Such different noise: main types
By nature, heart murmurs in a child can be:
- diastolic (occurring when the heart relaxes and fills with blood; often pathological);
- systolic (arising against the background of blood vessels pushing out; in most cases they are safe).
Noises can also be functional or organic. The first arise temporarily during the period of increase in the size of the heart and blood vessels along with human growth. The latter are directly related to damage to valves, blood vessels and pericarditis.
Functional noise
Functional heart murmurs in a child are not dangerous. They are not associated with anomalies in the development of the organs of a small person and do not bring him pain or discomfort. Most often, such heart murmurs occur at 1-2 years of age. As they grow older, they disappear spontaneously.
Such children are monitored by a cardiologist. In this case, no changes or abnormalities are detected on the X-ray image or on the ECG printout.
The causes of noise in this situation may be:
- thinness of the baby's chest;
- strong sound of venous blood flow;
- the presence of an additional chord;
- disturbance of metabolic processes in the heart muscle;
- anemia.
All these violations are not dangerous, they can be easily corrected.
Organic noises
Organic heart murmurs in a 2 or 3 year old child occur due to congenital or acquired heart diseases. They appear due to the formation of abnormal blood flows in large vessels. It is their swirls that are listened to by the doctor.
Such noises are quite loud and continuous. The reasons for their appearance may be:
- rheumatism;
- myocarditis;
- heart defects.
answers to some questions / 7. differential diagnosis / 104. differential diagnosis of heart murmurs
By origin S. sh. are usually divided into organic, associated with defects or aneurysm of the heart or vessels extending from it, and functional, caused, for example, by accelerating blood flow, reducing its viscosity, incl. and so-called innocent heart murmurs, often detected in healthy people, especially in children and young people.
In relation to the phases of the cardiac cycle ( Fig. 2, 3
) heart murmurs are divided into systolic, i.e. heard between the 1st and 2nd heart sounds (in the systole phase), and diastolic, heard in the diastolic pause between the 2nd and 1st heart sounds. S. sounds that occur during systole and continue after the second heart sound are called systolic-diastolic murmurs. Depending on what part of systole or diastole the noise occupies - initial, middle, final (late), it is designated as proto-, meso- and telesystolic (or proto-, meso- and telediastolic), respectively, and if it is heard from the beginning until the end of the pause - as pan-, or holosystolic (respectively, pan-, or holo-diastolic). Telediastolic murmur is more often called presystolic.
Listened S. sh. can be short and long, increasing, decreasing, increasing-decreasing (on a phonocardiogram - diamond-shaped, spindle-shaped), etc. In terms of pitch and timbre, the noise can be rough, gentle, blowing, scraping, sawing, rumbling, musical. The loudness of the murmur depends on many conditions, so in itself it cannot be a characteristic of the severity of a defect or other heart lesion. In thin people with a thin chest wall, as well as in children, murmurs are louder than in obese people. Pulmonary emphysema reduces the sonority of noises due to the air gap separating the heart from the anterior chest wall. In heart failure, the intensity of many murmurs caused by organic valve disease decreases, and sometimes these murmurs even disappear. Volume of diastolic S. sh. decreases with tachycardia (due to shortening of diastole); these noises usually disappear when the heart rate exceeds 100 per minute
. Due to respiratory fluctuations in cardiac output, the intensity of S. sh. may vary according to the phases of breathing; Intracardiac murmurs, both valvular and extravalvular, sharply weaken when straining after a deep breath. During physical exertion, mental excitement, fever, when the speed of blood circulation increases, the strength of S. sh. usually increases; in this case, it is often possible to listen to noises that are not detectable under normal conditions. S. sh. caused by valve defects, are best heard in a horizontal position of the patient, but in general they are less dependent on changes in body position than functional noises.
Diagnostic value of heart murmurs
. Murmurs that occur with heart defects have characteristics of origin and sound that reflect the nature of the pathology. Depending on the type of defect, the murmur is formed in certain phases of the cardiac cycle, so determining the phase of the cardiac cycle in which the murmur is heard has diagnostic significance.
Systole-diastolic murmurs occur when there is a septal defect in the heart or a shunt between large vessels. The most common cause of this noise is a patent ductus arteriosus.
.
