Updated September 11: 138,992 Author: Dmitry Petrov
Hello, dear readers of the KtoNaNovenkogo.ru blog. People with a normally functioning circulatory system can be easily distinguished from the general crowd.
It is the coordinated functioning and the necessary balance of all the numerous components that make up the blood that provide a person with an excellent mood, vigor, activity, fullness of strength and energy.
Let's consider the features of platelets, which are one of the three main formed components in the blood - why it needs them and what their imbalance can lead to.
What is P-LCR or large platelet ratio in a blood test and why is the content higher than normal?
Patients are interested in P-lcr in a blood test - what it is, why it is tested.
Decoding this analysis allows you to obtain information about platelets that regulate clotting. For testing, blood can be taken from a finger or from a vein in the case of an advanced analysis. Blood sampling is almost painless and rarely causes discomfort. When taking blood from a vein, the arm is tied with a flagellum, the skin is treated with a disinfectant solution and pricked with a sterile needle. When taking blood from a finger, it is disinfected with an antiseptic and pierced with a medical blade.
The material is collected in a test tube and transferred for research, which must be carried out immediately in the first hours, because then a precipitate may form and it will be difficult to determine many indices.
For the study to be accurate, you need to prepare for it. You should not eat food 8 hours before the test, so the procedure is scheduled in the morning. Blood is taken from the patient on an empty stomach.
On the eve of the analysis you cannot:
- smoke;
- drink alcohol;
- drink coffee or tea;
- take medications.
Some drugs may distort the results. If the patient has chronic diseases that require constant use of medications, it is necessary to inform the doctor about this. The doctor will explain which medications should not be taken before the procedure.
Increase P-LCR
An increased number of large platelets means that there is a pathology in the body. Only in isolated cases is a high P-LCR value an individual characteristic of a person and does not require treatment.
Etiology
The reasons for an increase in P-LCR can be completely different diseases - inflammatory, oncological, hematological, infectious.
But most often, the formation of a large number of large platelets occurs in autoimmune disorders.
Systemic diseases that can cause thrombocytosis include: collagenosis (scleroderma, systemic lupus erythematosus, rheumatic diseases, periarteritis nodosa), sarcoidosis, polyarthritis, ankylosing spondylitis, enteropathy. These processes are accompanied by the release of interleukin and other inflammatory mediators into the blood, which stimulate the biosynthesis of thrombopoietin and the formation of a large number of platelets.
Along with this, the P-LCR index increases if the patient has:
- infectious pathology - bacterial, viral, fungal, parasitic,
- post-traumatic and postoperative syndrome,
- oncological and hematological diseases - lymphoma, neuroblastoma and hepatoblastoma, anemia,
- spleen diseases,
- cirrhosis or polycystic liver disease,
- damage or inflammation of the spinal cord,
- alcoholism,
- intoxication with chemicals that disrupt bone marrow function,
- atherosclerosis,
- diabetes mellitus
Some scientists believe that the increase in P-LCR is due to a congenital stem cell defect. In patients, the process of platelet formation is disrupted. The large cellular elements produced are defective and inactive. They are unable to adequately interact with other structures and function fully.
A high P-LCR index leads to the fact that the patient has a tendency to thrombosis. Due to the adhesive properties of platelets, they stick together and form a blood clot, which disrupts blood circulation and prevents the free movement of blood. As the thrombus grows, it narrows the lumen of the vessel, disrupts the blood supply to the organ, and causes hypoxia and ischemia of the tissue. When the coronary arteries are damaged, this leads to myocardial infarction. With thrombosis of cerebral vessels, an ischemic stroke develops. The result of the process is often varicose veins or atherosclerotic changes in the arteries. These pathologies are deadly and often result in the death of patients.
Symptoms
When the P-LCR increases, the patient develops corresponding clinical signs. They may go unnoticed behind the obvious symptoms of the causative disease. Such patients are not treated for thrombocytosis, which further aggravates the situation.
