Pregnancy brings many changes to the functioning of a woman's organs, and the heart is no exception. In most cases, the pain that occurs in it is not dangerous and is associated precisely with the restructuring of the body caused by an increase in the weight of the uterus and placenta, increased nervous and emotional excitability of the expectant mother, changes in blood circulation and oxygen starvation of the myocardium. Only sometimes pain in the heart signals possible pathologies that the woman did not know about before pregnancy.
In our article we will talk about cases that may be a reason to contact a cardiologist, and those situations when heart pain is only a temporary and self-limiting phenomenon. This knowledge will help you suspect pathology if it is already present, and will reassure you if an episode of harmless pain worries you.
Disorders of the cardiovascular system in pregnant women
With an increase in atrial and ventricular parameters in a healthy heart, ventricular function is preserved. Meanwhile, in patients with heart disease, adaptation of the left and right ventricles during pregnancy may be insufficient.
Also, at present, pregnant women experience peripheral vasodilation and a decrease in systemic and pulmonary vascular resistance.
At the end of pregnancy, due to the strong enlargement of the uterus in the supine position, compression of the inferior vena cava occurs, which can reduce the flow of venous blood, changing the systolic and cardiac output.
It is important to note that pregnancy is a hypercoagulable state that increases the risk of thromboembolic complications.
In modern society, as methods of treating congenital heart defects improve and the age of pregnant women increases, more and more often pregnant women with arterial hypertension (AH) and coronary heart disease undergo corrective operations on the heart or valve.
It is important to know the risks of cardiovascular disease for the mother and fetus, since treatment can affect not only the health of the mother, but also the health of the child. The article discusses the main cardiovascular diseases of pregnant women and methods of their optimal treatment.
Features of treatment
Treatment for heart pain is selected depending on the diagnosis. Diagnosis is carried out by a cardiologist or neurologist if we are talking about intercostal neuralgia. As a rule, the diagnosis is made on the basis of a cardiogram and ultrasound of the heart.
Self-medication while carrying a child is prohibited. The most harmless medications that a woman took before pregnancy can negatively affect the fetus. What should a pregnant woman do if her heart hurts? During an attack, the expectant mother should take a semi-lying position, empty her chest, unfasten the buttons, and provide access to fresh air. If the pain continues, you need to call an ambulance.
Hypertensive diseases and their treatment during pregnancy
The most common health problems during pregnancy are hypertension, which affects up to 5-10% of pregnant women in the world. Such problems are associated with increased maternal, fetal and neonatal morbidity and mortality.
Maternal hypertension is associated with an increased risk of:
- development of placental abruption;
- stroke;
- organ dysfunction;
- disseminated intravascular coagulation.
Development of placental abruption
And fetal growth retardation, premature birth and intrauterine fetal death are also possible.
Increased blood pressure (EQS) is measured in the outpatient or inpatient setting (sAKS ≥140 mmHg and/or dAKS ≥90 mmHg), but the classification of hypertension (AH) in pregnant women differs from that in the rest of the population. Moderate increase in EQS is 140–159 / 90–109 mmHg. Art., and high-grade hypertension is defined as EQS ≥160/110 mmHg. Art.
It is important to emphasize that EQS during pregnancy should be measured in sedentary patients using a mechanical sphygmomanometer, as automated EQS meters are unreliable in severe preeclampsia.
Additional tests—complete blood count, urinalysis, uremic tests, liver function tests—are important for all patients who develop elevated EQS during pregnancy.
To determine preeclampsia, it is necessary to evaluate the level of proteinuria and the albumin/creatinine ratio. In selected cases of suspected rare diseases causing hypertension, ultrasound examination of the adrenal glands, renal blood vessels and urinalysis for metanephrine should be considered.
What examinations need to be completed
Each expectant mother is registered with the antenatal clinic for observation and periodic examinations. It is advisable to do this during the first trimester (up to 12 weeks). Women who have heart pain during pregnancy are at risk and require closer monitoring.
If attacks worsen or become more frequent, it is recommended to seek advice from a therapist or cardiologist. It may be necessary to conduct a number of laboratory and instrumental studies:
- electrocardiography;
- echocardiography (ultrasound of the heart);
- general blood analysis;
- clinical urine analysis;
- blood chemistry;
- hormonal indicators;
- genetic tests.
These procedures are informative and safe for the woman and fetus.