The noise begins immediately after the first tone ( Fig. 3, f
) with a slight deviation from it. As the pressure in the aorta increases, the volume of the noise increases. The pressure gradient between the aorta and the pulmonary trunk reaches a maximum at the end of systole, and at the same time the maximum sound of the murmur is noted. It ends in the middle or at the beginning of diastole. The noise is often accompanied by shaking. Gromkiy S. sh. heard over the entire region of the heart, but has maximum intensity in the second left intercostal space, from where it radiates to the third intercostal space; When the patient is lying down, the noise intensifies. An aneurysm of the sinus of Valsalva, when it ruptures into the right ventricle, is accompanied by a systolic-diastolic murmur, which is heard to the left of the sternum. The diastolic component of the murmur is louder than the systolic component.
Systolic murmurs are heard most often, because formed in a variety of heart diseases, including myocarditis, cardiosclerosis, cardiomyopathy, as well as anemia and hyperkinetic syndrome; they make up the largest portion of “innocent” noises in practically healthy individuals and, in addition, can be important auscultatory symptoms of the most common valvular heart defects - insufficiency of the atrioventricular valves or stenosis of the aorta or pulmonary trunk (see.
Acquired heart defects
), as well as septal defect of the heart.
In mitral regurgitation, systolic murmur occurs due to regurgitation of blood from the left ventricle into the left atrium. It begins immediately after the weakened first sound and decreases towards mid-systole ( Fig. 3, a
), but often continues until the beginning of the second tone, i.e.
happens pansystolic. The noise may have the same intensity throughout the entire systole, but may intensify towards the end of it, often having a blowing character. Damage to the papillary muscles during acute myocardial infarction
, traumatic separation of the papillary muscles leads to the formation of acute mitral regurgitation; in this case, a rough and prolonged systolic murmur is heard, which begins with separation from the first tone, has a diamond shape, and is sometimes carried out to the vessels of the neck and into the interscapular space. Telesystolic (late) murmur is often heard in patients with atherosclerotic cardiosclerosis, with sclerotic degeneration of the papillary muscles, as well as with mitral valve prolapse.
The systolic murmur of tricuspid regurgitation is better heard at the base of the sternum, often intensifies at the height of inspiration and often has varying intensity, in contrast to the stable murmur of mitral regurgitation. Inconsistency of noise is more typical for relative tricuspid insufficiency. As the patient's condition improves, the sound of organic failure does not change or even intensifies due to increased contractility of the right ventricular myocardium, while the sound of relative failure becomes quieter or disappears.
A systolic murmur in the second intercostal space to the right of the sternum is characteristic of aortic stenosis (ejection murmur). Most often it has a diamond-shaped or spindle-shaped shape, it begins with some separation from the first tone ( Fig. 3, b
), ends before the beginning of the second sound, often radiating to the apex of the heart and carotid arteries.
The systolic murmur of aortic stenosis is usually accompanied by trembling of the chest wall determined by palpation (“cat purring”). The same systolic ejection murmur, but in the second left intercostal space, is heard with stenosis of the mouth of the pulmonary trunk ( Fig. 3, d
). Sometimes it is best heard in the third or fourth intercostal space, to the left of the sternum.
Systolic murmur with a ventricular septal defect is loud, prolonged, sharp and even rough, accompanied by tremors, the epicenter of which is in the third or fourth intercostal space, at the left edge of the sternum. The murmur usually covers the first sound and occupies the entire systole ( Fig. 3, c
), sometimes it is registered as increasing-decreasing. In a horizontal position, the noise is louder, often heard at a distance, and is carried into the interscapular space. After the introduction of mezatone, it becomes more intense; sublingual administration of nitroglycerin reduces its intensity.
With an atrial septal defect, the systolic murmur begins immediately after the first sound, it is not intense, blowing, and is accompanied by a bifurcation of the first sound. The intensity of the noise increases with physical activity, but does not reach the degree that occurs with ventricular septal defects.
Diastolic murmurs are almost always associated with organic heart pathology. Most often, diastolic murmurs are caused by insufficiency of the aortic valve or pulmonary trunk or stenosis of the atrioventricular orifices.
The diastolic murmur of aortic insufficiency begins at the very beginning of diastole, during the period of the second sound, which is often replaced or covered by this noise. The noise is high-frequency, gentle, usually blowing. The duration of the murmur depends on the severity of aortic insufficiency. With minor aortic insufficiency, the diastolic murmur is short (protodiastolic; Fig. 3, e
), it is difficult to detect, only in the absence of extraneous noise. With more severe aortic insufficiency, it occupies 1/2-2/3 of diastole and is characterized by decreasing intensity; with severe aortic defects, the murmur often occupies the entire diastole. Many researchers believe; that in severe aortic insufficiency the murmur is usually more intense. It is heard at the auscultation point of the aortic valve and at the fifth point, and is better heard with the patient lying on his stomach with calm, shallow breathing.