An increase in P-LCR is manifested by the following symptoms:
- hypersensitivity and pain in the fingertips,
- causeless appearance of hematomas,
- irritation and itching of the skin,
- cyanosis,
- asthenia of the body,
- rapid heartbeat,
- shortness of breath at rest,
- visual dysfunction.
These signs are optional. They can appear individually or in various combinations. But despite this, the patient needs to visit a health care facility and undergo certain tests, based on the results of which doctors will determine the cause of the P-LCR deviation and prescribe appropriate treatment.
Treatment and diagnostic procedures
To determine the cause of the disorder and make a correct diagnosis, in serious cases, a bone marrow biopsy is examined and blood is taken again. Additionally, general clinical and molecular tests and ultrasound of internal organs are performed.
To normalize the P-LCR value, the causative disease
. If the pathology is not treated, the patient risks dying from thrombosis, or more precisely from its consequences - acute coronary or cerebral failure. These phenomena are very dangerous. They are often fatal. That is why this deviation needs to be corrected. Hematologists carry out diagnostic and treatment measures. Restoration of normal P-LCR levels in a blood test is a sign of adequate and effective therapy.
- Patients are prescribed a diet rich in vegetables and fruits, vegetable oils, freshly squeezed juices and other products that make the blood less viscous. For the same purpose, experts recommend optimizing your drinking regime - drinking up to 2-3 liters of water per day.
- To prevent thrombosis and its consequences, the use of antiplatelet agents and anticoagulants is indicated - Aspirin, Cardiomagnyl, Trental, Cavinton, as well as drugs that improve microcirculation - Dipyridamole, Piracetam, Vinpocetine.
- If the cause of a high level of large platelets is an infectious disease, then after intensive antibiotic therapy, the P-LCR index value returns to normal almost immediately.
- In severe cases, the use of corticosteroids - Prednisolone, Dexamethasone and cytostatics - Anagrelide, Hydroxyurea, Radioactive phosphorus 32P is indicated.
- To stimulate the immune system, Interferon and its derivatives are prescribed.
- There are folk remedies that allow you to correct (but not eliminate) existing violations. These include: mulberry poison, sweet clover infusion, ginger tea, celery juice. These plants have a beneficial effect on the condition and activity of platelets.
Norm
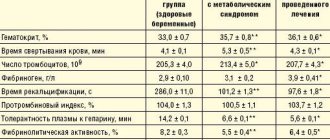
The normal platelet count in the blood of an adult is 13-43%. The indicator may deviate from the norm in some diseases.
Standard values depend on the person’s age:
- The norm for women and men is 180-320x10 9/l.
- In newborns and infants from 180 to 490 × 10 9/l.
- In children under 1 year of age, the indicator is 180-400 × 10 9/l.
- In children from 1 year to 6 years, 160-390 × 10 9/l.
- In children from 7 to 12 years old, 160-380×10 9/l.
- In adolescents from 12 to 18 years old, the indicator is 160-360 × 10 9/l.
If a laboratory test reveals a deviation from the norm, the doctor will prescribe an additional examination in order to establish a diagnosis, because changes in the indicator indicate the presence of pathology.
Different laboratories use different reagents and instruments, so the same person in different laboratories may get different results. The form indicates the patient’s indicators and normal values.
What is the norm?
In an adult, the normal level is considered to be from 180 to 400 g/l.
During pregnancy in women, the value can vary from 100 to 420 g/l, and immediately after menstruation - from 100 to 350 g/l. In infants, the norm is 150-450 g/l, and after a year of life, the platelet count becomes the same as in adults.
The lifespan of platelets is no more than 10 days, so some daily fluctuations in the level are considered normal.
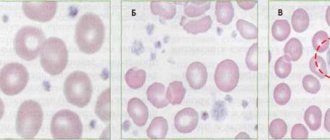
Platelets are not uniform in size, most are 3-4 microns in size, the smaller bodies are called microforms and the larger ones are called macroforms.
Treatment
Minor deviations from the norm do not threaten the patient’s life. The safest and most gentle treatment in this case is diet. It is recommended to include more foods that can thin the blood in your diet. Fresh garlic and onions are especially useful. Tomatoes and fresh juice from them, salad dressings with apple cider vinegar, fish oil, and olive oil reduce platelets. It is also necessary to include foods rich in magnesium in your diet and drink enough liquid, at least 2 liters per day. Avoid products that thicken the blood.
