur simultaneously. Only a doctor can make an accurate diagnosis in a particular case.
Pain during bowel movements
Pain is felt primarily during bowel movements. In the case of an acute crack, there is usually no pain at rest.
With a significant size of the anal fissure, as well as if the rectal fissure has become chronic, the pain during defecation can be quite severe and even cause the so-called “fear of stools” - i.e. the desire to postpone bowel movement as long as possible, just to avoid experiencing unpleasant sensations.
Blood in stool
Blood may be found in stool or on toilet paper.
Itching in the anus
In the case of an acute fissure, patients may complain of itching in the anus at rest.
Chronic fissure and aloe treatment - how effective and safe is it?
The most popular traditional medicine recipes are based on the use of aloe. As you know, aloe has anti-inflammatory and healing properties and can alleviate the suffering of the patient and relieve the acute state of the disease. Rectal suppositories are made from it, pieces of the plant are applied to the sore spot, and a variety of local preparations are made based on the juice. Treatment of hemorrhoids in the initial stages of the disease in this way is quite possible and is periodically used as the first conservative stage in the treatment process. However, before treating anal fissures with traditional methods, you should remember that self-medication is fraught with extensive negative consequences.
Anal fissure treatment methods
Anal fissures require treatment. It is possible that a recently formed crack will disappear on its own, but there is a risk of the disease becoming chronic and it is quite high (10-15%). Besides, there is no point in putting up with pain and discomfort.
If an anal fissure is not treated, there is a possibility of a “vicious circle”. Pain during bowel movements causes bowel movements to be delayed, resulting in harder stool. Spasm of the anal sphincter makes defecation difficult; you have to push harder. All this leads to repeated injury to the mucous membrane and does not allow the crack to heal.
A timely visit to a doctor (immediately after detecting signs of crack formation) will allow you to avoid surgery and limit yourself to non-surgical and minimally invasive treatment methods. Getting rid of a fissure brings joy, because life with a fissure is filled with painful sensations and inconveniences, so much so that a person’s character may even change.
Qualified proctologists at the Family Doctor have the experience to choose the most effective course of treatment, and the modern equipment of the clinics allows operations and manipulations to be performed efficiently, quickly and in the most painless manner for the patient.
Conservative treatment
Acute anal fissure
treated conservatively. Treatment of rectal fissure is aimed primarily at normalizing stool (eliminating constipation or diarrhea). The patient is prescribed a diet that excludes spicy, salty and sour foods, as well as alcoholic drinks. The goal of drug treatment (suppositories, ointments) is to reduce pain, reduce sphincter spasm, and speed up healing.
Surgical treatment of anal fissure
For the treatment of chronic anal fissures
Minimally invasive surgical methods are used, and (if surgery is indicated) acute excision of the anal fissure is performed. The operation is performed under local anesthesia.
At the “Family Doctor”, surgical treatment of an anal fissure, depending on its nature, can be carried out using various methods: using a laser, using a radio wave scalpel (Surgitron radio wave surgery device), sharp excision of the fissure.
More information about the treatment method
Make an appointment Do not self-medicate. Contact our specialists who will correctly diagnose and prescribe treatment.
Rate how useful the material was
thank you for rating
What does a proctologist usually prescribe for a rectal fissure?
If this crack is fresh, acute, and no more than a month old, then the proctologist will prescribe a conservative treatment regimen. Of all the things that are suitable for anal fissures in order to normalize stool and reduce hypertonicity of the anal sphincter, the following important points can be highlighted:
- taking mild laxatives containing the prebiotic lactulose (a product of the processing of milk sugar - lactose), as well as herbal medicines (buckthorn bark, leaves of senna alexandria);
- diet therapy (more water, figs, dried apricots, raisins, beets, fermented milk products, fiber-rich whole grain products);
- if necessary, additional drug treatment (tablets, rectal ointments, creams, suppositories) can be prescribed. They will relieve inflammation, reduce sphincter spasm, and accelerate the repair (healing) of the anal fissure.
How does cauterization of an anal fissure occur?
