Pediatrician (working with children of the first year of life)
Murzina
Oksana Yurievna
21 years of experience
Pediatrician of the highest category, member of the Union of Pediatricians of Russia
Make an appointment
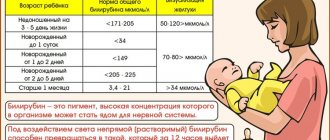
Jaundice in newborns (most often physiological) is a condition in which the skin and whites of the eyes turn yellow due to high levels of a substance called bilirubin in the blood. Most babies develop 2-3 days after birth. Bilirubin is a yellow substance resulting from the destruction of hemoglobin during the natural replacement of red blood cells. Under normal conditions, it should be processed quickly in the liver. According to medical statistics, jaundice is diagnosed in 50-60% of cases in newborns born at term, and in 80% of premature infants. Bilirubin in excess amounts has a toxic effect on internal organs.
Causes of the disease in infants
Jaundice in newborns can have the following causes:
- increased breakdown of hemoglobin due to Rh conflict;
- blood type conflict between mother and baby;
- maternal and infant infections;
- birth injuries;
- hypothyroidism (decreased thyroid function);
- polycythemia (increased number of red blood cells);
- reaction to breast milk;
- congenital hepatitis;
- pyloric stenosis (congenital pathology of the stomach).
Bilirubin - what is it?
Bilirubin is a substance that occurs naturally in the body. It is a breakdown product of hemoglobin. Hemoglobin itself is a component of red blood cells, its task is to saturate the tissues of our body with oxygen. Red blood cells live in the body for 3-4 months, after which they are destroyed along with hemoglobin. At this point, free or indirect bilirubin enters the blood.
Although bilirubin is produced naturally in the body, it is in a toxic fat-soluble form, so the body tends to get rid of it. But bilirubin cannot dissolve in the blood, so the body first processes it with special proteins. They bind indirect bilirubin and convert it into water-soluble, after which it passes to the liver, which acts on it, turning it into a safe component. The substance is then excreted in the usual way: with feces and urine.
What are the symptoms in babies?
Symptoms may range from mild to severe. This depends on the level of bilirubin in the blood and the duration of the disease. The causes and consequences of jaundice in newborns can vary, but there is one common characteristic - jaundice of the skin and sclera. It is worth noting that the eyes show symptoms faster. The baby may experience increased drowsiness with a decreased sucking reflex. Convulsions may occur. Without treatment, advanced jaundice can cause deafness, mental retardation and paralysis.
Does your newborn have symptoms of jaundice?
Only a doctor can accurately diagnose the disease. Don't delay your consultation - call
Parenchymal jaundice
It develops when liver cells are damaged by infectious or toxic agents, which leads to a decrease in their ability to bind bilirubin. In the first place in this series are intrauterine infections: cytomegalovirus (it is the cause of approximately 60% of all cases of prolonged jaundice in infants), toxoplasmosis, listeriosis, rubella, viral hepatitis. As a rule, the idea of an intrauterine infection arises with the development of prolonged jaundice (when its duration exceeds 2-3 weeks in full-term newborns and 4-5 weeks in babies born prematurely), as well as in the presence of other symptoms (enlargement of the liver, spleen and peripheral lymph nodes , anemia (decrease in the level of hemoglobin in the blood), darkening of urine and discoloration of feces, signs of inflammation in a general blood test (increased number of leukocytes, increased ESR), increased levels of liver enzymes in a biochemical blood test. To make a diagnosis, serological reactions are used (detection in the blood antibodies to viruses or bacteria), detection of RNA or DNA of the pathogen using PCR (polymerase chain reaction is a method that allows you to “recreate” DNA or RNA from small fragments that are found in biological fluids or tissues of the body. After this, the resulting RNA or DNA is examined for species (i.e. determine the type of pathogen).
Main and rare types of disease
Increased bilirubin in infants is considered normal, but only in the first few days. Gradually the figures are decreasing. If this does not happen, we are talking about the development of a pathological process.
Types of jaundice in newborns (depending on the reasons for its occurrence and severity):
- physiological;
- hemolytic;
- conjugative;
- neonatal;
- nuclear;
- parenchymal;
- obstructive;
- pathological4
- mechanical.
Classification of newborn jaundice allows you to accurately diagnose and determine the direction of treatment. In uncomplicated cases, health is good. Physiological jaundice occurs in 60-70% of infants. It is also called temporary conjugation. Appears on days 3-4 (in premature infants on days 5-6) after birth without signs of anemia and hemolysis. It goes away within 7-14 days.
