P-LCR is a laboratory criterion that reflects the proportion of giant platelet cells in the blood, measured in %, and is normally 13-43%
, regardless of the age and gender of the patient. To determine the index, a special clinical blood test is performed. With this you can find out the number of platelets that regulate blood clotting, their maturity, size and functional activity. Other equally widespread indices are mean platelet volume (MPV) and relative platelet volume distribution width (PDW).
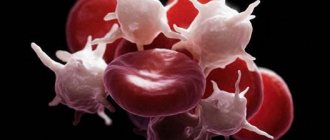
a – normal platelets (against the background of erythrocytes) b – platelets of different volumes (anisocytosis) c – huge macroplatelets (P-LCR increased)
Deviation of P-LCR from the norm is associated with the presence of pathology in the body. The main function of platelets is thrombus formation: the cells form a blood clot, which closes damage to the vascular wall and prevents massive blood loss. When their amount in the blood decreases, the risk of bleeding increases. With a high concentration of platelets, there is a tendency to thrombosis and their severe consequences.
After receiving the results of a general blood test and if the patient has characteristic complaints, specialists conduct a detailed study aimed at determining P-LCR. This diagnostic test is ordered when it is necessary to carefully examine the morphology of platelet cells and count the number of excessively large elements.
Laboratory doctors who performed an extensive blood test evaluate the results and make an appropriate conclusion, on the basis of which clinicians make a final diagnosis. Deviations are usually observed in individuals with recurrent somatic diseases or hereditary anomalies.
examples of diagrams of platelet content in the blood - 1) normal, 2) with a decrease in the total number of platelets and P-LCR, including, 3) with an increase in % P-LCR - the presence of a large number of giant platelets
To determine the large platelet ratio, it is necessary to donate venous blood for analysis. The biomaterial is collected directly in the laboratory. The study is performed immediately. The sooner it is started, the more accurately many indices will be determined. It is necessary to prepare for the analysis: the day before you cannot smoke, drink alcohol, drink coffee and tea, or take medications. Nicotine, ethanol, caffeine and drug components often distort the results. Immediately before donating blood, it is forbidden to eat or drink. A day later, the patient receives a form indicating the result of the study, as well as reference values. The specialist interpreting the analysis must take into account all factors affecting the body and changing the number of large platelets. A P-LCR value in the range of 13-43% is considered normal. If a deviation is detected, an additional examination of the patient is carried out to identify the cause of the problem.
Basic functions of platelets
In appearance, platelets are round or oval red plates with a smooth surface. They are formed in the bone marrow. They mature in approximately 8 days. These components constantly circulate in the bloodstream.
The main function of platelets is to ensure blood clotting. In addition, the ability of these blood components to stop bleeding is important. This is ensured by the fact that individual platelets can stick together and stick to sites of vascular damage. The process is automatically started by the human body when there is a risk of bleeding.
An important question is how long platelets live. Their viability time lasts approximately 10 days. Depending on the age of the red plates, their size changes: from 2 to 5 microns in diameter.
The process of platelet renewal in the blood occurs constantly. Therefore, an important factor to ensure the maintenance of blood condition is the balance between the formation of red plates and their death. Otherwise, there may be a tendency to blood clots or increased bleeding.
Symptoms
Hereditary thrombocytosis and reactive thrombocytosis most often occur asymptomatically and are not characterized by microcirculatory disorders, as with primary thrombocytosis. Half of the patients with essential thrombocytosis are also asymptomatic, and only a blood test reveals this disease. In other patients, symptoms of vascular thrombosis and hemorrhage come to the fore. At the initial stage of the disease, the tumor mass gradually increases, and during the first years thrombosis and thromboembolism develop, and in the elderly this occurs against the background of atherosclerosis and cardiovascular pathology. Factors that contribute to the development of thrombosis:
- thrombocytosis, leukocytosis, activation of blood coagulation, functional abnormalities in platelets, presence of mutation; age, history of thrombosis, risk of cardiovascular complications.
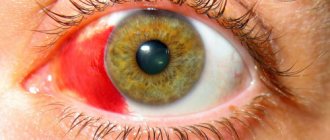
Microcirculation disorders are manifested by acrocyanosis, pain, burning sensations in the fingers, Raynaud's syndrome (cold extremities). Disturbances in the blood supply to the brain are manifested by blurred vision, periodic lameness or gait disturbance, transient ischemic attacks, impaired speech and clarity of consciousness, headaches or migraines, and dizziness. Thrombosis of the retina and hemorrhages into the vitreous body develop. Neurological manifestations are associated with microthrombosis. Sometimes, on the contrary, the disease begins with hemorrhagic syndrome - bleeding from minor injuries. In 50% of patients the spleen is enlarged, and in 20% the liver is enlarged.