Cauterization of an anal fissure is called electrocoagulation, and is performed with an infrared laser. Laser coagulation of cracks is modern and widely used, but it is quite painful and is not indicated in all cases. It is not suitable in the fight against chronic fissures, and is effective only for fresh ruptures of the rectum (for a period of 3, maximum 4 weeks).
It is much more painless and effective to undergo radiofrequency treatment , which, like laser treatment, is called cauterization.
The essence of cauterization is laser or radio wave excision of scar perianal tissue along with a crack. Occurs under local anesthesia.
DRUG TREATMENT OF HEMORRHOIDS AND ANAL fissure
L. Blagodarny, G. Vorobyov State Scientific Center for Coloproctology, Ministry of Health of the Russian Federation
Drug treatment of acute and chronic hemorrhoids, as well as anal fissure, is becoming increasingly important. This fact is associated with the highest frequency of these diseases in the practice of a surgeon and coloproctologist and with the appearance on the pharmaceutical market of quite effective analgesic, thrombolytic, hemostatic and phlebotonic drugs. The work of domestic and foreign scientists has established that hemorrhoids are based on the pathology of cavernous vascular formations formed during normal embryogenesis in the submucosal layer of the distal part of the rectum.
We came to the conclusion that, in addition to the vascular factor, the muscular dystrophic factor plays an important role in the pathogenesis of hemorrhoids. The first is based on vascular dysfunction, which promotes an increased influx of arterial blood into the cavernous bodies and a decrease in outflow through the cavernous veins, which leads to an increase in their size and the development of hemorrhoids. The second leading factor is dystrophic processes in the longitudinal muscle of the submucosal layer of the rectum and the ligament of Parks, which hold hemorrhoids in the anal canal. Under the influence of unfavorable factors, hemorrhoids enlarge, move distally, and ultimately fall out of the anal canal. Basically, these disorders occur in high-risk groups, which include people engaged in heavy physical labor, suffering from constipation, and sedentary occupations.
Hemorrhoids manifest themselves in two main syndromes: chronic and acute. These syndromes are like phases of the same process. Traditionally, hemorrhoids are characterized by two main symptoms: bleeding and prolapse of hemorrhoids. Note that the symptoms of colon diseases are quite monotonous and bleeding is a symptom not only of hemorrhoids, but of diseases such as malignant neoplasms, polyps, ulcerative colitis, and colon hemangioma. Prolapse of hemorrhoids most often should be differentiated from prolapse of the rectum, prolapse of a villous tumor. Therefore, to make a correct diagnosis, it is imperative to carry out not only an examination of the perianal area, but also a digital examination of the rectum and sigmoidoscopy.
The basis for the development of an acute process is thrombosis of hemorrhoids. The inflammatory process that develops in the node and surrounding tissues is most often its consequence. According to the clinical course, we divide acute hemorrhoids into three stages: 1. Thrombosis of hemorrhoids without an inflammatory process; 2. Thrombosis complicated by inflammation of hemorrhoids; 3. Thrombosis of hemorrhoids, complicated by inflammation of the subcutaneous tissue and perianal skin.
Indications for conservative treatment are the initial stages of chronic hemorrhoids and the acute course of the disease. This type of therapy consisted of general and local treatment. Of course, conservative treatment is indicated for acute hemorrhoids, but it should be noted that its prevention primarily consists of normalizing the activity of the digestive tract and treating constipation, which occurs in more than 75% of patients with hemorrhoids. We prescribe enzyme preparations, agents that affect the flora and peristalsis of the small and large intestines, hydrophilic colloids, or, as they are also called, dietary fiber, against the background of regular and sufficient fluid intake. Wheat bran, seaweed and flaxseed in their natural form or in the form of pharmacological preparations are traditionally used as their source in our country. Abroad, psyllium seeds and husks and flaxseed are more often used in the form of preparations such as agiolax, fiberlax, nutriclinz, etc., which have a high water-holding capacity. It is not our task to analyze drug therapy for irritable bowel syndrome. However, regulation of the consistency of intestinal contents and its transit through the colon is an indispensable condition not only for the prevention, but also for the successful treatment of hemorrhoids.