Conjugation jaundice develops due to the immaturity of any component of the bilirubin metabolic system. Occurs from 2 to 10 days after birth. The disease lasts from 14 to 30 days. Differential diagnosis is difficult, and symptoms may be similar to other types of jaundice. Inpatient monitoring of the young mother and baby is recommended.
Hemolytic jaundice in newborns occurs due to a history of other diseases. These may be: pulmonary infarction, liver damage, septic endocarditis, malignant tumors, malaria. Toxic effects on the body can also cause the development of this form of the disease. Diagnostics shows an increased level of stercobilin in feces and the presence of hyperbilirubinemia.
Neonatal jaundice of newborns is provoked by immaturity of liver cells, increased production of bilirubin and low ability of blood serum to bind it. If a decreasing trend in indicators is not observed, diagnostics are necessary to determine the causes. Neonatal jaundice is characterized by insufficient amounts of enzymes that are needed to neutralize excess bilirubin in the blood.
A severe form of the disease is considered to be kernicterus, which affects the brain, which is not bound by bilirubin. Symptoms develop rapidly during the first two days after birth. The baby has a mask-like facial expression, convulsions, tension in the muscles of the neck and head, and wheezing when listening. This type of jaundice in newborns has serious health consequences.
Parenchymal type is a severe form of the disease that requires immediate medical attention. It is of hepatitis origin. Obstructive jaundice is a pathological syndrome, the cause of which may be disturbances in the metabolism of metals, proteins, anatomical defects and obstruction of the bile ducts. It appears from the first days of life. Recovery is possible by the second half of the year, provided the form of the disease is uncomplicated.
The obstructive (subhepatic) form of the disease develops against the background of bile duct obstruction. There may be a history of abdominal tumors. In infants, the skin color has a greenish-yellow tint, stool is whitish, and urine is dark. Pathological jaundice in the neonatal period develops rapidly - in the first days after birth. An enlargement of the spleen and liver, and the occurrence of spontaneous bruises on the body are diagnosed. Increased hemolysis may occur if there is a history of Rh factor incompatibility between mother and baby.
Neonatal jaundice and breastfeeding
The original title of the manuscript was “Hemolytic disease”
Ekaterina Denisova PA Central Cultural Center “Rozhdenie”, Dnepropetrovsk.
Leonid Vodyanikov, neonatologist, Maternity Hospital in Asbest, Sverdlovsk Region.
Introduction
Jaundice occurs in the majority (approximately 40 to 70%) of completely healthy full-term newborns and is usually the result of natural processes occurring in the body. The yellow color of the skin is given by a special substance - bilirubin. It is found in the blood of every person and is excreted by the liver. During intrauterine life, fetal bilirubin is excreted by the mother's liver. After birth, the child’s liver is not yet able to cope with the amount of bilirubin; it gradually accumulates in the blood, and usually only on the 2nd or 3rd day this becomes noticeable by a change in the color of the child’s skin - it acquires a yellowish tint. At first, the face and chest become stained, but gradually, as the level of bilirubin increases, the jaundice seems to “descend lower” - to the buttocks and legs. Gradually intensifying, jaundice becomes most pronounced by the 4th-5th day and completely disappears by 2-3 weeks of age without any treatment (so-called physiological jaundice).
Jaundice is clearly visible in daylight if you lightly press your finger on the skin of the chest for a few seconds and then release. A slight icteric discoloration on the cheeks and chest is a phenomenon that usually does not bother doctors, but icteric discoloration of the buttocks, abdomen, and especially the legs should be alarming. If jaundice is detected on the first day or at another age of the child, when the intensity of jaundice seems unusually pronounced, the level of bilirubin in the blood is determined. To do this, they take blood from the child’s vein or use the method of measuring bilirubin using a special device that allows you to assess the level of bilirubin in the blood using a method that does not require taking blood for analysis - transcutaneous bilirubinometry.
There is an opinion in medical circles that breastfeeding can increase bilirubin levels, so when a newborn develops jaundice, breastfeeding is stopped or interrupted in some hospitals. But at the same time, it is well known that breastfeeding is indeed the very first measure to prevent jaundice in a newborn.
Let's try to figure it all out.
