Among diseases of the biliary tract, the first place belongs to dyskinetic disorders.
Dysfunctions of the biliary tract (previously called dyskinesias) mean disturbances in the motor-evacuation function of the gallbladder, ducts, as well as disturbances in the tone of the sphincter of Oddi. These changes lead to disruption of the process of formation and secretion of bile, and subsequently to its stagnation. Biliary tract dysfunctions are functional disorders lasting more than 3 months. They can be periodic, short-term or protracted, manifesting themselves in the form of pain in the right hypochondrium.
Bile plays an important role in the digestion process. It is needed to “blur” fats into an emulsion. It is then processed by enzymes in the intestines, broken down and absorbed. Bile is an aqueous solution consisting of 70% bile salts (cholic and chenodioxycholic), 22% phospholipids (lecithin), 4% cholesterol, 3% protein and 0.3% from bilirubin. With insufficient amounts of bile acids - lecithin and cholesterol - insoluble cholesterol appears and bile becomes lithogenic. When stagnation occurs in the biliary tract, changes in the composition of bile occur, an inflammatory process develops and a sediment appears in the bile - biliary sludge, which can subsequently lead to the formation of stones.
Causes of biliary tract dysfunction
Primary biliary dyskinesia can occur in children due to: uncoordinated work of the sympathetic and parasympathetic nervous systems: the tone of the sphincter of Oddi and the gallbladder decreases.
Also, various stresses, improper diet or eating errors (eating large amounts of fatty foods, overeating or irregular meals) lead to the fact that the neuromuscular apparatus of the gallbladder becomes irritated and contracts poorly. Secondary dyskinesia of the biliary tract appears due to: chronic diseases of the digestive system, helminthic infestation; congenital malformations of the biliary tract; endocrine disorders, inflammatory diseases of the digestive system.
Why does the disease occur?
It is customary to identify a number of reasons that provoke the development of bleeding (portal hypertension) from varicose veins. The presence of several varicose veins leads to disruption of the closure function of the cardiac sphincter. As a consequence, so-called reflux esophagitis is observed, which as a result causes thinning and atrophy of the esophageal mucosa, as well as the appearance of erosions. With a significant increase in portal pressure, varicose veins rupture in the area of damaged esophageal mucosa, which is accompanied by severe esophagogastric bleeding. A serious danger of such bleeding cannot be excluded due to the possibility of injury to the superficially located veins of the mucous and submucosal layers of the esophagus, which have a superficial location, as well as the cardia of the stomach when eating rough food. In addition, it is quite possible to provoke a rupture of the varicose veins by exhibiting increased physical activity. You should know that peptic ulcer disease in this case is another serious risk factor.
Symptoms of biliary tract dysfunction
Clinical manifestations of dysfunctional disorders of the biliary tract are quite wide and can be nonspecific. Complaints are multisymptomatic and usually associated with psychosocial factors. They can be roughly divided into three groups.
Abdominal pain
The hypertensive form of gallbladder dysfunction is characterized by acute paroxysmal, stabbing, short-term compressive pain in the right hypochondrium or around the navel, usually accompanied by nausea, belching or even vomiting, but without a rise in temperature.
The hypotonic form is characterized by aching, pressing, dull pain that becomes constant and is associated with eating, physical activity or emotional stress. There is a bitterness in the mouth and nausea.
Spasm of the sphincter of Oddi in combination with decreased tone of the gallbladder is characterized by dull, aching pain in the abdomen. With insufficiency of the sphincter of Oddi, early pain is characteristic after eating fatty foods; they can be sharp and aching, combined with manifestations of dyspepsia.
Dyspeptic disorders
Nausea, vomiting, belching, heartburn, bitterness in the mouth, a feeling of heaviness in the epigastrium, changes in the nature and frequency of stool are observed. All this is associated with untimely release of bile into the duodenum and impaired digestion of fats, with duodenogastric and gastroesophageal reflux.
Neurological and autonomic disorders
Headache, feeling of a lump in the throat, sweating, drowsiness, fatigue, cardialgia, cold extremities, behavior changes, anxiety, hysteria, decreased learning ability and performance.