Classification of hypertension in pregnant women
According to the recommendations of the European Society of Cardiology (ECD), hypertension during pregnancy is divided into:
- chronic (primary or secondary);
- pathologies of pregnant women;
- chronic complicated preeclampsia;
- unclassified hypertension;
- preeclampsia.
The main risk factors for hypertension and preeclampsia are:
- observed increase in EQS in previous pregnancies;
- chronic kidney disease;
- autoimmune diseases (systemic lupus erythematosus, antiphospholipid syndrome);
- diabetes mellitus type 1 or 2;
- late pregnancy (> 40 years);
- increase in BMI (> 35 kg/m2);
- multiple pregnancy;
- family history of preeclampsia.
Late pregnancy
Treatment of arterial hypertension during pregnancy
Treatment of hypertension during pregnancy depends on the increase in EQS, duration of pregnancy, and risk factors for the mother and fetus. Non-pharmacological treatment alone does not have a significant effect on the reduction of EQS in pregnancy outcomes, but changes in diet and lifestyle (maintenance of physical activity, low weight gain in pregnant women with obesity ≤6.8 kg) are recommended in combination with medications.
Drug treatment is recommended for all women with EQS ≥150/95 mmHg. Art. or at > 140/90 mm Hg. Art., for gestational hypertension, previously diagnosed hypertension with observed worsening during pregnancy or with signs of end-organ damage.
- Typically used to treat pregnant women: methyldop, beta-blockers (BAB, labetolol), calcium channel blockers (CCB, nifedipine). BBs are less effective than CCBs and can cause fetal bradycardia, growth retardation, and hypoglycemia, so it is important to choose the right dose.
- ACEs, ARBs, and direct renin inhibitors are contraindicated for the treatment of ACS during pregnancy. During preeclampsia, there is a decrease in plasma volume, so diuretics should be avoided.
- In case of a significant increase in EQS (≥170/110 mmHg), further inpatient treatment is recommended.
Drug treatment of arterial hypertension during pregnancy
The choice of medication depends on the planned end of pregnancy. Treatment usually begins with intravenous labetolol, methyldopa, or oral nifedipine. Hydralazine and sodium nitroprusside are not recommended for possible side effects in the fetus. For preeclampsia and pulmonary edema, treatment with intravenous nitroglycerin is recommended. The main recommendations for the treatment of hypertension according to ECD are presented in Table 1.
Table 1. Recommendations for the treatment of hypertension ECT during pregnancy
| Recommendation | Class | Level |
| Low-dose aspirin (100–150 mg) is recommended for patients at moderate to high risk of preeclampsia from 12 to 36 and 37 weeks of pregnancy. | I | A |
| In the case of gestational hypertension, previously diagnosed hypertension, exacerbation of pregnancy, or detection of end-organ damage, it is recommended to initiate medication when EQS > 140/90 mmHg. In all other cases, with EQS ≥150/95 mmHg. | I | C |
| SAKS ≥170 mmHg Art. Or dAKS ≥110 mmHg. Art. In pregnant women, this is a situation that requires urgent action, so hospitalization of patients is recommended. | I | C |
| Methyldopa (B), labetalol (C), KKB (C) are recommended drugs during pregnancy. | I | B (methyldopa) |
| C (labetolol and KKB) | ||
| In women with hypertension or preeclampsia, delivery is recommended at 37 weeks of pregnancy. | I | B |
| Early birth is recommended in the presence of preeclampsia and other disorders (vision, hemostasis). | I | C |
| Intravenous nitroglycerin is recommended for the treatment of preeclampsia and pulmonary edema. | I | C |
| For severe hypertension, treatment with labetolol, oral methyldopa, or nifedipine is recommended. | I | C |
| In obese pregnant women (BMI >30 kg/m2), a weight gain limit of <6.8 kg should be considered. | IIa | C |
| ACE inhibitors, ARBs, and direct renin inhibitors are contraindicated. | III | C |
Recommendations for the second trimester of pregnancy
Most recommendations are universal for all trimesters, for example, giving up bad habits, sleeping for 8-9 hours and eating well. But there are some important tips that apply specifically to the second trimester.
- You should only sleep on your side and use a special pillow for pregnant women.
- From the 24th week, it is advisable to start wearing a bandage, this will help reduce the load on the spinal column.
- Avoid contact with people who are sick or have a cold. If the second trimester falls during the “cold season,” try to spend less time in crowded places.
- Take vitamin and mineral supplements, even if you haven't done so before. Right now, the need for vitamins and minerals is increasing somewhat, especially iron, as well as omega-3 PUFAs, which are needed for the formation and proper development of the child’s brain, nervous and immune systems.