Breastfeeding jaundice and its prevention
There are studies that show that jaundice is slightly stronger and lasts slightly longer in those children who, compared to bottle-fed babies, are exclusively breastfed6,7. This circumstance, for the most part, affects only those who are late to the breast, receive infrequent feedings, or maternity hospital staff do not provide mothers with good assistance in establishing feeding.
Why?
A significant part of the bilirubin is excreted from the child’s body with the first stool - meconium, and colostrum, which has a mild laxative effect, helps to expel it earlier and more completely. Therefore, it has been proven that early breastfeeding is a good measure to prevent jaundice.
There are also studies that convincingly prove that frequent breastfeeding (at least 8-10 times a day), compared with rare ones, reduces the severity and duration of jaundice,
Let's try to understand why then there is such a term “breastfeeding jaundice” and what does it mean?
Prolongation of jaundice up to three weeks is a natural, physiological continuation of jaundice for breastfed children. This jaundice depends on the presence of a certain factor in breast milk, which is why it is otherwise called “breast milk jaundice.” This type of jaundice is due to the fact that under the influence of this factor, the reabsorption of bilirubin from the intestine increases.
Sometimes such jaundice prolongs and in this case, in approximately 4% of children, it is one of the causes of the so-called. “protracted jaundice” (see below). Most often, this jaundice appears only at the end of the first week (which is why it is otherwise called “late”), and in some cases it can last from 1 to 3 months. Although it is usually also completely harmless, in this case it is necessary to exclude another possible cause of the protracted course of jaundice and, if necessary, carry out treatment.
Another type of “breastfeeding jaundice” (also called “early”) was called “non-feeding breastfeeding jaundice” by Dr. Lawrence Gartner. Despite the fact that such children from birth are not given any additional types of feeding other than the mother's breast, for some reason these children still do not receive enough breast milk.
In this case, an increase in the reabsorption of bilirubin from the intestine was also noted, but this does not depend on the factor of human milk, but occurs due to insufficient energy supply to the child. This form of jaundice can be more severe, so you need to pay attention first of all to the following principles of proper breastfeeding of a newborn:
- Frequent feedings. As already noted, it has now been proven that frequent breastfeeding is a good measure for the prevention of severe forms of jaundice in newborns. A healthy newborn baby must be latched to the breast at least 8-10 times a day. As a rule, such children show a desire to breastfeed much more often. Moreover, in the first two to three days, the baby’s night feedings predominate. A baby's sucking of the breast promotes the production of the hormone “prolactin,” otherwise called the “motherhood” hormone, which prepares the breasts for milk production. The peculiarity of this hormone is that its action occurs mainly at night. Therefore, to maintain good lactation, night feedings are very useful.
- Effective sucking is a sucking process during which the baby not only sucks at the breast, but also easily sucks out all the milk that is there. Such proper feeding also serves as a measure to prevent jaundice in newborns.
It happens that the doctor and mother think that the baby is “suckling”, but in fact he is not receiving the required amount of milk. Let's look at what's going on here? Sometimes the baby is simply too weak to suckle effectively (premature or sick baby). More often, this situation occurs when a healthy full-term newborn holds only one nipple in his mouth, without grasping most of the areola (nipple circle) and does not observe grip asymmetry (the areola should be visible more from above than from below). This causes pain and cracks in the mother’s nipples.This situation is a consequence of improper attachment of the baby to the breast. Despite the apparent sucking, a child who has not latched onto the breast correctly cannot quickly receive all the milk he needs, which is available from the mother.
The most common causes of ineffective sucking are: incorrect position at the breast, uncomfortable maternal position, use of a pacifier and previous bottle feedings, feeding with a breast pad. Rarer causes depending on the child may also be important, but only a doctor can determine this.
- Water in a newborn's diet.
Breast milk is 87% water. It provides all the fluids and nutrients the baby needs for optimal growth and development of the baby. Up to six months, this is the only menu for the baby. A portion of water or glucose is perceived by the baby as food, suppresses his appetite and reduces the number of necessary feedings, which reduces breast stimulation and affects milk production. In addition, it has now been proven that water or glucose solutions do not help prevent jaundice. ,. The use of breast milk substitutes or other supplemental fluids is extremely rare in healthy newborns and only for strict medical reasons. - Availability of adequate support from medical staff and relatives. Qualified staff support includes helping the mother start breastfeeding as early as possible, teaching her how to properly attach to the breast, encouraging breastfeeding on demand, and giving the nursing mother all the necessary information about the signs of an effective milk supply to the baby. The support and participation of people around you at this time is, of course, also very important.
