Cardiac syndrome X: issues of differential diagnosis and therapy
The problem of pain in the left half of the chest, or cardialgia syndrome, constantly attracts the attention of doctors: approaches to assessing these pains are being improved, and differential series are being replenished (see table). But it was never possible to finally resolve this problem. This topic may be considered particularly relevant due to the high risk of association of cardialgia with acute diseases and conditions that can lead to death. General practitioners are often forced to be the first to resolve issues of diagnosis, differential diagnosis and tactics in relation to individuals with pain in the precordial region.
In recent years, in the medical literature, more and more attention has been paid to a relatively new pathological condition, which undoubtedly belongs to the category of cardialgia - syndrome X. To designate this condition, Russian and foreign language synonyms are used: cardialgic (cardiac) syndrome X (syndrome X), angina pectoris with damage to vessels of small diameter, small vessel disease, Gorlin-Licoff syndrome, microvascular disease, etc. We believe that the most common and consistent with the modern view of this problem can be considered the definition of “cardiac syndrome” X" [1]. We will use this term in the future, since it indicates the main clinical syndrome of the disease - pain in the left half of the chest, and also reflects the complexity of understanding the etiopathogenetic mechanisms of this pathology.
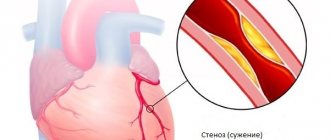
Cardiac syndrome X (CSX) is a pathological condition characterized by the presence of signs of myocardial ischemia (typical attacks of angina and depression of the ST segment ≥1.5 mm (0.15 mV) lasting more than 1 minute, established during 48-hour ECG monitoring) against the background absence of atherosclerosis of the coronary arteries and spasm of the epicardial coronary arteries during coronary angiography.
The identification of CSC occurred due to the development and improvement of modern diagnostic methods. The first description of a patient with long-term angina pectoris, in whom absolutely normal coronary arteries were discovered at autopsy, belongs to W. Osler and dates back to 1910; later this phenomenon was not mentioned. Only in 1967 were unique reports of two patients with coronary arteries unchanged during coronary angiography and chest pain; by 1973, Kemp had collected data on 200 such patients [2]. From this group, a part of the patients were selected in whom it was possible to prove the presence of signs of ischemia (lactate production during pain, ischemic changes in the ST segment during stress tests). In connection with the existing objective signs, there is currently no doubt about the presence of this pathological condition, but there is also no single, balanced opinion about the causes of its occurrence and the pathogenetic signs that unite patients suffering from this disease.
Sketches of pathogenesis. According to modern concepts, the development of CSC is based on defective endothelin-dependent vasodilation of small myocardial arteries. In other words, during physical activity, the myocardial oxygen demand increases sharply, which normally leads to expansion of the vascular bed of the heart muscle, whereas this does not happen with cardiopulmonary syndrome. For some unclear reasons, small arterial vessels lose their ability to dilate, which, against the backdrop of an ever-increasing level of physical activity, provokes the occurrence of angina pain.
The occurrence of defective vasodilation may be due to the following reasons [1]:
- A decrease in the production of brain natriuretic peptide (brain-BNP), a biologically active substance that is produced by the myocardium and has a local vasodilating effect (this assumption is somewhat contradicted by the fact that a number of researchers find defective vasodilation not only in the myocardial vessels, but also in the vessels of the forearm, then there is a widespread process).
- Reduced production of adrenomedullin, a vasoactive peptide produced by cells of the adrenal medulla and endothelial cells, which reduces the proliferation activity of smooth myocytes and prevents the development of hypertrophy of the vascular wall. According to histological studies, in the cardiac muscle during CSC, phenomena of proliferation of smooth muscle cells in the medial layer of small arteries are detected.
- Excessive formation of endothelin - a non-stanoid substance that is produced by endothelial cells (under the influence of stress, hypoxia, angiotensin-II, serotonin, damage to the intima of the vessel) and promotes the proliferation of vascular smooth myocytes, which can also cause the above-described morphological changes. In addition, endothelin increases the concentration of intracellular calcium, and the effectiveness of calcium antagonists in CSC can be considered proven.