Blood test for platelets
A complete blood test can determine the platelet count. The main indications for its implementation are the following:
- Increased bleeding of gums.
- Heavy menstruation.
- The appearance of bruises from minor impacts.
- Frequent nosebleeds.
- Difficulty stopping bleeding from minor injuries.
The number of platelets in the blood is measured in thousands per 1 microliter of blood. Counting is carried out in specialized laboratories in various ways that guarantee high accuracy.
The normal platelet count in the blood depends on gender and age and is:
- For men, 200–400 thousand.
- In women, 180–320 thousand, during menstruation the amount can decrease to 75–220 thousand, and during pregnancy to 100–310 thousand.
- In children, indicators depend on age, and the corresponding values are given in special tables.
To conduct a general blood test, blood is taken from a finger. No special preliminary preparation is required before this. To ensure accurate results, it is better to donate blood in the morning on an empty stomach. At the same time, 12 hours before the procedure it is not recommended to consume fatty spicy foods, carbonated drinks, and alcohol.
Additionally, to determine blood clotting indicators, Sukharev and Lee-White tests are performed. They are informative and allow you to obtain the necessary additional data about the pathological condition. This will allow you to carry out correct treatment measures and avoid dangerous consequences.
Preparing for the study
Before taking the OAC, you should stop drinking alcoholic beverages, fatty, spicy, excessively salty and fried foods the day before the procedure. Blood is donated on an empty stomach, the patient is advised to maintain physical and emotional peace (refrain from sudden movements, climbing stairs, avoid stressful situations) for half an hour before the test. Also, platelet testing is not recommended immediately after recovery from a long-term illness, which may distort the results due to weakened immunity.
Detailed instructions for preparing for a general blood test are here.
Increased platelet levels
Elevated platelets are a pathological condition. It is called thrombocytosis. The main danger of the pathology is the increased risk of blood clots.
The cause of an increase in the level of platelets in the blood can be various diseases. Most often thrombocytosis occurs against the background of:
- Malignant neoplasms.
- Infectious diseases.
- Helminthic infestations.
- Surgical operations.
- Autoimmune pathologies.
- Kidney failure.
High levels of platelets in the blood are observed in older people. Temporarily, indicators may increase after heavy physical exertion, for example, after playing sports.
The symptoms of thrombocytosis are characteristic, but mild. It is imperative to conduct a general blood test if the following symptoms are noted:
- Pain in the fingers and toes.
- Itching of skin surfaces.
- Unreasonable weakness, which leads to decreased performance.
- Lack of appetite.
Platelets are increased (thrombocytosis)
An increase in platelet count (thrombocytosis) is observed when:
- excessive physical stress
- chronic inflammatory processes (rheumatoid arthritis, tuberculosis, sarcoidosis);
- myeloproliferative diseases (primary erythrosis, chronic myeloid leukemia, myelofibrosis, myelosclerosis);
- some hemolytic anemias;
- hemolysis or severe blood loss;
- carcinoma, lymphoma;
- after removal of the spleen.
Sources:
- Eugenio D. Hottz. Platelets in Immune Response to Virus and Immunopathology of Viral Infections. — Front Med (Lausanne). Apr 2018.
- Data from the independent laboratory Invitro.
- Data from Helix laboratory.
- Steven Kim, MD. Acquired Platelet Function Disorder. — Healthline, Jan 2021
- Douglas B. Cines. Thrombocytopenia in pregnancy. - Blood. 2017 Nov 23; 130(21): 2271–2277
- Danilova L.A., Doctor of Medical Sciences, Prof. Analyzes of human blood, urine and other biological fluids at different age periods, SpetsLit, 2014.
Decreased platelet levels
Low platelet levels, the norm of which differs between men and women, provoke the development of a condition known as thrombocytopenia. Very often it occurs against the background of uncontrolled use of medications: antidepressants and antibiotics.
The reasons for a decrease in the level of platelets in the blood can be various infectious diseases: ARVI, hepatitis, herpes, etc. Thrombocytopenia can be observed when a large number of blood thinning products are included in the diet. These are ginger, cherries, garlic, onions, etc.
Non-infectious factors that reduce the level of platelets in the blood include pregnancy, vitamin deficiency, alcohol or heavy metal poisoning.
Thrombocytopenia can be suspected based on the following signs:
- Heavy menstruation.
- Frequent nosebleeds.
- The appearance of hematomas.