You need to start breastfeeding as early as possible (ideally within the first two hours after birth).
From the very first feedings, the mother needs to choose a comfortable position for feeding and learn how to properly attach to the breast. The maternity hospital should create conditions for the mother and child to stay together and encourage frequent (unlimited in duration and frequency) breastfeeding.
The mother should be given the following information:
- You need to feed your baby as often as he asks. There is no need to wait for him to scream from hunger. Signs your baby is hungry: Lip smacking
- Pulls fists into mouth
- Looking for breasts with his mouth
- Makes “calling” sounds
Mom needs to be well aware of the signs of effective breastfeeding:
- While sucking, the baby makes several slow sucking movements with a pause, during which you can hear him swallowing the milk. After feeding, the baby’s mouth is moist and the breasts seem “empty.” After feeding, the baby feels satisfied.
- The original stool is dark olive in color. If the baby receives a sufficient amount of breast milk, usually by the fourth day his stool will lighten, acquiring a soft or semi-liquid consistency. As a rule, in children who receive good breastfeeding, by the fourth day the stool becomes yellow and grainy. Its frequency is very individual for each child. Normally it may be greenish.
- In the first days, children urinate rarely (1-3 times per second), but if the child sucks out a sufficient amount of milk, then at the age of 4 days the number of wet diapers reaches 6-8 times per day. By the 3rd week, the frequency of urination is even greater (can reach 20 times per day). Urine is light, straw-yellow in color.
- If the child eats well, by the 3rd day he does not lose much weight (up to 10% of birth weight), by the 4th day he begins to restore his weight, gaining approximately 25-30 g per day, by 14 -th day or earlier - restores the original mass.
If there is a need to increase the volume of milk sucked by the baby, you can increase the number of feedings up to 12 times a day, be sure to feed several times at night, and after feeding, when the baby has already had enough from the breast, you can feed the baby a little with expressed breast milk from a spoon.
Pathological jaundice
Any jaundice may have an unusual course, therefore such jaundice is conventionally called “pathological jaundice”. It differs from the “physiological” one by its earlier appearance (already in the first day of life), longer duration (more than 3 weeks) or a very high level of bilirubin in the blood. For example, the most common reasons for the manifestation of the so-called. pathological jaundice of a newborn - incompatibility of the blood of mother and child by group (if there is the first group in the mother and the second or third in the child), or Rh factor (with a negative Rh factor in the mother and positive in the child).
There are other factors that increase the likelihood of such a course of jaundice, for example: prematurity, massive hemorrhages on the skin or head of the child, severe jaundice in previous children and some others. There are many other reasons for a serious increase in bilirubin in the blood, which must be identified in any case, so a mother who notices jaundice in a child (especially in the first day) should definitely tell the doctor about it. Such children require special attention so that treatment is started on time.
After the mother is discharged from the hospital, she should monitor her baby for jaundice and be concerned if the jaundice worsens or lasts more than 3 weeks.
Protracted jaundice is a group of pathological conditions that are manifested by prolonged persistence of increased bilirubin in the child’s blood (more than 3 weeks). Of course, innocent “jaundice from human milk” can also occur this way, but prolonged jaundice, at the same time, can cause a very serious illness and require a detailed examination of the child.
Jaundice that lasts more than three weeks requires a mandatory visit to a doctor!
In addition, the mother needs to remember that with ordinary “physiological” jaundice there is never any discoloration of the stool, and the urine never takes on a dark color. These color variations in stool and urine should always be a concern for parents and a doctor should be consulted.
If the child is jaundiced, parents should also be alarmed by the child’s unusual behavior: lethargy, drowsiness, breast refusal, poor weight gain.
Treatment
At a certain level of bilirubin, or a certain rate of increase, which depends on the age of the child and many other conditions, the attending physician can discuss with the parents the issue of starting treatment for jaundice, the purpose of which is to prevent a dangerous rise in the level of bilirubin in the blood.
The most effective and safe type of treatment, which is used for most jaundice in a newborn, is phototherapy (light therapy).
In rare cases (usually with hemolytic disease of the newborn), a replacement blood transfusion may be required.
During phototherapy, light from special blue or blue-green lamps illuminates the baby from all sides, and bilirubin located in the skin, under the influence of such light, is converted into a water-soluble form, which is easily excreted in stool and urine.