Local treatment is aimed at eliminating pain, thrombosis or inflammation of hemorrhoids, as well as bleeding. When choosing local treatment for acute hemorrhoids, it is necessary to take into account the prevalence of one of the symptoms - pain, thrombosis, the prevalence of the inflammatory process and the presence of a destructive component. In case of bleeding, the amount of blood loss, its activity and the severity of posthemorrhagic anemia should be clearly assessed.
Pain syndrome with hemorrhoids is often associated with strangulation of a thrombosed hemorrhoid or the occurrence of an acute anal fissure. Most often, the mechanism of its formation is a spasm of the anal sphincter associated with the inflammatory process in the hemorrhoidal node. Therefore, to eliminate pain, the use of non-narcotic analgesics and local combined painkillers is indicated. For local treatment of hemorrhoids, we use drugs such as aurobin, ultraproct, proctoglivenol, etc. From this group, the new drug nefluan, containing a high concentration of lidocaine and neomycin, stands out for its effectiveness.
Thrombosis of hemorrhoids, complicated by their inflammation, is an indication for the use of combination drugs containing analgesic, thrombolytic and anti-inflammatory components. This group of drugs includes proctosedyl and hepatrombin G, produced in the form of ointment, gel bases and suppositories. The pharmacokinetics of the latter drug is that heparin and allantoin, by binding plasma coagulation factors and having an inhibitory effect on hemostasis, cause a thrombolytic effect, panthenol stimulates metabolic processes, granulation and epithelization of tissue, and polydecanol has an analgesic effect. The preference for using hepatrombin G is that it has a pronounced thrombolytic and anti-inflammatory effect and does not contain glucocorticoids. The use of this drug in 30 people for seven days showed its high effectiveness, rapid subsidence of pain in 87% of treated patients, reduction of thrombosis and inflammatory processes in 91%.
Thrombosis of hemorrhoids is an indication for the use of local anticoagulants. This group of drugs includes heparin and troxevasin ointments, hepatrombin G. In 70-80% of cases, thrombosis of hemorrhoids is complicated by their inflammation with transition to the subcutaneous tissue and perianal area. For inflammation of hemorrhoids and surrounding tissues, the above drugs are used in combination with water-soluble ointments that have a powerful anti-inflammatory effect. These include levosin, levomekol, mafinide.
Bleeding is one of the main symptoms of hemorrhoids. Continuous bleeding for one hour is a sign of an acute process, and suppositories containing adrenaline can be used to eliminate it. In addition, local hemostatic materials such as adroxon, beriplast, tachycomb, spongostan, consisting of fibrinogen and thrombin, are used. When introduced into the anal canal, they dissolve, forming a fibrin film, and block the bleeding areas of the hemorrhoids.
The basis of general treatment was the use of phlebotropic drugs, which cause an increase in the tone of the veins, improvement of microcirculation in the cavernous bodies and normalization of blood flow in them. This group includes drugs such as troxevasin, venoruton, glivenol, cyclo 3 Fort. In our opinion, as in the opinion of many phlebologists, the most effective in this group is Detralex 500. In one of our studies, treatment with this drug was carried out in 120 patients with acute hemorrhoids. In the main group (60 people), patients took Detralex, and in the control group, placebo. Compared with the group of patients taking placebo, pain in the main group decreased in 83% of cases, prolapse of nodes in 81%, and bleeding of hemorrhoids in 91%. In the same group, there was an almost two-fold decrease in the frequency and quantity of taking non-narcotic analgesics. In 98% of treated patients, after such treatment, inflammatory phenomena subsided, and the frequency of annual exacerbations decreased by 2.2 times. Treatment with phlebotropic drugs can more than halve the duration of exacerbations and reduce the average severity of exacerbations by 1.5 times. As a maintenance treatment, conservative therapy is carried out with widespread minimally invasive treatment methods, used mainly in outpatient settings and during surgical interventions, which are indicated in the later stages of hemorrhoids.