Increased value
An increased value of the large platelet ratio means that pathological processes are present in the patient’s body.
Causes
High levels mean that the following diseases may develop:
- thrombocytosis;
- circulatory disorders;
- obstructed blood movement through the vessels.
When a person is injured, large platelets stick together and form a blood clot, which clogs the damaged vessel and prevents bleeding. If a person’s index increases, then there is a risk of a blood clot in the vessel.
What do elevated platelets mean?
An increase in the concentration of Bizzocero plaques can warn of the presence of various pathological processes - the development of tuberculosis infection, blood cancer (leukemia), cancer of various organs, Hodgkin's lymphoma.
Thrombocytosis (increased platelets) is a constant companion :
- erythrocytosis;
- inflammatory intestinal and joint pathologies;
- chronic form of myeloid leukemia;
- acute course of infectious diseases;
- intravascular hemolysis and anemia.
lead to an increase in the number of platelets , which can ultimately lead to the development of thrombocytemia and failure of the functions of stem cells in the bone marrow.
Oddly enough, significant blood loss does not reduce the concentration of platelet platelets, but, on the contrary, increases it. This is due to the presence of compensated properties of the body that can replenish platelet losses.
It doesn’t matter for what reasons platelets go beyond the normative values. In such a situation, a medical assessment with appropriate therapy is necessary.
Reduced level
The reasons for a decrease in the P-lcr index can be chronic kidney disease, leukemia, and malaria. The index decreases after heavy metal poisoning and after chemotherapy.
A reduced level of the indicator occurs in pregnant women, after heart surgery, with adverse reactions caused by medications, with alcohol abuse, and lack of vitamin B12 and folic acid.
Thrombocytopenia can be caused by congenital bone marrow diseases and hereditary predisposition to this disease. A decrease in the rate is called thrombocytopenia. This diagnosis is made if the number of platelets has decreased by 3 times.
- the appearance of blood in the urine;
- skin rashes;
- it is difficult to stop bleeding from the nose;
- gums bleed;
- bleeding increases during menstruation.
The cause of thrombocytopenia must be quickly eliminated, because in this case, a minor injury can cause large blood loss. The attending physician must select individual therapy for this condition for the patient.
Lower P-LCR
On the contrary, a decrease in the P-LCR index, as well as the total number of platelets, is a sign of thrombocytopenia. This term unites a whole group of hemorrhagic diathesis, differing in etiology, pathogenesis, and course. As a result of a decrease in the number of platelets in the blood, the risk of bleeding and hemorrhage increases.
Etiology
The giant platelet ratio decreases under the influence of pathological and physiological reasons.
- In healthy people, a reduced content of large platelets in the blood is caused by pregnancy, alcohol abuse, deficiency of B vitamins, and taking certain medications - sedatives, antibacterials, sulfonamides.
- A low level of P-LCR is a laboratory diagnostic criterion for the following diseases: renal pathology, leukemia, malaria, lymphomas, hemangiomas, portal hypertension, tuberculosis infection, influenza, measles, rubella, congenital bone marrow anomalies.
- This indicator decreases as a result of poisoning with heavy metal salts or after cytostatic chemotherapy or radiation therapy.
- Thrombocytopenic purpura is an autoimmune disease in which the body produces antibodies to its own platelets. As a result of their destruction, huge platelet cells are formed with impaired functional activity, which leads to undesirable consequences.
- Hereditary diseases based on giant platelet syndrome. Defective cells are the cause of immune and hematological disorders, occurring in the form of thrombocytopenia with a high tendency to bleeding.
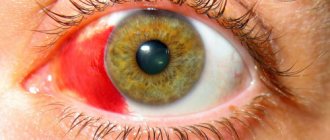
signs of thrombocytopenia/coagulopathy
Symptoms
Clinical signs of low large platelet counts include:
- rapid injury to mucous membranes,
- hematuria,
- blood in stool
- hemorrhagic rash on the skin, petechiae,
- spontaneous and persistent nasal, gingival, uterine, pulmonary, renal, intestinal bleeding,
- heavy and prolonged menstruation,
- ecchymosis at injection sites.