A fading diastolic murmur in the second (less often in the third) intercostal space to the left of the sternum is a sign of pulmonary valve insufficiency. With relative pulmonary valve insufficiency resulting from hypertension of the pulmonary circulation
, a quiet blowing diastolic murmur, called Still's murmur, is heard. It begins immediately after the second sound and is heard in a limited area in the second intercostal space on the left; in cases of bifurcation of the second tone, the noise begins from its second component.
The diastolic murmur of mitral stenosis occurs immediately after the second component of the bifurcated II tone, has presystolic amplification, often musical, and is accompanied by chest trembling. The murmur is usually low-frequency, better heard at the apex of the heart when the patient is horizontally positioned on the left side, and intensifies after physical activity. It can occupy the entire diastole; in this case, it first decreases, and then, approximately from the middle of diastole, continues with a constant amplitude until presystolic increase ( Fig. 3, e
), associated with atrial systole. This is explained by the fact that during the phase of rapid filling of the left ventricle, blood rushes at high speed through a narrow opening, creating a noise that subsides as the flow rate decreases and intensifies again with its additional acceleration associated with atrial systole. With atrial fibrillation, there is no presystolic increase in noise. Along with diastolic murmur, an increase in the first tone and a bifurcation of the second tone are detected, which creates the so-called melody of mitral stenosis.
Diastolic murmur with presystolic amplification is determined with myxoma of the left atrium (see Heart
), it is variable, its appearance and intensity depend on the position of the body and the speed of blood flow.
With severe organic aortic insufficiency, functional stenosis of the left atrioventricular orifice occurs due to the fact that the blood stream regurgitating into the left ventricle lifts the mitral valve leaflet. In this case, a diastolic murmur with presystolic amplification (Flint murmur) is heard at the apex of the heart. It is not as long and loud as with organic mitral stenosis, and is not accompanied by an increase in the first sound and the sound of the mitral valve opening.
Often, in children with mitral valve insufficiency and ventricular septal defect, with significant dilatation of the atria or ventricles, a fusiform diastolic murmur is detected,
separated by an interval from the second tone and lasting no more than 0.2 s
(Coombs noise); it is heard near the apex of the heart only in the presence of a third sound.
Diagnostic differentiation of cardiac murmurs is carried out primarily with extracardiac (paracardial) murmurs. The greatest similarity with S. sh. have pericardial friction rub, cardiopulmonary and pleuropericardial murmurs. Pericardial friction noise is detected in pericarditis, myocardial infarction, usually in the form of short scratching sounds during systole or diastole or in both phases. Cardiopulmonary (cardiopulmonary) murmurs occur in those parts of the lungs that are in contact with the heart. Changes in the size and position of the heart during systole cause rapid movement of air in the adjacent areas of the lungs, which generates high-frequency noise. Cardiopulmonary murmurs are often heard in persons with a reduced anteroposterior chest size, in young people with excited cardiac activity (the so-called hyperkinetic type of cardiac activity), as well as in cases of severe cardiac hypertrophy. They are usually heard during systole, and when breathing is held during exhalation, they usually disappear. Pleuropericardial murmurs, i.e. friction noises that occur with dry pleurisy in the areas of contact between the pleura and the pericardium intensify during inspiration. When differentiating the nature of murmurs, it is also necessary to remember about the various vascular murmurs.
Significant difficulties sometimes arise when differentiating organic and functional S. sh. To distinguish organic and “innocent” noises, various techniques (physical activity, change of body position) and pharmacological tests were proposed. Taking nitroglycerin causes an increase in the systolic murmur of aortic stenosis, a weakening of the murmur of mitral regurgitation and an increase in the systolic murmur of tricuspid regurgitation. Functional pulmonary systolic murmur is heard in the second intercostal space, at the edge of the sternum. The murmur usually has a spindle-shaped shape and occupies the first half of systole, always blowing, is better heard when the patient is lying down, and intensifies under the influence of stress and with fever. Exhalation improves the audibility of this noise. An “innocent” aortic systolic murmur occurs due to systolic vibration of the distended aortic root. It occupies mid-systole, is heard in the second intercostal space, and is usually carried out to the apex of the heart at the right edge of the sternum.