In conclusion of this section, it should be noted that, despite the use of modern effective drugs, conservative treatment, carried out mainly in the acute phase of the disease, is only a palliative measure and gives only a temporary positive effect. Resumption of constipation, errors in diet, and increased physical activity lead to another exacerbation, which requires repeated conservative treatment. Therefore, if this type of treatment is ineffective, especially in the later stages of the disease, combined treatment should be carried out, including conservative and minimally invasive methods or conservative and surgical methods of treatment.
Let us note that if conservative treatment of acute and chronic hemorrhoids can be carried out by general practitioners, then minimally invasive methods should be performed only by a coloproctologist on an outpatient basis or, if indicated, in an inpatient setting. Surgical intervention - hemorrhoidectomy - should be performed in specialized hospitals.
Thus, the choice of a treatment method for hemorrhoids depending on its stage and severity of symptoms, the use of drug treatment, minimally invasive methods, both independently and in combination with conservative treatment or surgical methods, allow achieving good results in 99% of patients.
Anal fissure is a spontaneously occurring linear or elliptical defect (ulcer) of the mucous membrane of the anal canal. The incidence of anal fissure, judging by the number of patients, ranges from 11 to 15% among diseases of the colon and is 20-23 cases per 1000 adults. Young and middle-aged women are more often affected.
The causes of anal fissure are numerous. Among them, the most likely are considered: mechanical, vascular disorders, changes in the perianal epithelium (parakeratosis), neuromuscular changes in the anal sphincter. This area of the anal canal also has anatomical prerequisites for the formation of cracks. Firstly, the deeper distal parts of the anal sinuses (crypts) are located here. Secondly, the tendon endings of the anal sphincter muscles converge on the posterior wall of the anal canal. In women, the weak point of the anal canal is its anterior part, where the vulva, vagina and fibrous center of the perineum seem to converge. Therefore, a fissure in the anterior part of the anal canal occurs mainly in women. Cracks on the side walls of the anal canal are relatively rare.
The formation of a fissure is also associated with vascular changes in the anal canal. The fissure is often combined with hemorrhoids. The medial walls of the internal hemorrhoids are essentially the walls of the anus. They are located in the area of the anorectal line, which is most susceptible to injury during defecation. In addition, circulatory disorders (blood stagnation, thrombosis) in this area, especially in the posterior and anterior parts of the anal canal, may be accompanied by the formation of linear ulcers, similar in nature to varicose ulcers, which explains the chronic course of many anal fissures with hemorrhoids. Thus, anal fissure is a polyetiological disease, which must be taken into account in the process of its treatment.
The area of the mucous membrane in these areas, exposed to highly virulent rectal flora, becomes scarified, and then thickens, deepens, and thus a real crack is formed - a longitudinal defect of the mucous membrane with clear edges and a bottom. In a chronic course, the edges of such an ulcer become denser and thicker, especially in the distal part of the fissure, where a polypoid, connective tissue thickening is formed - a “sentinel tubercle”, and in the proximal part, i.e. at the level of the dentate line itself, a hyperplastic anal papilla is sometimes detected. Anal papillae are normally thickened distal parts of the valves of the anal columns and have no relation to true polyps of the anal canal. This was clearly shown by V.A. Amineva (1972), but still many surgeons in such cases diagnose an anal polyp, which leads not so much to incorrect actions by the doctor, but to misinformation of patients that is unjustified from the standpoint of deontology.
The clinical picture of an anal fissure consists of a triad - pain in the anus, spasm of the anal sphincter, bleeding from the anus. This is so typical and so clearly revealed during the first interview of the patient that in typical cases the diagnosis is clear even before the examination. If the fissure is combined with hemorrhoids, then prolapse of nodes and more profuse rectal bleeding are usually added to these complaints. Pain that intensifies during defecation, in turn, causes a spasm of the muscular structures of the anal sphincter, and the spasm only intensifies the pain. These two symptoms - pain and spasm - constitute the most important elements of the well-known clinical triad of anal fissure. Its third component is bleeding from the anal canal. These relatively minor hemorrhages during or immediately after defecation are explained simply by injury to the walls of the fissure by dense feces (especially with constipation).