How does the disease manifest itself?
In order to diagnose the disease in time and begin treatment, you need to know about the symptoms characteristic of biliary hypertension:
- jaundice;
- malaise, loss of performance;
- abdominal pain, which is located in different parts of the abdominal cavity, has varying intensity and duration;
- dyspepsia – belching, nausea and vomiting;
- bloating, unstable stools, alternating diarrhea and constipation;
- regular pain in the area of the right hypochondrium.
Since doctors call the formation of neoplasms the main cause of the development of biliary hypertension, the disease itself can often be detected in advanced stages. After all, the growth of benign and malignant tumors occurs asymptomatically. Therefore, the listed symptoms must be treated carefully, because even nonspecific signs may indicate the development of biliary hypertension.
An increase in the size of the spleen is also considered a clear sign of pathology.
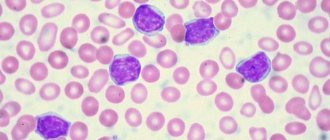
Simultaneously with the increase in biliary pressure, the patient experiences hypersplenism syndrome - a decrease in the number of blood cells (leukopenia, anemia, thrombocytopenia). The problem occurs in patients with diseases of the liver system, manifested by hepatosplenomegaly.
When biliary pressure increases due to insufficient outflow of bile secretions, fluid begins to accumulate in the patient's abdominal cavity; this symptom requires immediate medical intervention. In the initial stages, an indirect sign is local swelling - not only the spleen enlarges, the legs also swell.
Methods for diagnosing biliary tract dysfunction
The abundance and variety of symptoms of dysfunctional disorders of the biliary tract causes difficulties in making a diagnosis, which requires additional examination.
Screening diagnostic methods
Screening diagnostic methods include: biochemical studies of blood serum, ultrasound of the abdominal organs and endoscopy.
Clarifying methods
To clarify the diagnosis, ultrasound is used to determine the function of the gallbladder and sphincter of Oddi, dynamic cholescintigraphy, and ERCP.
Sign up for diagnostics To accurately diagnose the disease, make an appointment with specialists from the Family Doctor network.
Treatment of portal hypertension
The basis of therapy for the portal system is the elimination of the pathology that caused the disease.
Specialists provide comprehensive support to patients. It has several directions.
Diet therapy for hypertension
If there are disturbances in the functioning of the portal circulatory system, it is very important to reduce the amount of salt consumed (up to 3 g per day). This allows you to reduce fluid stagnation in the body.
Protein consumption is also reduced (up to 30 g per day). It is very important to distribute food intake evenly throughout the day. This reduces the risk of hepatic encephalopathy (brain damage from substances normally detoxified by the liver).
This therapy can be carried out on an outpatient basis. It is very important to undergo the necessary examinations regularly.
Conservative treatment for hypertension
A number of drugs are used for therapy:
- Pituitary hormones. These drugs can reduce hepatic blood flow and reduce pressure in the portal vein.
- Nitrates. These drugs are salts of nitric acid. They dilate blood vessels, leading to a reduction in blood flow to the liver.
- Beta blockers. These drugs reduce the frequency and strength of heart contractions. This reduces blood flow to the liver.
- Synthetic analogues of somatostatin (a hormone that is normally secreted by the brain and pancreas, suppresses the production of many other hormones and biologically active substances). The drugs reduce portal hypertension by narrowing the arterioles of the abdominal cavity.
- Lactulose preparations. These drugs remove harmful substances from the intestines that accumulate due to liver dysfunction and can cause brain damage.
- Diuretics. This group includes effective diuretics that can reduce excess fluid in the body.
- Antibacterial therapy is also prescribed. It allows you to remove from the body all microorganisms that cause various diseases.
Surgical treatment of hypertension
The operation is prescribed only if there are indications for its implementation. Usually, intervention is relevant if conservative therapy does not produce the desired results.
The main indications for surgical intervention when a portal defect is detected are:
- varicose veins of the stomach or esophagus,
- enlarged spleen,
- ascites (free fluid in the abdominal cavity).