- Switch to proper nutrition. The second trimester is a time of active fetal growth; diets and fasting are inappropriate now. But it is important not to get carried away with fast food, to make sure that the menu has enough proteins and seasonal vegetables and fruits.
Treatment of coronary heart disease during pregnancy
The incidence of acute coronary syndromes (ACS) in pregnant women is low, but coronary heart disease is associated with more than 20% of cardiovascular deaths in pregnant women.
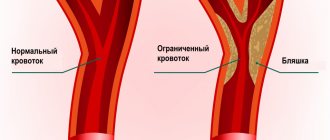
The etiology of coronary heart disease in pregnant women differs from the rest of the population. In most cases, it is not atherosclerotic coronary artery disease that predominates, but spontaneous coronary artery dissection associated with pregnancy, thrombosis, or cardiac damage in the absence of coronary artery disease.
Spontaneous coronary artery dissection may be associated with fluctuations in estrogen/progesterone levels, which cause structural changes in the coronary arteries, increasing vasodilation during labor. Thrombosis is usually caused by a hypercoagulable state. Paroxysmal embolization is possible.
Most ACS occur in the 3rd trimester or after childbirth. The ECG is more difficult to assess because T wave inversion can occur during pregnancy even in the absence of myocardial ischemia, and elevated serum troponin levels should be considered a marker of myocardial damage even when preeclampsia is diagnosed.
Recommendations for the treatment of ACEs in pregnant women are similar to those for the rest of the population. However, it is important to emphasize that in hemodynamically stable, low-risk patients with non-ST segment elevation acute myocardial infarction (AMI), a conservative treatment strategy may be considered.
Meanwhile, for patients requiring interventional treatment, it is important to reduce the dose of ionizing radiation they receive during interventional radiological procedures. From a treatment point of view, pregnancy is a condition with an increased risk of bleeding, so high activity P2Y12 inhibitors (ticagrelor) should be used with caution, and there is no information on the use of glycoprotein IIb/IIIa inhibitors (abciximab, tirofiban). Therefore, treatment with a combination of aspirin and clopidogrel with the shortest duration of clopidogrel administration is currently recommended.
Nature of pain
Sharp, pressing pain on the left side of the sternum is called ischemic. They radiate to the left arm or shoulder blade. They appear in pregnant women in the first trimester, when the circulatory system is adapting, or after excessive physical and nervous stress.
Doctors call diffuse, aching pain in the sternum cardialgia. They get worse when coughing and taking deep breaths. Such sensations should alert the expectant mother, because they indicate the presence of inflammatory processes or defects.
Heart valve disease and its treatment during pregnancy
Heart valve disease in patients of reproductive age is more common in developing countries where the incidence of rheumatic fever is still high. Another important problem for pregnant women is the need for mechanical prostheses and anticoagulants. In the case of stenotic heart defects, increased cardiac output causes an increase in the transverse gradient of up to 50%, which increases the risk of complications for the fetus and mother.
Heart valve diseases
Although mitral stenosis is well tolerated, approximately one third of patients with a valve opening area of less than 1 cm2 experience symptoms and signs of heart failure during pregnancy.
Drug treatment is recommended in the presence of severe symptoms or clinically significant pulmonary hypertension. Treatment with selective BAC (metoprolol, bisoprolol), diuretics in low doses is recommended; for paroxysmal or persistent atrial fibrillation (PV), left atrial thrombosis (BP), previous thromboembolism, unfractionated heparin (NFH), low molecular weight heparins (MMMH) or vitamin K antagonists (VKA).
Anticoagulants should also be considered in patients with sinus rhythm but severe mitral stenosis, spontaneous enhancement, severe cardiac dilatation, or congestive heart failure (CHF).
Pregnancy is not recommended for all patients with severe mitral stenosis, and interventions should be performed prior to this.
Regarding aortic valve stenosis (AoV), exacerbation and mortality during pregnancy depend on the severity and symptoms of aortic stenosis. Heart failure occurs in 10% of patients with moderate AoV stenosis who were asymptomatic before pregnancy.
In symptomatic patients, heart failure during pregnancy may be as high as 25%. Although pregnancy is well tolerated, mortality and severe complications in the mother are rare, but about 20-25%. cases are associated with fetal growth retardation, premature birth, and low birth weight.
If symptoms of heart failure develop, drug treatment is used. If signs of congestive heart failure are present, diuretics may be prescribed.