Diagnosis of the nature of the North. more accurate for dynamic noise estimation. As heart function improves, organic murmurs usually become more distinct. We can also assume that murmurs heard in the diastole phase and murmurs that occupy the entire systole are never “innocent”. If there is doubt about the nature of the noise, a comprehensive examination of the patient and dynamic observation is necessary.
Causes of pathology at different ages
Infants
Why does my child have a heart murmur? When analyzing the reasons, pay attention to the age of the young patient. Each age has its own primary sources.
For example, heart murmurs in a newborn baby appear against the background of:
- congenital pathologies;
- unclosed oval window;
- active ductus arteriosus.
Normally, the oval window closes already in the 1st or 2nd year of the baby’s life. But even if it is observed in older children, it is considered not a developmental defect, but an individual feature of the body’s functioning.
Children over one year old
Heart murmurs in a child aged 4, 5, 6 or 7 years can be caused by both health problems and non-dangerous conditions: thinness, mild temporary overload or an unstable psycho-emotional state (whims against the background of the next transition period from the category of small children to the category preschoolers).
The danger comes from those noises that occur in parallel with acute respiratory or viral diseases (sore throat, scarlet fever). The fact is that during illness, pathogenic microflora has a harmful effect on the heart. For this reason, children often develop a disease such as rheumatism.
Pupils
Heart murmurs in an 8-year-old child or even when starting school are associated with:
- with an unbalanced diet;
- with increased physical and mental stress;
- with stress.
Because of this, the myocardium receives much less oxygen and nutrients than it needs. At the same age, there is a discrepancy in the size of the heart sac, which also provokes audible murmurs.
Teenagers
Adolescents are considered a separate category of patients. A heart murmur in a child 10 years of age or older usually occurs due to an imbalance in the influence of the autonomic or sympathetic nervous system. As we grow older, this imbalance disappears along with extraneous noise from our main organ.
At the same time, you still need to control the situation, since various myocardial diseases and other pathologies can be detected in adolescents.
What are “innocent” noises and their features
The name “innocent” speaks for itself: these are extraneous sounds that are not associated with significant pathologies in the organ and do not affect the condition and functioning of the baby’s heart. In this case, neither an ECG nor an ultrasound of the heart reveals any problems.
This type of noise differs in the nature of its sound during auscultation: extraneous sounds are short, unclear, barely audible. In newborns, they are most often caused by changes in blood circulation associated with changes in living conditions and adaptation to extrauterine development. Over time they pass.
If we talk about children under 5 years old, the appearance of noise can be associated with various factors. The impact can be caused by emotional overexcitation, the development of anemia or rickets, physical activity, and fatigue.
Very often, pediatricians refer children aged 4-5 years and adolescents 12-15 years old for consultation with a pediatric cardiologist. Practice shows that it is at this age that noises that were not previously detected most often appear. In most cases, the reason for them lies in the intensive growth of the child, i.e. when the size of the organ and the heart sac does not have time to “catch up” in size with the development of the whole organism, and the myocardium has to work with “overload”. Once development and growth are balanced, the noise goes away. But during the most stressful period, you should adhere to some recommendations, which the pediatric cardiologist at the Happy clinic will definitely tell you about at your appointment.
Some types of cardiac abnormalities can also cause “innocent” murmurs. One of the most common is the pseudochord, i.e. a thin thread connecting the opposite walls of the left ventricle. However, there is also a nuance here: the direct location of this false chord is very important, and if it does not interfere with blood flow, then there is no cause for concern, but if it disrupts the heart rhythm, then the help of a pediatric cardiologist becomes mandatory.
Diagnostics
If murmurs are detected during listening by a pediatrician, neurologist or cardiologist, then the patient must undergo a comprehensive diagnosis. It includes:
- conducting an electrocardiogram (shows disturbances in the functioning of the heart, for example, disturbances in rhythmic activity or chamber hypertrophy);
- performing radiography (demonstrates the boundaries of the hematopoietic organ and the condition of both lungs);
- carrying out echocardioscopy (ultrasound examination will show the condition of the valves, vessels and cavity of the heart, growths, narrowings and pathologies).
The main task of the doctor is to accurately differentiate the type of eshum. We need to thoroughly understand what is the true reason for their appearance. This will help you not waste time and prevent a serious illness from developing.