Important! Indications for treatment are determined only by a doctor! At the same time, he always tells the patient about the features of the operation, its duration, complications, and risks. You can ask the specialist any questions you may have. Before any operation, a general diagnosis is carried out. It allows you to detect both indications and contraindications for the use of an intervention.
Methods of surgical treatment:
- Portosystemic shunting. This portal operation consists of creating an additional blood flow path from the portal vein to the inferior vena cava. In this case, the liver is not included in this circulatory system.
- Splenorenal shunt. This intervention comes down to creating additional blood flow from the splenic vein to the renal vein. The liver is also bypassed.
- Transplantation (liver transplant). This operation is performed when it is impossible to restore normal activity of the patient’s own liver. Usually the organ is taken from a close relative.
- Devascularization of the lower esophagus and upper stomach. This intervention consists of ligating (closing the lumen) some arteries and veins of the esophagus and stomach. Portal surgery is performed to reduce the risk of bleeding from the veins of the esophagus and stomach. Usually the spleen is also removed.
Important! All surgical interventions have a number of disadvantages. Abdominal surgery requires a long recovery. They are performed using general anesthesia. This negatively affects the condition of the patient's body. Each individual intervention has its own set of disadvantages. That is why it is always important to evaluate the feasibility of its implementation.
Request a call back Get a free consultation
Treatment methods for biliary tract dysfunction
Treatment of dysfunctional disorders of the biliary tract should be comprehensive and aimed at normalizing the outflow of bile and pancreatic secretion. To do this, it is necessary to normalize the diet and nature of nutrition. Food stimulates the contraction of the gallbladder, so meals should be divided, up to 5 times a day, in small portions, and it is advisable to eat meals at the same time. The diet should be structured so that the first half of the day accounts for 55-60% of its total calorie content. Excluded from the diet: carbonated drinks, rich broths, fatty meats, smoked foods, spicy, fried and canned foods, concentrates. Freshly prepared food in warm boiled, steamed or stewed form is recommended. Therapeutic nutrition is prescribed for at least 1 year, and if the pain syndrome persists for a long time - up to 1.5-2 years.
A special role in the treatment of biliary dyskinesias belongs to choleretic drugs, which are conventionally divided into:
- choleretics that stimulate bile formation by enhancing the functional activity of hepatocytes. These are preparations containing bile: allohol, cholenzyme, lyobil; synthetic drugs: nicodine, oxafenomide, cyclone; preparations of plant origin: corn silk extract, milk thistle extract, artichoke, smoker, flamin, holagol, hofitol, holosas, hepabene, etc.
- cholekinetics that stimulate bile secretion, cause an increase in the tone of the gallbladder, a decrease in the tone of the bile ducts and promote increased flow of bile into the duodenum: magnesium sulfate, sorbitol, xylitol.
To relieve pain, myotropic antispasmodics (halidor, drotaverine, baralgin, mebeverine, etc.) are used. Cholelytic agents (derivatives of deoxycholic acid), which normalize cholesterol production, and hepatoprotective agents, which have a complex effect on the hepatobiliary system (antispasmodic, anti-inflammatory and choleretic), can also be prescribed.
To improve the outflow of bile, it is good to carry out dubazhi according to Demyanov (blind probing), with magnesium sulfate (0.2-0.4 g/kg), mineral water “Magnesium Donat”, 1-2 times a week (for a course of up to 4-8 procedures).
Quite often, dysfunction of the biliary tract is a consequence of neurosis. For this purpose, vegetotropic therapy is indicated. Preference is given to herbal medicines:
- sedatives: valerian root, bromine, motherwort, sage.
- tonic preparations: eleutherococcus extract, tincture of aralia, Chinese lemongrass, freshly brewed tea, etc.
Prevention
Prevention of dysfunctional disorders of the biliary tract consists of prescribing a balanced diet, following a diet, eliminating stress, sanitizing secondary foci of infection, and prescribing dosed physical activity.
Dispensary observation
Children with biliary tract dysfunctions are monitored for a period of 2 years. The child must undergo preventive courses of therapy in the spring-autumn periods and during the period of remission: herbal medicine, hydrotherapy and balneotherapy.