To diagnose a disease that causes thrombocytopenia, patients need to undergo a number of studies:
- coagulogram,
- immunogram,
- MRI and ultrasound of internal organs,
- medical and genetic counseling.
When microscopying a patient's blood sample, platelets of unnaturally large sizes are detected. Specialists record the time during which bleeding occurs, determine the platelet aggregation index, and conduct flow cytometry. The results of a comprehensive diagnostic examination allow doctors to understand the exact picture of the pathology.
Treatment
Thrombocytopenia is dangerous due to the development of spontaneous bleeding, which causes large blood loss. To restore the P-LCR indicator, drug treatment is carried out. Patients are prescribed hemostatic drugs that prevent or stop bleeding - angioprotectors "Etamzilat", "Ditsinon", "Vikasol", fibrinolysis inhibitors "Aminocaproic acid", "Tranexamic acid". They are strictly prohibited from taking drugs with antiplatelet effects - anticoagulants, antiplatelet agents, NSAIDs. These medications interfere with blood clotting and may increase bleeding.
To raise it to normal
platelet count, you should eat right, excluding spicy, salty, fried foods, marinades, and alcohol from your diet.
In severe cases, patients are transfused with platelet mass or donor blood.
All patients with signs of hemorrhagic syndrome are hospitalized in a hospital for emergency medical care. After establishing the cause of the decrease in the number of giant platelets, etiotropic therapy is carried out aimed at eliminating the underlying disease. Patients are prescribed drugs of various groups - glucocorticosteroids, cytostatics, immunomodulators. If conservative treatment fails, removal of the spleen is indicated. Most hereditary pathologies accompanied by a decrease in P-LCR are incurable, lifelong disorders with a high risk of prolonged bleeding, chronic neuropsychiatric problems and death due to major blood loss.
Persons with an increased or decreased P-LCR value need to lead a healthy lifestyle: do not drink or smoke, minimize stress, optimize work and rest schedules, get enough sleep, walk a lot and for a long time in the fresh air, be physically active, but avoid active sports, which may cause injury.
Deviation of P-LCR from the norm is a reason to contact a hematologist and treat existing pathological processes.
Don't delay going to the hospital.
Self-medication is strictly prohibited. An incorrectly identified cause of the problem can lead to incorrect treatment and the development of serious consequences - thrombosis or hemorrhage.
Symptoms of diseases
The large platelet ratio is a test that must be performed to determine the condition of the blood. Deviations from normal indicators can indicate various diseases. In this case, the level can either increase or decrease depending on the reason. A change in the level of cells in the blood indicates the presence of pathological changes in the human body. To understand what p lcr or large platelet ratio is responsible for and how to bring it back to normal, you need to learn more about these blood cells.
Features of primary thrombocytosis
Disturbances in the functioning of the bone marrow lead to a significant increase in platelets in the blood. This means that a lot of excess substances begin to enter the liver and spleen. Elderly patients are more susceptible to primary thrombocytosis; in young people and children this deviation is much less common. The disease is characterized by disturbances in the functioning of systemic organs, which causes deterioration of well-being and headaches.
Parameters for research
A medical examination begins with general tests. If there are alarming symptoms and complaints from the patient, the standard test is expanded. In addition to the total number of cells, the laboratory can evaluate their condition, size, mobility, maturity and other factors. So, with a normal overall level of platelets, the number of large cells may be increased, which means a violation of some processes in the body.
The study is carried out in laboratory conditions. The general clinical analysis may not include a P-LCR (Large Platelet Ratio) test. This and other parameters for analysis are indicated in the referral at the discretion of the physician. P-LCR reflects the proportion of enlarged platelets relative to normal-sized cells, measured as a percentage. LCC or large platelet fraction is essentially the same as P-LCR but is measured in absolute value.