- Tissue insulin resistance, leading to impaired glucose utilization by the myocardium and disorders of the endothelium of epicardial vessels [3, 4].
Another very important pathogenetic point is the decrease in the pain perception threshold in most patients with CSC; such patients are more sensitive to nociceptive stimuli. It is noted that even minor ischemia can lead to severe clinical manifestations of angina pectoris. The cause of pain is considered to be impaired autonomic control by the autonomic nervous system.
Disorders of adenosine metabolism may also play a key role in the pathogenesis of the disease. When this substance accumulates in excess, it can cause ischemic ST shift and increased sensitivity to painful stimuli. This is supported by the positive effect on aminophylline therapy.
Summarizing the above, it can be noted that the main factors determining the development of chest pain in this pathology are defective endothelin-dependent vasodilation and a decrease in the pain perception threshold (Fig. 1).
| Figure 1. Scheme of the main links in the pathogenesis of cardialgia syndrome X |
Clinical aspects. Among patients with CSC, middle-aged people predominate, the sex ratio is 1:1 with a slight predominance of women. The main complaint includes episodes of angina-type chest pain that occurs during physical activity or is provoked by cold or emotional stress; with typical irradiation, in some cases the pain is longer lasting than with ischemic heart disease, and is not always relieved by taking nitroglycerin (in most patients the drug worsens the condition).
During instrumental examination, a significant proportion of patients are found to have incoming or persistent conduction disturbances (like left bundle branch block). A resting ECG during an attack of chest pain, exercise testing, and 48-hour Holter monitoring reveals signs of ischemic ST segment depression exceeding 1.5 mm in amplitude and 1 min in time. The daily profile of ischemic episodes shows their high frequency in the morning and afternoon; at night and early in the morning ischemia is rare (as in patients with coronary artery disease). Myocardial stress scintigraphy with 201Tl shows typical ischemic focal disorders of drug accumulation.
Laboratory tests reveal accumulation of myocardial lactate during an attack. When performing a dipyridamole test, patients do not experience an increase in coronary blood flow at the level of small coronary vessels; clinically this is manifested by an increase in the severity of ischemia and the appearance of chest pain. The ergometrine test is positive, and when assessing cardiac output, a decrease is noted during the administration of the drug.
Today, the following diagnostic criteria stand out [1, 2, 5]:
- typical chest pain and significant ST segment depression during physical activity (including on the treadmill and bicycle ergometer);
- transient ischemic depression of the ST segment ≥1.5 mm (0.15 mV) lasting more than 1 minute during 48-hour ECG monitoring;
- positive dipyridamole test;
- positive ergometrine (ergotavin) test, decreased cardiac output against its background;
- absence of atherosclerosis of the coronary arteries during coronary angiography;
- increased lactate content during ischemia when analyzing blood from the coronary sinus area;
- ischemic disorders during stress myocardial scintigraphy with 201Tl.
Differential diagnosis. When a patient with cardialgia first visits, the question always arises about the differential diagnosis of this condition. At this stage, it is important to correctly question the patient, find out the characteristics of the pain syndrome and analyze, first of all, how much they correspond to the typical manifestations of angina pectoris.
When collecting anamnesis, you should pay attention to the age and gender of the patient, the presence of risk factors and occupational hazards. Significant assistance can be provided by available medical documentation indicating concomitant pathology (heart disease, long-term anemia, thyrotoxicosis, chronic lung diseases, etc.), which can simulate clinical angina. An objective examination reveals signs characteristic of diseases simulating angina pectoris: enlargement of the thyroid gland, pain on palpation of the thoracic spine, intercostal spaces, shoulder joint, changes in respiratory sounds, tachycardia, arrhythmia, murmurs in the heart area. Even if, based on a conversation with the patient, studying medical documentation and objective research, you are convinced that cardialgia is not associated with ischemic heart disease or coronary syndrome, but with some other reason, you should not neglect additional examinations that may refute your data.