Make an appointment Do not self-medicate. Contact our specialists who will correctly diagnose and prescribe treatment.
Rate how useful the material was
thank you for rating
Some aspects of diagnosis and differential diagnosis of obstructive jaundice
Ultrasound scanner WS80
An ideal tool for prenatal research.
Unique image quality and a full range of diagnostic programs for an expert assessment of a woman’s health.
Introduction
Obstructive jaundice (MF) is a pathological syndrome caused by a violation of the outflow of bile from the bile ducts of the liver into the duodenum (duodenum). The problem of diagnosis and differential diagnosis of the causes of obstruction of the biliary tract has not lost its relevance at the present time. Surgical interventions in patients with breast cancer, performed for emergency reasons, are accompanied by a large number of complications, and mortality reaches 15-30%, which is 4 times higher than in cases where breast cancer can be eliminated before surgery. Decompression of the biliary system is one of the main goals and an essential component of treatment in these patients [1-3].
Etiological factors of obstructive jaundice
- Malformations: biliary atresia; hypoplasia of the bile ducts; congenital common bile duct cysts; duodenal diverticula located near the major duodenal papilla (MDP).
- Benign diseases of the biliary tract: cholelithiasis (GSD), complicated by choledocholithiasis; driven stones BDS; inflammatory strictures of the biliary tract; BDS stenosis.
- Inflammatory diseases: acute cholecystitis with periprocess; sclerosing cholangitis; pseudotumorous pancreatitis; parasitic liver lesions in the area of the hepatic porta; inflammatory infiltrates in the area of the porta hepatis; acute papillitis; enlarged lymph nodes of the hepatoduodenal ligament.
- Tumors: papillomatosis of the bile ducts; cancer of the hepatic and common bile ducts (CBD); volumetric formations of the obstructive system; cancer of the head of the pancreas (PG); metastases and lymphomas at the gates of the liver.
- Structures of the main bile ducts developing as a result of surgical trauma.
Instrumental diagnosis of obstructive jaundice
- Ultrasound examination (ultrasound). The main sign of breast cancer on ultrasound is the dilation of the intrahepatic bile ducts (Fig. 1). Ultrasound allows not only to detect biliary hypertension, but also to establish the level of block. With a high biliary block (obstruction at the level of the hepatic hilum), ultrasound visualizes dilated intrahepatic ducts with a normal CBD diameter (up to 6 mm), the gallbladder is often of normal size or reduced, and a space-occupying formation may be detected in the hepatic hilum. With a low biliary block (obstruction at the level of the common bile duct, head of the pancreas, and obstruction), in addition to dilated intrahepatic ducts, dilated extrahepatic ducts are visualized, and the gallbladder is enlarged (Fig. 2). If the low block is caused by indurative pancreatitis, ultrasound shows an increase in the size of the organ, and calcifications in the pancreas may be detected (Fig. 3). With a tumor of the head of the pancreas against the background of biliary hypertension, a space-occupying formation in the pancreas is visualized (Fig. 4). The criteria for hypertension of the main pancreatic duct are its expansion of more than 2 mm in the body and more than 3 mm in the head of the pancreas. In case of cholelithiasis complicated by choledocholithiasis, an enlarged gallbladder with stones is detected, as well as stones in the common bile duct (Fig. 5). Focal liver lesions are diagnosed: echinococcal and alveococcal cysts; enlarged lymph nodes; places basins.
- Endoscopic retrograde cholangiopancreatography (ERCP).
- Percutaneous transhepatic cholangiography. ERCP and cholangiography under ultrasound control [1-3] may be accompanied by a subsequent therapeutic effect (installation of lost drainage, papillotomy, cholangiostomy).
- Computed tomography - CT and magnetic resonance imaging (MRI) of the liver and biliary tract.
Rice. 1.
Ultrasound picture of biliary hypertension in obstructive jaundice.
Rice. 2.
An echographic picture of a low liver block caused by a tumor of the head of the pancreas.
A)
Dilated intrahepatic ducts.
b)
Enlarged gallbladder with a thick suspension (red arrow) and dilated CBD (blue arrow).
Rice. 3.