As with mitral stenosis, patients with severe AoV stenosis and impaired LV function should be advised to avoid pregnancy.
Regurgitant heart valve disease may be associated with rheumatism, degenerative or congenital lesions. Patients who have severe valve leak and symptoms or LV dysfunction are at high risk of developing heart failure. According to the literature, 20-25% of patients diagnosed with moderate or severe mitral valve regurgitation (MVN) of rheumatic origin develop heart failure during pregnancy.
Acute severe valve leaks are poorly tolerated by pregnant women. It is important to note that some patients experience a persistent increase in valve leakage during pregnancy. Medicines are needed to reduce excess fluid in the body.
Although interventional treatment is recommended before pregnancy, in the presence of acute severe valve leak with signs of heart failure that cannot be controlled with medications, surgery is also performed during pregnancy.
It is important to emphasize that in the presence of a sufficiently mature fetus, termination of pregnancy is first recommended, and then cardiac surgery is offered.
For women of childbearing age planning pregnancy and suffering from heart valve disease, the issue of valve selection is important. Although mechanical valves have excellent hemodynamic properties and are durable, their implantation is associated with prolonged use of anticoagulants, increased pregnancy and fetal morbidity, and mortality.
The risk of complications (thromboembolism, bleeding, miscarriage, premature birth) during pregnancy with a mechanical valve and the use of anticoagulants is high. VKA use is associated with a risk of embryopathy in the 1st trimester, which depends on the dose of VKA. Meanwhile, the risk of complications with an implanted bioprosthesis with good function and without LV dysfunction is minimal.
However, bioprostheses are not as durable and are associated with a higher risk of structural damage to the valve. With severe dysfunction of the bioprosthesis, the risk of complications increases. In this case, patients are more likely to require repeat surgery during pregnancy. Thus, the decision to choose a valve for a woman of childbearing age should be made by a team of cardiologists together with the patient, taking into account all the disadvantages and advantages of the valves.
The issue of prescribing anticoagulants should be discussed with all women planning pregnancy and having an implanted mechanical heart valve.
Mechanical heart valve
It is important to emphasize that VKAs are the most suitable and effective option for the prevention of valve thrombosis in pregnant women, but they pose a danger to the fetus (embiopathy, fetopathy). MMMH, which do not cross the placental barrier, are less harmful to the fetus but are associated with a higher risk of valve thrombosis.
Another important aspect is extremely strict adherence to medication regimen. EKD recommends continuing VKA until conception. Their continuation may be considered during pregnancy if a low dose of VKA is required to achieve the target INR. When VKA is used during pregnancy, it is recommended to check the INR every 1-2 weeks. When administering MMMH 2 times/day, adjust the dose accordingly based on anti-factor Xa levels prior to administration.
What should you avoid in mid-pregnancy?
In the second trimester of pregnancy, the characteristics of a woman’s condition suggest some restrictions and more careful behavior in everyday matters.
- Do not take medications without a doctor's prescription.
- Do not wear tight, constricting clothing.
- Never lift more than 3 kg.
- If you are involved in strength or team sports, you will have to give up training. You can move on to more gentle and relaxing activities, such as swimming, Pilates, etc.
It is in the second trimester that a woman gets used to her new role, “gets to know” the baby when he moves, and becomes attached to him. This is a period of bright feelings and genuine emotions. Do everything in your power to ensure that your future baby develops correctly and is born healthy!
THIS IS NOT AN ADVERTISING. THE MATERIAL WAS PREPARED WITH THE PARTICIPATION OF EXPERTS.
conclusions
In modern society, thanks to improved treatment of congenital heart defects and patient survival, as well as an increase in the incidence of coronary and hypertensive heart disease, pregnant women with various cardiovascular diseases are becoming increasingly vulnerable.
This group of patients is exceptional. To choose the optimal treatment strategy, it is necessary to assess the risk not only for the pregnant woman, but also for the fetus. Therefore, it is important to carefully evaluate the situation on a case-by-case basis. Not only specialists in various fields (obstetrician-gynecologist, cardiac surgeon, neonatologist, etc.), but also the patient should take part in making decisions about treatment.
External factors of pain
The state of pregnancy makes a woman's body more susceptible to many environmental factors. Which of them can lead to painful sensations in the heart area? Most often this is:
- sudden changes in weather conditions;
- prolonged stay in an uncomfortable position;
- stressful situation;
- screams, noise, loud music;
- overwork;
- staying in a room with a large number of people, as well as in poorly ventilated areas.