With acute fissures, the pain is usually strong, constant, but relatively short-lived - only during bowel movements and for 15-20 minutes after it. Sphincter spasm in such patients is usually pronounced, and bleeding is usually minimal. With an acute fissure, usually only a painful area is detected on the wall of the anal canal (most often, we repeat, on the posterior wall), and seals, raised edges of the fissure, and a “guard tubercle” at its distal edge may not be detected. With a chronic fissure, the pain is longer lasting and intensifies not only after stool, but also with prolonged forced positioning. Patients develop a symptom such as “fear of stools.” Patients increasingly begin to resort to various laxatives, enemas, become irritable, and experience insomnia.
Complications of an anal fissure are most often acute paraproctitis, which develops as a result of infection entering the pararectal tissue through a defect in the mucous membrane of the anal canal.
The most typical clinical signs of anal sphincter spasm are prolonged intense pain that occurs after defecation, difficulty defecating, and a sharp increase in the anal reflex. With an anal fissure, the main changes in the function of the obturator apparatus of the rectum are reduced to a spasm of the internal sphincter. At the same time, no spasm is observed on the part of the external sphincter, which is confirmed by functional studies.
Differential diagnosis of anal fissure is relatively simple. The fissure must first of all be differentiated from incomplete internal fistulas of the rectum. In the chronic course of the disease, the fissure is often accompanied by anal itching, proctitis (sphincteritis) or proctosigmoiditis.
When diagnosing an anal fissure, you need to be sure that this is an ordinary, “banal” fissure, and not a manifestation of syphilis (gumma), rectal tuberculosis, some rare parasitic (actinomycosis) or other disease, for example, anal fissure in Crohn's disease. What helps here is mainly a careful collection of anamnesis, because according to the clinical picture, a “usual” anal fissure can occur in different ways and it can be very difficult to distinguish it from a specific lesion only with the help of digital examination or anoscopy (rectoscopy). It is also necessary to remember about possible anal manifestations of acquired immunodeficiency syndrome (AIDS).
When starting treatment for patients with anal fissure, you should make it a rule to begin treatment with conservative measures. Treatment of acute (or recurrent chronic) fissure begins with normalization of stool. Just as with hemorrhoids, in many cases, only regulating the transit of intestinal contents through the colon, changing its consistency during constipation with the help of hydrophilic colloids and nutritional supplements, or curing chronic diarrhea, most often associated with dysbacteriosis, especially with acute postpartum fissure, gives lasting effect. Of course, for the period of treatment, the course of which lasts on average two weeks, salty, sour foods and alcoholic drinks are excluded from food. Currently, many patented suppositories are produced (ultraproct, proctoglivenol, hepatrombin, drug N), and patients, using them independently, find the most suitable ones themselves. If we are talking about any analgesic and sanitizing ointment produced in bottles, then screw a special tip onto the bottle and squeeze out an example of 1 cm of ointment into the anal canal. After stool, before inserting the suppository, a warm (36-38°C) sitz bath should be prescribed. The same manipulation is performed at night. No antibiotics are prescribed.
Foreign scientists have proven the possibility of eliminating spasm of the anal sphincter with the help of drugs containing nitroglycerin. Drugs such as nitrolingval, isomac spray, isoket and nitroglycerin ointment are used. However, the use of these drugs is limited due to their pronounced vasodilating effects and side effects such as headache and weakness. The described course of treatment, as a rule, leads to significant improvement: the intensity of pain decreases, sphincter spasm decreases. Under all conditions, such a first course of treatment is very important prognostically: its ineffectiveness within 12-15 days is an indication for surgery. Surgical treatment of anal fissures must be carried out in case of chronic disease that is not amenable to conservative therapy.
Conservative treatment and surgical intervention, carried out taking into account the functional state of the obturator apparatus of the rectum, established on the basis of a clinical and functional examination, ensure recovery in 98-100% of treated patients
Source: “Pharmaceutical Bulletin” (www.pharmvestnik.ru)