During illness or the development of pathology, any of these indicators may be lowered or increased. Changes in the quantity and quality of blood cells, as well as their functions, are reflected by a clinical blood test. To determine possible violations, the test results are deciphered. The interpretation of the obtained data is carried out by a qualified specialist, taking into account all factors that could influence the results of the study.
How is their level determined?
Let us immediately note that, as such, there is no separate analysis for the determination of platelet plates.
An assessment of their functions and condition is carried out in conjunction with a general analysis of the blood clinic, displaying the result with the abbreviation - PLT (mandatory indicator) and the measurement of thrombocrit - PCT (the level of their concentration in the total volume of blood).
This analysis does not take into account the ratio of age groups and platelet forms (irritation and degeneration).
A more detailed analysis of platelet properties is determined in certain conditions (before surgery, during bleeding, and other critical conditions) by the hemostasiogram (coagulogram) method using screening tests that determine the consistency of the hemostasis process.
What are platelets
Red blood cells produced in the bone marrow are called platelets. They lack a nucleus and are the smallest cells compared to white blood cells and red blood cells. Despite this, their importance in the body is very great.
Thanks to these cells, blood has the ability to clot, which protects a person from blood loss during wounds and injuries:
- An abnormal platelet level often indicates diseases that occur in the human body.
- But the number of cells can also change due to temporary factors, for example, after physical activity.
After production, platelets remain in the blood for 5 to 11 days, after which they are destroyed in organs such as the liver and kidneys.
Based on their origin, platelets are divided into 3 types:
The division into types occurs depending on the reason that caused the generation of cells. Several factors can influence an increase or decrease in the large platelet ratio.
A blood test and further examination of the person will help identify the underlying cause. After which the doctor prescribes treatment adequate to the disease, and the patient may be hospitalized: the sooner the causes are identified, the more effective and easier the course leading to recovery will be.
Platelets are...
A thrombus is a blood clot (translated from Greek), the basis of which is platelets.
A platelet is a small, colorless, spherical platelet of blood (Bizzocero plaque). Plates are formed from the plasma structure (megakaryocytes - plasma cells) of the bone marrow. Platelets do not have a nucleus, but are equipped with an abundant number of granules (more than 200).
The value of granulations is due to the high content of special components of platelet growth (thromboxane, thrombin, adenosine diphosphorate and other factors), which ensure the formation of amino acids and enzymes (what are they?) that destroy the membranes of bacterial cells, of pathogens into the blood
The size of platelet plates varies within their age (young, middle, mature), from 2 to 5 microns.
However, when a platelet comes into contact with a surface that does not correspond to the internal vascular endothelium or the cavity of the cardiac pericardium, the plates are activated, releasing up to 10 pseudopods (processes) tens of times larger than the size of the plate itself.
This feature allows platelets to serve as a kind of “patch” that, if necessary, covers the wound surfaces of blood vessels, preventing bleeding.
It is the pseudopods that ensure the movement of the plates through the circulatory system. Platelets have the ability to adhere to foreign agents , capture them and destroy them, form a blood clot by aggregation (gluing the plates together) to prevent hemorrhagic processes (bleeding).
The main role of platelets is to actively participate in the process of blood clotting (hemostasis).
They provide a transport function, delivering nutritional components to the tissues (endothelium) lining the internal cavity of the vascular walls. They remain viable for up to 10 days , after which they are destroyed in various organs (spleen, lungs, or liver).
Recent developments by Japanese scientists have proven that megakaryocytes are not the only sources of formation of Bitsocerro plaques (platelets). They were able to obtain platelets from the patient's own stem cells.
These studies increase the success of transplantation, since the presence of such platelets does not cause the body to reject donor organs.
How platelets participate in the process of hemostasis can be seen in the diagram:
Having appreciated the basic functions of platelets, you can understand what their imbalance in the body entails and what the negative consequences may be.
Any imbalance in platelet activity and number is medically called thrombocytopathy.
- A decrease in the concentration of platelet platelets is called thrombocytopenia.
- And an increased concentration is thrombocytosis.
- A dysfunction of their activity is diagnosed as thrombosthenia.