The patient's additional examination plan should include:
- general blood test (excluding anemia, inflammatory changes that may be associated with a latent infection, signs of active rheumatological disease);
- lipid spectrum (determining the likelihood of atherosclerosis);
- fasting glucose level and/or, if necessary, glucose tolerance test (excluding diabetes mellitus as a risk factor for coronary artery disease);
- acute phase indicators (C-reactive protein, sialic acids, seromucoid, fibrinogen), rheumatoid factor - to exclude rheumatological pathology;
- UMSS or Wasserman reaction (to exclude syphilis);
- standard ECG and/or stress tests, Holter monitoring;
- chest x-ray (heart size, pulmonary fields), which allows to exclude the presence of pneumonia, tuberculosis in the lungs, pleural overlays;
- if there are signs indicating the possibility of detecting osteochondrosis or other pathology of the spine - radiography of the thoracic and cervical spine in direct and lateral projections, functional tests;
- EchoCG - in the presence of cardiac murmurs, changes in heart size during topographic percussion or according to radiography;
- FGDS - in the presence of complaints from the digestive system and at the same time burning pain in the chest (to exclude gastroesophageal reflux disease);
- Ultrasound of the abdominal organs - to exclude radiating pain caused by cholecystitis, pancreatitis, etc.;
- coronary angiography - performed in patients in whom atherosclerotic lesions of the coronary arteries cannot be definitively excluded.
The listed studies in most cases make it possible to more accurately differentiate the diseases included in the “pain syndrome in the left half of the chest”; in this case, studies can be carried out according to the algorithm of optimal diagnostic feasibility. In other words, based on data from subjective and objective examination methods, a plan for further research should be drawn up (taking into account economic costs and reducing diagnostic time).
As a guide, we can suggest the algorithm presented in Fig. 2. The task of the diagnostic search in this case is to separate cardiac and extracardiac causes of pain; The starting method of diagnosis is electrocardiography (routine, stress tests or Holter monitoring), which is available in most medical institutions and is easy to use and inexpensive. The detection of any (!) changes on the ECG in more than 90-95% of cases is alarming in terms of the cardiac genesis of the pain syndrome (although it is worth remembering the possibility of a combination of cardiac and extracardiac causes), and their absence convinces us of the opposite. Next, it is necessary to divide patients by age and sex, and then analyze the most likely cardialgia in a particular age and sex group and methods for verifying the diagnosis. An epidemiological approach taking into account age and gender factors significantly reduces the cost and speeds up the procedure for additional research.
To clarify the extracardiac cause of pain, it is necessary to search for an additional syndrome, which is carried out on the basis of the patient’s complaints, medical history, and a minimal physical examination. After clarifying the syndrome (pathology of the digestive, respiratory, musculoskeletal system, etc.), the circle of diagnostic search will narrow further.
Thus, in the differential diagnosis of cardialgia, a conversation with the patient, physical examination, electrocardiography (routine and monitoring and/or stress), and identification of leading syndromes using the principle of optimal diagnostic feasibility should be considered as the main methods. Epidemiological factors (gender, age, smoking) are important.
Issues of therapeutic tactics in patients with cardialgia syndrome X have not been fully worked out, but taking into account the data available in the literature, it is worth placing some fundamental emphasis. Depending on the situation, it is necessary to carry out therapy in order to relieve pain in the heart area or prevent it.
In case of an attack of angina pectoris against the background of CSC, the patient is prescribed a β-blocker under the tongue (anaprilin in a dose of 20-40 mg), a Ca++ antagonist (nifedipine 5-10 mg) or 5-15 ml of a 2.4% solution of aminophylline (aminophylline) is administered intravenously. for 15 minutes [5]. It is better to refrain from taking nitrates.