Sonographic picture of chronic pseudotumor pancreatitis. Calcifications in the parenchyma of the pancreas.
Rice. 4.
Ultrasound picture of a pancreatic head tumor: formation in the pancreatic head (red arrow), dilated pancreatic duct (green arrow).
Rice. 5.
Ultrasound picture of biliary hypertension in obstructive jaundice caused by cholelithiasis, complicated by choledocholithiasis, stones in the gallbladder and CBD.
Differential diagnosis of obstructive jaundice
Differential diagnosis of obstructive jaundice, first of all, should be carried out with parenchymal jaundice.
Parenchymal jaundice occurs with hepatitis and cirrhosis of the liver and develops gradually. The main distinguishing ultrasound sign of parenchymal jaundice from mechanical jaundice is the absence of dilation of the intra- and extrahepatic bile ducts.
Ultrasound signs of acute viral hepatitis [4] include an increase in the size of the liver due to both lobes; in the later stages, a decrease in the size of the liver is possible (symptom of a melting ice cube); echogenicity of the parenchyma is low (symptom of dark liver); the structure can be homogeneous due to pronounced edema of the parenchyma or heterogeneous (a symptom of protruding vessels); more pronounced enrichment of the vascular pattern; reduction in the diameter of the main trunks of the hepatic veins; a slight increase in the diameter of the main trunk of the portal vein; decrease in speed and volume blood flow through the portal vein; enlarged lymph nodes in the hepatoduodenal ligament; splenomegaly (increase in the area of the spleen by more than 50 cm²).
Ultrasound signs of chronic hepatitis [4] include enlarged liver; the contour of the liver is clear and even; rounding edges and increasing corners; the structure of the organ is diffusely heterogeneous; the echogenicity of the parenchyma is increased; depletion of the vascular pattern in the periphery; the main trunk of the portal vein is not dilated.
Ultrasound signs of liver cirrhosis [5-7] include an increase in liver size at the initial stage and a decrease in the terminal stage; hypertrophy of the caudate lobe of the liver; the contours become uneven and lumpy; the capsule is not clearly differentiated; the structure of the parenchyma is diffusely heterogeneous with multiple areas of increased echogenicity (foci of fibrosis) and decreased echogenicity (foci of regeneration); depletion of the vascular pattern in the periphery.
With the development of portal hypertension [5, 7, 8], typical echographic signs are revealed: an increase in the diameter of the portal vein with a decrease in the linear velocity of blood flow; change in the lumen of the portal vein during deep inspiration is no more than 10%; an increase in the diameter of the splenic (over 8 mm), superior and inferior mesenteric veins; an increase in the diameter of the extrahepatic part of the portal vein over 15 mm; hepatofugal direction of blood flow; identification of various porto-portal and porto-caval collaterals (Fig. 6); splenomegaly; ascites.
Rice. 6.
Echogram of portal collaterals of the portal vein.
A)
B-mode. Absence of the typical tubular anechoic portal vein trunk with hyperechoic walls. The trunk of the portal vein is visible as a heterogeneous formation with many echogenic septa running parallel to the walls of the vessel (arrow). The presence of hyperechoic areas in the paravenous region of the portal vein.
b)
Color flow mode. Pronounced large collaterals in the projection of the portal vein.
With parenchymal jaundice, histological verification of the diagnosis is desirable. For this purpose, it is recommended to perform a puncture aspiration biopsy (PAB) of the liver under ultrasound guidance.
Clinical observation
Patient L., 73 years old, was admitted to the hospital with complaints of yellowing of the skin.
Ultrasound of the abdominal cavity: intrahepatic ducts are dilated (segmental up to 6 mm, lobar up to 10 mm). CBD 14-15 mm. Gallbladder 120 30 mm, wall 3 mm, no stones detected. The pancreas is of normal size, the contours are smooth and clear. The structure is diffusely heterogeneous, with increased echogenicity. The pancreatic duct is dilated to 5 mm. Conclusion: ultrasound picture of a low liver block with biliary hypertension, a block at the level of the LBD, terminal part of the CBD (Fig. 7).
Rice. 7.
Sonographic picture of a tumor of the BDS.