Symptoms
When the P-LCR is elevated, the patient exhibits physical symptoms of the condition. In most cases, they can be overlooked due to obvious symptoms of the underlying disease. When treating a disease in a hospital setting under the supervision of the attending physician, blood is taken regularly for testing. At the same time, it is impossible to miss the moment when the level of platelets or P-LCR begins to increase. But the patient himself can determine the condition in which platelet cells increase in size by the following symptoms.
- High sensitivity of the fingers, especially the tips, to the point of pain.
- The appearance of bruises and subcutaneous hemorrhages for no apparent reason.
- A bluish tint to the skin and an itchy sensation.
- General weakness of the body, lethargy, decreased ability to work.
- Decreased vision.
- Frequent nose and intestinal bleeding, women have heavy periods.
It is extremely unlikely that all symptoms of high P-LCR will occur at once. As a rule, patients note the appearance of 2-3 signs, which is a reason to consult a doctor and undergo appropriate tests. The sooner the cause of the disease is identified, the higher the chances of a speedy and successful recovery.
Symptoms and diagnosis
Signs of thrombocytosis, especially secondary, in the initial phase may not be recognized by the symptoms of the disease that caused it.
But if this disease is treated in a hospital setting, where blood tests are performed regularly, then it is impossible to miss the increase in platelets. However, you should know the main signs of this deviation :
- Subcutaneous hemorrhages. You should pay attention to the appearance of bruises for no reason.
- Increased sensitivity of the fingertips and pain.
- Constantly itchy skin can indicate more than just dermatological diseases. In addition, the skin may take on a bluish tint.
- Intestinal, uterine and nasal bleeding.
- Lethargy, weakness, blurred vision.
It is not necessary that all symptoms will appear at once. But the appearance of 2-3 of them is grounds for a visit to the doctor. To make a correct diagnosis, it is necessary to take into account all the patient’s current illnesses and those that he suffered previously. Additional tests and studies include:
- general blood analysis;
- bone marrow biopsy;
- molecular research;
- Ultrasound of the pelvic and abdominal organs.
Reasons for changing the coefficient
As already mentioned, various factors can cause a decrease or increase in the level of large platelets.
- inflammatory processes;
- various diseases;
- hematological factors;
- temporary reasons.
Inflammatory processes that provoke a sharp increase in red blood cells in the blood include diseases such as hepatitis, polyarthritis, rheumatoid purpura, inflammatory enteropathy and others. Having a negative effect on the body, these diseases provoke an increase in interleukins, which are an anti-inflammatory substance. The production of these substances is accompanied by an increase in platelet counts in the blood.
And cancer cells can also provoke a change in the coefficient. Oncological diseases often cause thrombocytosis. Lymphomas and hepatoblastoma can also lead to changes. And also the level of cells in the blood changes in patients during the postoperative period. People who are anemic usually have elevated platelet levels in their blood tests.
Reasons that may temporarily affect platelets may include:
- pregnancy;
- injuries;
- physical exercise;
- suffered stress.
The reasons for the change may be temporary (in which case the condition returns to normal without much effort) or such that they will require long-term treatment.
Causes
So why are platelet levels rising? By origin, thrombocytosis is usually divided into three types: primary, secondary and clonal. The first type of disease causes disturbances in the functioning of the bone marrow, which is responsible for the generation of this type of cell. The second type is a consequence of one or several factors at once. These may be physiological reasons, which include:
- pregnancy;
- physical stress;
- increased adrenaline levels.
A number of factors of pathological origin also lead to secondary thrombocytosis.
Inflammation
Inflammatory processes in the body leading to thrombocytosis can cause the following diseases :
- Kawasaki disease;
- collagenosis;
- sarcoidosis;
- rheumatoid purpura;
- juvenile polyarthritis;
- chronic hepatitis;
- ankylosing spondylitis;
- chronic inflammatory enteropathy.
These diseases cause a significant increase in pro-inflammatory interleukin, leading to increased synthesis of thrombopoietin and a subsequent increase in the number of platelets in the blood.
Tumors
The cause of an increase in the platelet ratio can be any cancer, but the most common are: lymphoma, neuroblastoma and hepatoblastoma.