With a constant pathological decrease in the level of platelets in the blood, the risks of developing severe bleeding and stroke conditions, which are life-threatening, increase.
Pathogenesis
The main hypothesis for the development of essential thrombocytosis is a hereditary predisposition, which is transformed into a disease under the influence of factors that damage the genome. As a result, malignant degeneration occurs. Hereditary predisposition is associated with carriage of the JAK2 gene and activation of a certain signaling pathway that regulates cell growth. This is a signal transduction pathway from thrombopoietin and erythropoietin by JAK2 kinase, which causes myeloid lineage hyperplasia and explains the pathogenesis of myeloproliferative diseases. The JAK kinase family includes the following proteins: JAK1, TYK2, JAK2, JAK3. 4-8% of patients with primary thrombocytosis have mutations in the MPL gene, which encodes the receptor for thrombopoietin, which is a factor in the growth and development of megakaryocytes .
Reactive thrombocytosis is associated with increased production of thrombopoietic factors that activate megakaryocyte precursors or mature megaryocytes. Interleukin-6 plays the main role in stimulating thrombocytopoiesis. Reactive thrombocytosis has a transient form (for example, during trauma, surgery, acute bleeding) or a long-term persistent form (with malignant tumors, iron deficiency anemia, chronic infectious and inflammatory processes).
Restoring platelet levels in the blood
You can normalize the level of platelets in the blood with a balanced diet. It is important to saturate your diet with foods high in materials and microelements. You need to give up spicy food, alcohol, fast food and sweet carbonated drinks, lead a healthy lifestyle and maintain a drinking regime.
If it is not possible to normalize the indicators using natural methods, then you need to undergo a full examination by a hematologist. If platelet levels are elevated, special medications may be prescribed - anticoagulants or antiplatelet agents. They thin the blood and minimize the risk of blood clots. But at the same time, they should be taken only as prescribed by a doctor. It should be understood that stabilization of the condition is possible only after eliminating the underlying causes that provoke deviations from the norm.
Deviation from the norm is not always a disease
If the level of red blood cells during the first analysis is slightly outside the normal range, do not panic.
Your doctor will help you interpret the results correctly, taking into account your individual characteristics and medical history. A single slightly elevated or slightly decreased result may have no medical significance. There are several factors that can cause a test result to fall outside the established reference range without pathological reasons:
- Under the influence of external factors (stress, previous infections, physical activity), the results of the analysis of the same person may differ slightly. In this case, a person can be healthy. If the analysis shows a slight deviation, retake the test on another day.
- Individual characteristics. For some people, the boundaries of the norm may differ slightly from generally accepted ones. Reference values are valid for the vast majority of people, but we are all different, and in some rare cases, a healthy person may have their own norms, slightly different from the usual values.
Only a doctor can accurately determine this after conducting additional research.
Platelet count according to Fonio
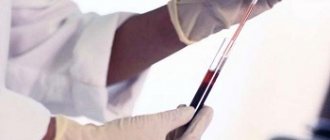
When counting platelets, the laboratory technician uses several types of reagents. This is sodium ethylenediaminetetraacetate or magnesium sulfate. Reagents are taken using the SEE meter pipette.
The analysis is carried out in several stages:
- One of the reagents and blood are added to the test tube using a pipette. The amount of reagent is taken to the 75 mark, the blood volume to the K mark.
- The resulting mass is mixed well and used to make smears.
- If magnesium sulfate is used, the smear is stained using the Romanovsky-Giemsa method for 120 minutes and 45 minutes if the laboratory technician takes sodium ethylenediaminetetraacetate. In this case, the platelets turn purple-pink.
Platelet counts are performed through a microscope
Using a microscope, platelets and red blood cells are counted up to a thousand red blood cells. To find out the number of platelets, they are multiplied by the number of red blood cells in 1 microliter, and then the resulting figure is divided by a thousand. The specific color of the cells being studied helps to obtain the most reliable results. That is why many specialists use the Fonio platelet count method when making a diagnosis.
Consequences and complications
The most common complications are:
- Thrombosis and thromboembolism . Increased platelet aggregation significantly increases the risk of venous and arterial thrombosis and cerebral ischemia . In malignant tumors, the number of venous thromboses increases significantly when compared with other types of secondary thrombocytosis. In essential thrombocythemia, thrombosis is the second cause of mortality (in first place is transformation into acute leukemia). It is noted that in 60-70% of cases these are arterial thromboses . Patients develop myocardial and cerebral infarction and peripheral occlusions. In the case of venous thrombosis, the veins of the lungs, extremities and abdominal cavity are involved.