A)
An enlarged gallbladder with a thick suspension inside (red arrow) and an enlarged CBD (blue arrow).
b)
Dilation of the intrahepatic ducts (blue arrow).
V)
Dilatation of the pancreatic duct (green arrow).
Multislice CT with bolus contrast: intra- and extrahepatic bile ducts are dilated (lobar up to 9 mm, common hepatic duct (CHD) 14 mm, intrapancreatic part of the common bile duct 12 mm). The Wirsung duct is dilated throughout its entire length to 6 mm. In the BDS projection, a soft tissue formation up to 11 mm is visualized and accumulates contrast. Conclusion: BDS tumor with low liver block.
ERCP performed with endoscopic papillosphincterotomy (EPST) established: the LDS is significantly increased in size, tense, infiltration of the mucosa in the area of the mouth, structureless small-tuberous growths, contact vulnerability, catheterization with a lateral papillotome was unsuccessful. The longitudinal fold was dissected with an end papillotome to form a suprapapillary fistula. With ERCP, the dilated common bile duct is contrasted, interrupted at the level of the intrapancreatic department, without evacuation of contrast. A “lost” common bile duct drainage (7 cm) was installed into the fistula via a guidewire, and an outflow of contrast into the intestine was obtained. Conclusion: endoscopic picture of the BDS tumor. Condition after ERCP, EPST. Installation of a “lost” common bile duct drainage.
Thus, the diagnosis was made: papillary adenoma of the BDS. Acute cholecystitis. Paravesical abscess. Mechanical jaundice.
conclusions
- Radiation diagnostic methods provide significant assistance in the diagnosis and differential diagnosis of breast cancer.
- Ultrasound plays a decisive role in the diagnosis and differential diagnosis of breast cancer in primary care.
- At the second stage of the study, depending on the level of the block, ERCP (possibly in combination with EPST), CT, MRI, percutaneous transhepatic cholangiography under ultrasound control are indicated.
- Minimally invasive endoscopic and percutaneous transhepatic decompression interventions are an effective way to restore bile outflow in case of obstruction of the biliary system. These techniques make it possible to quickly and effectively eliminate jaundice and cholangitis, make it possible to carry out surgical interventions in the most favorable conditions, in a planned manner, and in elderly patients with severe concomitant pathology they can serve as an alternative to surgical treatment.
Literature
- Tannapfel A., Wittekind C. (2004). Gallbladder and bile duct carcinoma. Biology and pathology. Internist 45: 33-41.
- Valle J., Wasan H. et al. (2010). Cisplatin plus gemcitabine versus gemcitabine alone for billiary tract cancer. N Engl J Med 362:1273–1281.
- Wiedmann M. W., Mossner J. (2010). Molecular targeted therapy of biliary tract cancer - results of the first clinical studies. Curr Drug Targets 11:834–850.
- Balashov A.T. Possibility of using ultrasound in determining the severity of acute viral hepatitis (literature review) // Medical visualization. 2007, N 1. P. 32-37.
- Mikhailov M.K. Echography in the diagnosis of cirrhosis. M.: MEDpress-inform. 2003.
- Shipov O.Yu., Syutkin V.E., Matyukhina A.P., Ivanikov I.O. Features of the ultrasound picture in patients with liver cirrhosis with varying degrees of activity of alcoholic hepatitis // Medical journal “SonoAce-Ultrasound”. 2007. N 16. P. 46-51.
- Annet L., Materne R., Danse E. et al. Hepatic flow parameters measured with MR imaging and Doppler US: Correlations with degree of cirrhosis and portal hypertension // Radiology. 2003. V. 229. P. 409-414.
- Vasiliev V.A., Lisachenko N.A., Tsekhanovich K.B. Possibilities of ultrasound Dopplerography of the portal system in the diagnosis of viral hepatitis // Materials of the III scientific and practical conference with international participation. Petrozavodsk. 2004. pp. 82-83.
Ultrasound scanner WS80
An ideal tool for prenatal research.
Unique image quality and a full range of diagnostic programs for an expert assessment of a woman’s health.