You need to remember that even if you listen to noises, but the child does not have any complaints, there is nothing to worry about. Those noises that are accompanied by pallor of the skin, blueness of the nasolabial triangle, shortness of breath and elevated temperature should be alarming. The baby may complain of chest pain, be capricious and refuse to eat. In such a situation, urgent examination and consultation with a specialist is necessary.
What is the treatment of heart murmurs in children?
If murmurs are detected in children, their treatment is selected based on the cause of the symptom. If there are no organic heart lesions, the child is cheerful, cheerful and visually healthy, then no treatment is prescribed. The absence of complaints indicates that the body is doing its job well.
In the vast majority of cases, the cardiologist prescribes medications. Special medications will help:
- improve myocardial nutrition;
- normalize metabolic processes in the heart muscle;
- strengthen the child’s body’s defense system.
Vitamins and amino acids are also prescribed in combination with medications. In some situations, if prescribed by a doctor, hormonal agents and diuretics are also added to this regimen.
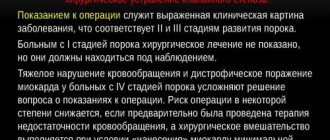
Particular attention is paid to patients in whom congenital or acquired pathologies were identified during diagnostic studies. As a rule, such children undergo surgery. In such cases, it is impossible to solve the problem without surgical intervention.
The operation can be aimed at:
- removal of excess tissue;
- stent insertion;
- valve replacement.
Our clinic provides surgical treatment for children, after which the rehabilitation period does not take much time. Children quickly return to their usual active life. At the same time, they must take blood thinning medications for some time, as well as take medications to speed up recovery and prevent complications.
What to do if you find a heart murmur?
It is important to remember that if your baby is diagnosed with a heart murmur, then you need to gather yourself as much as possible, do not panic and do not make any independent predictions in advance. Children's organisms, although small, are endlessly striving for life. Even in the case of pathologies, if the child is given timely help, everything can turn out well.
To understand the situation, determine the original source of these noises and eliminate it, you need to undergo diagnostics, and then a course of treatment from a qualified doctor.
How to make an appointment with a doctor
There can be many causes of heart murmurs in a child. To exclude dangerous pathologies or receive comprehensive treatment for the disease in a timely manner, you need to seek help from a specialist. The clinic is attended by experienced cardiologists who thoroughly study the situation, compare the results of diagnostic studies, make an accurate diagnosis and take a whole range of measures to effectively combat it.
Our doctors find an approach to each child, taking into account all the developmental features, previous diseases, and return. All this is necessary in order to establish a diagnosis and prescribe a truly appropriate treatment.
To get a consultation with a cardiologist at JSC “Medicine” (academician Roitberg’s clinic), you can call 24/7 or fill out an online appointment form on the website.
The clinic is located at the address: Mayakovskaya metro station, 2nd Tverskoy-Yamskaya lane, 10.
What are “pathological” noises, their causes and dangers
Pathological are those types of heart murmurs that are a consequence of pathology and indicate the presence of a congenital defect. During auscultation, you can pay attention to their distinct character, rough sound, very audible, long-lasting, most often spreading over the surface of the chest. There are cases when congenital defects do not manifest themselves as heart murmurs in a newborn, but appear a month or two later. A dangerous indicator in this case is their increase in dynamics.
As a rule, the pathological type of murmur is accompanied by changes in the ECG, but there are also “invisible” exceptions. The pathology they indicate can be detected by x-ray examination of the organ.
Pathological noises can indicate the presence of problems such as:
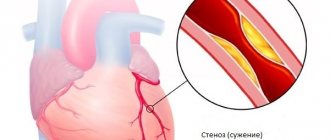
- stenosis (mitral, aortic or pulmonary artery);
- development of hypertrophic cardiomyopathy;
- tricuspid valve insufficiency;
- Ebstein's anomaly;
- endocarditis;
- heart failure;
- defect of the interchamber septum;
- the appearance of cardiac myxoma (a rare type of benign tumor) and many other very serious diseases.
Unfortunately, the absence of murmurs is also not a guarantee that there is no pathology developing in the heart in the child’s body, so it is very important to carefully monitor any abnormalities, and if even small problems appear, be sure to discuss them with the pediatrician. Fatigue, weakness, pallor (especially if it is accompanied by blueness of the fingers, lips, tip of the nose), shortness of breath - all this may indicate cardiac pathology.
We all know that the heart is the most important organ that ensures the vital functions of the entire body, therefore its health should be given increased attention from the very birth of the baby.