- Blast transformation. Prolonged growth of the tumor clone causes additional mutations and a higher degree of malignancy. The consequence of this is blast transformation and the development of blast crisis, which is regarded as the terminal stage of the disease. Progression to blast transformation occurs in 1-2% of patients within 10 years of the disease; with a longer course (20 years), this percentage increases and is already 5-8. The diagnostic criterion for blast crisis is the appearance of more than 20% blast cells in the blood or bone marrow. Risk factors are: a decrease in hemoglobin less than 110 g/l and thrombocytosis more than 1000 x 10 in 9/l. It is believed that the development of a blast crisis can be provoked by cytoreductive therapy, in particular the chemotherapy drugs busulfan and hydroxycarbamide . The duration of treatment with them does not have a significant effect on this process.
- Development of postthrombocythaemic myelofibrosis . The transition to postthrombocythaemic myelofibrosis is observed in 4-10% of patients in the first 10 years, and with a disease duration of more than 10 years - in 30%. Erythroblasts, young neutrophil granulocytes are found in the blood, the liver and spleen are enlarged, and tumor intoxication appears (fever, weight loss, night sweats). Changes in the bone marrow in the form of fibrosis significantly worsen hematopoiesis and cause the development of cytopenias (inhibition of all hematopoietic germs. Therefore, with the development of myelofibrosis, symptoms appear: bleeding due to thrombocytopenia (decreased platelet levels), anemia associated with inhibition of the erythrocyte germ and various infectious complications due to leukopenia Spontaneous bleeding from dilated veins of the esophagus is life-threatening.Due to the enlargement of the liver and spleen, the pressure in the portal vein increases and portal hypertension develops.
Forecast
In most cases, the course of essential thrombocythemia is indolent (sluggish), with long intervals without any manifestations, which is periodically interrupted by thrombosis or hemorrhagic manifestations. With this course, the life expectancy for essential thrombocythemia is 10-15 years. The main cause of disability and decreased life expectancy is the occurrence of thrombosis and thromboembolism . The duration of the disease increases the risk of these complications. Only in some patients, with a long course of the disease, can an outcome occur in secondary bone marrow fibrosis, which was mentioned above, or the transition to acute myeloid leukemia.
With the development of blast transformation, the prognosis is unfavorable and survival is estimated at several months. In patients with normal general status, chemotherapy is attempted according to the protocols for the treatment of acute leukemia . However, it brings an effect only in some patients and this effect is temporary. When the effect of chemotherapy is achieved, allo-bone marrow transplantation is sometimes performed to increase life expectancy.
List of sources
- Moroz G.I. Reactive thrombocytosis in children / Health of Ukraine. — 2015, No. 3, p. 63.
- Gluzman D.F., Sklyarenko L.M., Nadgornaya V.A., Ivanovskaya T.S. Modern laboratory diagnosis of myeloproliferative neoplasms / Health of Ukraine 2011 No. 1-2 p.30-31.
- Clinical hematology: a guide for doctors / ed. A.N. Bogdanov and V.I. Mazurova. – St. Petersburg: Foliant Publishing House LLC. – 2008. – 488 p.
- Abdulkadyrov K.M., Martynkevich I.S., Shuvaev V.A. Modern approaches to the diagnosis and treatment of essential thrombocythemia: a review of the literature and our own data/Clinical oncohematology. Basic research and clinical practice.—2015, pp. 235-246.
- Bogdanov A.N., Tyrenko V.V., Noskov Y.A., Semelev V.N. /Differential diagnosis of thrombocytosis in clinical practice/Bulletin of the Russian Military Medical Academy - 2014.-2(46), pp. 44-49.
Advantages of the technique
The Fonio method of counting red blood cells has been successfully used by many doctors for many years. The technique has a number of advantages, including:
- when examining blood under a microscope, the laboratory technician clearly sees the material being examined, color, shape, number of cells;
- if necessary, analysis can be carried out at any time of the day;
- the method is easy to use, which is associated with a simple formula, but at the same time very informative.
Important! Despite the fact that medicine does not stand still and today there are new methods for counting blood particles, Fonio’s method is not inferior to them in its accuracy and information content.
Reasons for increased indicators
When the number of cells in question per unit of blood increases, we are talking about thrombocytosis. As a rule, this is a secondary pathology that occurs against the background of the following conditions:
- treatment with certain medications;
- previous surgery;
- splenectomy;
- heavy blood loss;
- inflammation of the lining of the brain;
- kidney and liver pathologies;
- development of oncological formations;
- Iron-deficiency anemia.
The greatest danger of thrombocytosis is the formation of blood clots that can clog arteries. This often leads to heart attacks, strokes and other dangerous diseases.