Use of modern techniques in the treatment of hypertension
Today, perhaps the most progressive method used to eliminate portal hypertension (PH) is the method of endovascular transjugular intrahepatic portosystemic shunt (TIPS). It is precisely this method in the treatment of portal hypertension that is used by specialists in our endovascular surgery center. Such popularity of the use of TIPS in clinical practice lies in the fact that endovascular (intravascular) intervention has proven its validity in practice, since it is the most effective and gentle in the treatment of liver cirrhosis in patients of the Child B and Child C groups: it is in these cases that the dysfunction of the main indicators of homeostasis are extremely evident.
Also, this method is particularly effective in the treatment of many complications of the above disease, such as bleeding from the veins of the stomach and esophagus, susceptible to varicose veins, ascitic syndrome, and hepatic hydrothorax.
When using transjugular intrahepatic portosystemic shunting (TIPS) as a method of intravascular therapy and prevention of bleeding from varices of the esophagus and stomach, ascitic syndrome in portal hypertension syndrome, intravascular intervention in the vast majority of cases causes a critical reduction (up to 40%) in the degree of portal hypertension already in within two weeks. This treatment can be combined with simultaneous embolization of thickened and dilated veins of the esophagus. This integrated approach ensures the cessation of bleeding, as well as a drop in pressure in the portal vein system.
When carrying out intravascular therapy for portal hypertension, specialists, as a rule, additionally reduce hepatic and splenic blood flow, due to which the degree of pathology decreases.
When acute bleeding from varicose veins of the esophagus is detected, specialists first of all use drug vasoconstrictor therapy and balloon tamponade of the veins with a Blackmore probe. After carrying out these emergency measures, taking into account expediency, it is customary to use endovascular and endoscopic (sclerotherapy of veins, ligation) comprehensive preventive measures to prevent recurrent bleeding. At this stage, TIPS is used as the most effective method, eliminating failures that can occur, for example, during surgical operations, as well as in the ineffectiveness of drug and endoscopic treatment.
In what cases is the TIPS method used in the treatment of portal hypertension?
Treatment using the TIPS technique is carried out for:
- hepatorenal syndrome;
- refractory diuretic-resistant ascites;
- acute and recurrent bleeding caused by varicose veins of the esophagus;
- hepatic hydrothorax;
- bleeding from gastric varices;
- Budd-Chiari disease and syndrome;
- ectopic variceal bleeding (anorectal, intestinal, from stoma);
- portal gastropathy (with hypertension, the mucous membrane has a mosaic appearance) and vascular ectasia of the antrum (the presence of linear or diffuse scarlet lesions on the inner surface of the antrum of the stomach);
- hepatopulmonary syndrome.
Method of applying an intrahepatic portacaval shunt
This medical intravascular intervention is quite complex, and therefore is performed in our center only by highly qualified specialists who have undergone special training. First of all, puncture of the right jugular vein located in the neck is performed. It is here that a special introducer is installed, through which X-ray contrast examination of the hepatic vein is carried out using a catheter.
Then this catheter, which performs a diagnostic function, is replaced with a thicker medical conductor, through which a special curved needle is inserted. It is she who performs a liver puncture. While the tip of the needle is in one of the branches of the portal vein, a conductor-string is inserted into it, along which a balloon catheter is placed into the liver tissue, and then staged dilatation of the liver tissue is performed.
Next comes the stage of stenting the created intrahepatic canal. Typically, self-expanding or matrix covered and metallic stents can be used for this purpose.
Practice has shown that the use of so-called covered stents (stent-grafts) is the most effective and successful for this surgical intervention, as the quality and patency of the transhepatic shunt improves.
The clinical effectiveness of TIPS can be assessed by regression or complete cessation of the symptoms of portal hypertension: absolute cessation of esophagogastric bleeding, elimination of varicose veins of the stomach and esophagus, as well as veins of the anterior abdominal wall, reduction in the amount of transudate and the dose of diuretics in the treatment of ascitic syndrome, etc.
After surgery, patients are prescribed a course of diuretic, infusion and homeostatic therapy. If necessary, our specialists also recommend endovascular embolization of gastric and esophageal varices, as well as embolization of the splenic or hepatic artery.