When a child undergoes phototherapy, he or she will need some additional fluid intake. This is due to the fact that prolonged exposure to light sources increases the child’s fluid loss. However, mandatory administration of water or glucose solutions during phototherapy is not currently recommended. Glucose is not a therapeutic agent for the treatment of jaundice. Additional fluid intake can be provided by increasing the volume of feedings and more frequent feedings.
Feeding for jaundice
What type of feeding is most preferable during phototherapy?
The World Health Organization states that the best form of feeding for a newborn baby is breastfeeding.
Modern manuals for the treatment of jaundice recommend that mothers breastfeed whenever possible.
For all types of “breastfeeding jaundice,” it helps if the child, provided he is suckling effectively, is offered more frequent breastfeedings (12 or more times a day), as well as prescribed some additional amount of expressed breast milk from the mother, which can be fed to the child after after he finished suckling. If it was “breastfeeding jaundice,” then within 12 hours after these measures, bilirubin usually decreases. In these cases, additional administration of formula may sometimes be necessary, but temporary cessation of breastfeeding for these jaundices is rarely required and is not mandatory.
There are other situations when the doctor needs to discuss with the parents the issue of starting to supplement the baby with breast milk substitutes. Such testimony must always be strictly substantiated. For example, these are situations associated with dehydration of a child (loss of initial weight by more than 10-12%) in which frequent breastfeeding does not help improve the situation.
It should be remembered that the doctor always takes into account the benefits of breastfeeding and the risk of introducing a breast milk substitute into the baby’s diet:
Children receiving artificial nutrition are more at risk of intestinal infections and other infectious diseases, for example: pneumonia, otitis media, etc.
- These children are more likely to develop allergic diseases
- All existing breast milk substitutes place increased stress on the digestive system of a newly born baby.
- Any substances of such substitutes are less easily absorbed.
- Artificial children are more likely to be obese.
- It is known that feeding a child with artificial substitutes instead of mother's milk is a risk factor for the child to develop diseases such as hypertension and bronchial asthma in adulthood.
Why, in some cases, when treating jaundice, are doctors forced to separate mother and child and temporarily interrupt breastfeeding?
It is known that anti-Rh antibodies in Rh conflict cause hemolysis (destruction of red blood cells - erythrocytes), and in medical circles there is a very strong opinion that the additional intake of these antibodies with mother's milk can maintain jaundice in the child.
The following traditions are based on this:
- do not feed the baby with mother's milk in the first three days
- do not feed the baby until the titer of antibodies in the mother's milk is determined.
There is currently no basis for such recommendations.
There are no studies that show the effectiveness of these measures for the prevention and treatment of hemolytic disease of the newborn.
Typically, hemolytic disease develops (even with early onset) only several hours after birth. Until the first signs of illness appear (jaundiced discoloration of the skin), if the child is otherwise healthy, nothing prevents him from communicating with his mother and suckling the breast within the first hour after birth (like all other healthy full-term children). It is very important that colostrum is the baby’s first food (it is a transitional food from the amniotrophic method of feeding (when the fetus swallows amniotic fluid) to breastfeeding, since the baby’s kidneys are not yet able to pass large volumes of fluid. It is also known that colostrum is rich in vitamin A and immunoglobulins , growth factors and has a laxative effect.
During phototherapy there are no contraindications to breastfeeding, but there are some difficulties.
For example, the difficulty is that sometimes the baby must be exposed to a special therapeutic light continuously (in very severe cases this helps to avoid a replacement blood transfusion) and therefore the mother does not always have the opportunity to hold the baby in her arms.
In some cases, methods are used to breastfeed the baby:
- If bilirubin levels are not very high, the phototherapy unit can be placed in a shared ward. In this case, the mother has more opportunities to feed the baby on demand.
- A special fiber-optic device for light therapy (luminous blanket) is used, which allows phototherapy to be carried out even during feeding.
If it is not possible to stop phototherapy for feeding, the baby can in any case be fed the mother's expressed milk from a spoon or small cup. In some hospitals, a syringe without a needle is used for this purpose, with which milk is instilled directly into the baby's mouth.
If the baby has received a replacement blood transfusion, at first he requires special monitoring, but soon he can be fed breast milk and combined with his mother, if phototherapy is installed in a shared ward.
What can a mother do in a situation where a child requires treatment for jaundice?