Trauma and postoperative syndrome
Post-traumatic stress, as well as surgery, can cause platelet levels to increase.
These include some diseases accompanied by extensive tissue damage:
- enterocolitis;
- pancreatitis;
- tissue necrosis.
Hematological factors
The most common hematological cause of increased platelets is anemia, or iron deficiency in the body , although the relationship between these phenomena has not yet been fully studied. Chemotherapy, as well as acute bleeding, generates the phenomenon of platelet involvement in the bone marrow.
Symptoms
There are practically no symptoms of an increase in the average platelet volume at the initial stage, so the presence of pathology can only be determined from a blood test. As the disease progresses, signs appear that indicate an increase in volume.
Note!
Increased average volume and increase in quantity are not equivalent values. In certain conditions, the platelet count may be low; in other cases, it may be high.
The symptoms are quite varied, and some are signs of other diseases:
- Hemorrhages
. They most often occur when platelet levels are low. They appear as causeless bruises. These bruises may be painful when palpated. - Bleeding
. Bleeding from the nose and ears occurs, women may experience discharge from the genital tract, and bleeding gums are observed. Bleeding occurs spontaneously. - Itching of the skin
, which persists after taking antihistamines, may also indicate an increase in the average platelet volume. - Soreness and numbness in the fingertips
. They become sensitive and pain is felt when pressed. This condition occurs when the platelet count is elevated. - Change in skin color
: it acquires a bluish or reddish tint, or pronounced pallor is noticeable. - Increased fatigue
, drowsiness, weather dependence.
Other symptoms include blurred vision, surges in blood pressure, blood clots, and frequent migraines.
It is important to understand that an increased average platelet volume is a serious pathology that cannot be left to chance. It provokes stagnation and the formation of blood clots. And this, in turn, can lead to heart attacks, strokes, and thromboembolism.
(2 ratings, average 4.5 out of 5)
Types of hematological studies
The main hematological study is a clinical blood test, the results of which reflect the general condition of the body and provide the doctor with information about the nature of hematopoiesis (blood formation). The analysis is used to diagnose inflammatory processes, anemia, leukemia and many other pathological conditions.
The study is prescribed to all patients who seek specialized medical care. It is also carried out during pregnancy, preventive examinations, and during medical examination.
The biological material for research can be capillary or venous blood. A clinical blood test consists of many tests (from 8 to 30). Some of these may be independent hematology studies.
Preparing for analysis
- Two weeks before the test, it is important to stop taking medications. If drugs are vital, then the conditions for correcting treatment are discussed with the doctor.
- The day before the test, you need to exclude fatty and fried foods from the menu, give up alcohol, and avoid physical and emotional stress.
- On the eve of the study, dinner should be no later than 22.00.
- The test is taken in the morning on an empty stomach. Before the study, you should not smoke, drink coffee or tea. It is allowed to drink water in a volume of no more than 0.5 liters.
Carrying out analysis
This test shows the number of platelets, their maturity and size. The index is called the large platelet ratio. The study indicates changes in particle number and associated pathology. Blood is drawn in the laboratory.
For testing, blood can be taken from a finger or from a vein in the case of an advanced analysis. Blood sampling is almost painless and rarely causes discomfort. When taking blood from a vein, the arm is tied with a flagellum, the skin is treated with a disinfectant solution and pricked with a sterile needle. When taking blood from a finger, it is disinfected with an antiseptic and pierced with a medical blade.
The material is collected in a test tube and transferred for research, which must be carried out immediately in the first hours, because then a precipitate may form and it will be difficult to determine many indices.
For the study to be accurate, you need to prepare for it. You should not eat food 8 hours before the test, so the procedure is scheduled in the morning. Blood is taken from the patient on an empty stomach.
On the eve of the analysis you cannot:
- smoke;
- drink alcohol;
- drink coffee or tea;
- take medications.
Some drugs may distort the results. If the patient has chronic diseases that require constant use of medications, it is necessary to inform the doctor about this. The doctor will explain which medications should not be taken before the procedure.