To prevent the occurrence of pain in the heart area, the use of long-acting theophylline preparations (teopeca, theodura, theotard, etc.) is discussed, this is especially indicated for patients with the absence of tachycardia, concomitant obstructive pathology of the respiratory tract (bronchial asthma, chronic obstructive bronchitis); If there is a tendency towards arterial hypertension, long-acting nifedipine or amlodipine may be the drugs of choice. Psychocorrectors (usually antidepressants, in particular imipramine) [6] and antiplatelet agents are also used.
The prognosis for syndrome X is generally favorable and the risk of mortality, despite the clear clinical symptoms, is extremely low. However, with a favorable overall prognosis, patients with CSC are characterized by a low quality of life, which is due to limited physical activity and severe pain. There was a tendency for the disease to transform into dilated cardiomyopathy (especially in the presence of left bundle branch block according to ECG), into typical ischemic heart disease.
Cardiac syndrome X is a disease that is very difficult to identify; it can be considered rather as a diagnosis of exclusion; therefore, it is especially important to be able to differentiate it.
Literature
- Kalyagin A. N. Cardialgic X-syndrome // Siberian Med. magazine. 2001. T. 25. No. 2. P. 9-14.
- Kostyuk F. F. X-syndrome // Cardiology. 1992. Issue. 32. No. 1. P. 80-82.
- Kudryavtsev S. A. Features of the pathogenesis, clinical picture and non-invasive diagnosis of coronary heart disease with angiographically unchanged coronary arteries: Abstract of thesis. ...cand. honey. Sciences, 1998.
- Maychuk E. Yu., Martynov A. I., Vinogradova N. N., Makarova I. A. Syndrome X // Klin. medicine. 1997. No. 3. P. 4-7.
- Ioseliani D. G., Klyuchnikov I. V., Smirnov M. Yu. Syndrome X (issues of definition, clinic, diagnosis, prognosis, treatment) // Cardiology. 1993. Vol. 33. No. 3. P. 80-85.
- Metelitsa V.I. New in the treatment of chronic coronary heart disease. M.: Insight, 1999. 212 p.
A. N. Kalyagin, Irkutsk State Medical University, Irkutsk
Causes of gastrocardial syndrome
The most common causes of gastrocardial syndrome:
- systematic overeating;
- high diaphragm position;
- increased sensitivity of receptors in the mucous membranes of the stomach and esophagus;
- stretching of the cardiac mucosa;
- flatulence;
- neoplasms or ulcers of the cardiac part of the digestive system (esophagus, stomach);
- atherosclerosis of the coronary arteries;
- frequent stress.
An overfilled stomach provokes excessive irritation of the vagus nerve, which intensifies symptoms.
Prevention
To prevent recurrence of attacks and exacerbation of the condition, you need to:
- monitor the amount of food, do not overeat;
- switch to proper nutrition in accordance with doctor’s recommendations;
- avoid irritation of the gastric mucosa;
- cure concomitant pathologies;
- if necessary, undergo a course of psychotherapeutic treatment;
- regularly give the body moderate physical activity;
- prevent constipation;
- try to reduce body weight if it is excessive;
- prevent conditions in which reflux occurs - food from the stomach enters the esophagus (for example, it is not recommended to bend over immediately after eating).
Treatment of gastrocardial syndrome
For patients diagnosed with gastrocardial syndrome, treatment is selected by a cardiologist and gastroenterologist. The treatment regimen includes:
- taking antispasmodics half an hour before meals;
- fractional meals in small portions;
- taking sedatives, tranquilizers, sedatives of herbal origin;
- limiting the one-time volume of liquid consumed (while the daily norm remains the same).
During treatment and throughout life, it is important for patients to monitor the activity of the intestines and avoid constipation. In addition to fractional meals, the diet should be reviewed. Excluded:
- foods that irritate the mucous membrane (salted, smoked, sour foods);
- fatty, rough foods;
- foods that cause increased gas formation (cabbage, legumes).
The prognosis of therapy is positive in most cases. In severe cases, endoscopic intervention may be performed.