- discuss this situation with your doctor
- express your desire to breastfeed your baby
- share concerns about formula feeding
- justify the need and possibility of breastfeeding, referring to WHO recommendations
- insist that whenever possible the baby is allowed to be breastfed as often as he requests, and if this is not possible (for example, some children become drowsy during phototherapy or phototherapy cannot be interrupted) - ensure that the mother can feed her baby with expressed milk without using bottles.
- if the child is in the intensive care unit, ask the doctor for permission to visit the baby often and touch him. During visits, talk to him, calm him down, ask him to hold him in your arms between treatments, you can also ask the medical staff not to use a bottle or pacifier when caring for her child.
- If a mother is temporarily separated from her baby or does not have the opportunity to breastfeed, then to enhance lactation she must pump at least once every 3 hours (each breast for about 20 minutes). A night break of 4-5 hours is allowed, but it is better to express your breasts at night, because... this allows more milk to be produced.
What can a doctor do in a situation where a child needs treatment for jaundice?
- Discuss the current situation with your mother.
- Listen to her questions, support her desire to breastfeed.
- Reassure the nursing mother that her baby’s jaundice is treatable and since it has already been treated, it will not cause any harm to the baby. Tell her that the methods of examination and treatment of her child used in the maternity hospital are the safest and most effective currently known and how to make them even safer.
- Assure the mother that even if for some reason the baby cannot be put to the breast for some time, she can continue to give him her breast milk.
- Reassure the mother that if the baby has to be given formula for a while, even a small amount of breast milk will be beneficial!
- Assure the mother that she can successfully breastfeed the baby, well, as a last resort, for some time she will also have to give the baby her expressed breast milk.
- Reassure her that for this, the hospital uses only proven, safe methods of alternative feeding of the baby with expressed milk (for example, a spoon, or better yet, a cup, and does not use other feeding methods that could later prevent the mother from calmly continuing breastfeeding).
- If the child is in the intensive care unit, assure the mother that she will be allowed to visit the baby often and communicate with him without restrictions, as she wants, and even pick him up, and even try to put him to the breast (under the supervision of staff, of course)
At this time, it is difficult for the mother to remain calm and be confident, but all her fears about the child’s jaundice are usually greatly exaggerated. A mother should believe that such a short-term episode in her child’s life as treatment for jaundice will not prevent her from maintaining her lactation and resuming feeding if it was briefly interrupted.
Literature:
- James Acre Feeding children in the first year of life: physiological basis // scientific journal, WHO Bulletin, supplement, T 67. Geneva. 1989
- “Basics of newborn care and breastfeeding” in 3 parts, Regional Office for Europe of the World Health Organization, Maternal and Child Health, Family Planning, 1997
- de Carvalho M, Klaus MH, Merkatz RB, Frequency of breastfeeding and serum bilirubin concentration. Arch Dis Child, 1982. 136: p. 737-738.
- Evidence-Based Guidelines for Breastfeeding Management during the First Fourteen Days, International Lactation Consultant Association, April, 1999
- Gartner LM. Breastfeeding and jaundice. J Perinatol 2001 Dec;21
- Giovanna Bertini, MD, Carlo Dani, MD, Michele Tronchin, PhD, and Firmino F. Rubaltelli, MDIs Breastfeeding Really Favoring Early Neonatal Jaundice? PEDIATRICS Vol. 107 No. 3 March 2001, p. e41
- Maisels MJ, Newman TB. Kernicterus in otherwise healthy, breast-fed term newborns.Pediatrics. 1995;96:730 -733
- Management of Hyperbilirubinemia in the Newborn Infant 35 or More Weeks of Gestation Subcommittee on Hyperbilirubinemia PEDIATRICS Vol. 114 No. 1 July 2004, pp.297-316
- McDonagh AF, Lightner DA. 'Like a shrivelled blood orange'-bilirubin, jaundice, and phototherapy. Pediatrics. 1985;75:443 -455
- Timothy Ramer, MD Breast Milk Jaundice eMedicine
- Yamauchi Y, Yamanouchi I, Breastfeeding frequency during the first 24 hours after birth in full-term neonates. Pediatr, 1990. 86: p. 171-175.
- Yetman RJ, Parks DK, Huseby V, Mistry K, Garcia J. Rebound bilirubin levels in infants receiving phototherapy. J Pediatr. 1998;133:705 -707