Most often, these are the reasons that cause cardiac complaints. In such situations, eliminating the trigger factor leads to a gradual decrease in symptoms. That is, if a woman is in a stuffy room, it is necessary to ensure an influx of fresh air and this will certainly have a beneficial effect on the well-being of the pregnant woman.
Sources
- Lindheimer, M.D., S.J., Cunningham, F.G. ASH Position Paper: Hypertension in Pregnancy. J Clin Hypertens (Greenwich) 2009;
- Shade JH Jr, Ross J, Bever FN, et al. Troponin I in the diagnosis of acute myocardial infarction during pregnancy, labor and the puerperium. Am J Obstet Gynecol 2002;
- Kampman MA, Valente MA, van Melle JP, et al: Cardiac adaptation during pregnancy in women with congenital heart disease and healthy women. Heart 2016;
- Cornett J, Ruiz TP, Rossi A, et al. Hemodynamic adaptation to pregnancy in women with structural heart disease. Int J Cardiol 2013;
- Farr A, Einig S, et al. Outcomes and trends in postpartum maternal intensive care unit admission. Wien Klin Wochenschr 2017;
- Villar J, Carroli J, Wojdyla D, et al. Preeclampsia, gestational hypertension and intrauterine growth restriction, related or independent conditions? Am J Obstet Gynecol 2006;
- Elkayam U., Goland S., Pieper P.G., Silverside S.K. High-risk heart disease during pregnancy: Part i. J Am Coll Cardiol 2016;.
- Horvat S., Diller G.P., van Hagen I.M. et al. Risk of pregnancy in moderate and severe aortic stenosis: From the international ROPAC registry. J Am Coll Cardiol 2016;
- American College of Obstetricians and Gynecologists; Task Force on Hypertension in Pregnancy. Hypertension during pregnancy. Report of the American College of Obstetricians and Gynecologists' Task Force on Hypertension in Pregnancy. Obstet Gynecol 2013;
- Magee LA, Cham S, Waterman EJ. et al. Hydralazine for the treatment of severe hypertension in pregnant women: a meta-analysis. BMJ 2003;
- Elkayam U., Jalnapurkar S., Barakkat M.N. et al. Acute myocardial infarction associated with pregnancy: a review of contemporary experience in 150 cases between 2006 and 2011. Circulation 2014;
- Shekhar S, Gupta N, Kirubakaran R, Pareek P. Oral nifedipine versus intravenous labetalol for severe hypertension during pregnancy: a systematic review and meta-analysis. BKAD 2016;
- Goland S., Elkayam U. Anticoagulant therapy during pregnancy. Cardiol Clin 2012;
- Van Hagen IM, Thorne SA, Taha N, et al. ROPAC Investigators and EORP Team. Pregnancy outcomes in women with rheumatic mitral valve disease: Results from the Pregnancy and Heart Disease Registry. Circulation 2018;
- Sillesen M, Hjortdal V, Veilstrup N, Sørensen K. Pregnancy with prosthetic heart valves - 30 years of nationwide experience in Denmark. Eur J Cardiothorac Surg 2011.
MAKE AN APPOINTMENT
[contact-form-7 id=”296" title=”Untitled”]
Abortion and contraception clinic in St. Petersburg - department of the medical gynecological association "Diana"
Make an appointment, tests or ultrasound via the contact form or by calling +8 (812) 62-962-77. We work seven days a week from 09:00 to 21:00.
We are located in the Krasnogvardeisky district, next to the Novocherkasskaya, Ploshchad Alexander Nevsky and Ladozhskaya metro stations.
The cost of a medical abortion in our clinic is 3,300 rubles. The price includes all pills, an examination by a gynecologist and an ultrasound to determine the timing of pregnancy.
Why does your heart hurt in early pregnancy?
In most cases, unpleasant symptoms in the expectant mother arise due to her delicate position and are not associated with any specific pathology. So, in the first weeks of pregnancy, a woman may feel unwell due to serious hormonal changes in the body. During this period, the blood is sharply enriched with progesterone, estrogens, human chorionic gonadotropin and other specific substances.
A woman’s cardiovascular and respiratory systems begin to systematically adapt to the needs of the growing fetus. The tone of the autonomic system also changes: neuralgic conditions develop, as a result of which the expectant mother may feel pain in the heart. The same reason is associated with the appearance of drowsiness, high irritability and dizziness. Typically, a pregnant woman’s mood and well-being level off with the onset of the second trimester.