When should you take a Magnesium (blood) test?
- Suspicion of the development of magnesium deficiency;
- Suspicion of the development of hypermagnesemia (increased magnesium in the blood);
- Comprehensive examination of persons with malabsorption of nutrients and persons suffering from alcoholism;
- Treatment with drugs that affect the level of magnesium in the body;
- Presence of diabetes mellitus, kidney disease;
- To assess renal function (along with the determination of blood urea and creatinine);
- Determining the cause of low levels of calcium, potassium, phosphorus in the blood.
General information
Like other macro- and microelements necessary for the body, magnesium comes with food and is absorbed into the gastrointestinal tract. There is a small amount of it in the blood (about 1%), the main part is found in various cells and tissues. Normally, the amount of a macronutrient is maintained at a stable level by regulating its absorption and excretion in the urine. An excess of this substance can occur with an overdose of drugs containing magnesium compounds, as well as in the case of kidney dysfunction. A deficiency of a macronutrient may not manifest itself in any way for quite a long time. If its deficiency is significant or is not replenished for a long time, symptoms such as decreased appetite or its complete loss, nausea, weakness, muscle spasms, and confusion appear. When there is an excess of a macronutrient, similar symptoms appear. Heart rhythm disturbances may also be added to them.
Detailed description of the study
Magnesium is necessary for the normal functioning of cells and tissues of the body. It is involved in more than 300 biochemical reactions. This microelement is important for the regulation of normal muscle contraction, for the functioning of the cardiac conduction system and the transmission of nerve impulses.
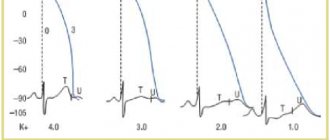
Magnesium is of great importance in the transport of potassium and calcium ions through the cell wall. This process is important in muscle contraction, conduction of nerve impulses, regulation of vascular tone and maintenance of normal heart rhythm.
This microelement is used for the formation of DNA and RNA, participates in the reactions of aerobic (oxygen) and anaerobic (oxygen-free) energy synthesis (oxidative phosphorylation and glycolysis), and also acts as a cofactor - a non-protein compound that activates enzymes (substances that accelerate biochemical reactions).
The main depot of magnesium in the body is bone tissue, it contains about 60% of the total amount of magnesium, the remaining 40% is contained in the cells of other organs and tissues. Magnesium is excreted by the kidneys.
Water contains about 10% of the daily required amount of magnesium. The main sources of magnesium are the following foods: vegetables and greens (such as spinach), nuts, seeds and unprocessed grains, which are also rich in magnesium. Legumes, fruits, fish and meat contain less magnesium. Most magnesium is absorbed in the small intestine.
Many people do not reach their daily magnesium intake, which is approximately 3.6 mg/kg. A lack of magnesium - hypomagnesemia, is more common than hypermagnesemia (excess), and can lead to disruption of the normal functioning of the heart, muscles and the development of neurological disorders.
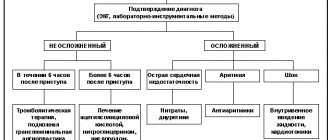
Hypomagnesemia is accompanied by a number of nonspecific symptoms. Early symptoms of deficiency of this microelement are: nausea, lethargy, weakness, loss of appetite, increased fatigue. A more pronounced deficiency is accompanied by an increase in neuromuscular excitability and the development of seizures. Hypomagnesemia can cause cardiac arrhythmias, including atrial and ventricular tachycardia, prolongation of the QT interval when recording an ECG.
Hypomagnesemia is often associated with other electrolyte abnormalities such as hypocalcemia, hypokalemia.
The causes of hypomagnesemia are:
- Poorly controlled diabetes mellitus type 1 and 2;
- Alcohol abuse;
- Taking medications (laxatives, diuretics, digoxin, cyclosporine, insulin);
- Malabsorption (impaired absorption of substances in the small intestine);
- Endocrine diseases (dysfunction of the thyroid and parathyroid glands).
In addition, low levels of magnesium in the blood are very often detected in the second and third trimesters of pregnancy; a deficiency of this microelement increases the risk of premature birth, miscarriages and other pregnancy pathologies.
Hypermagnesemia is less common. It can occur with impaired renal function, severe renal failure, Addison's disease, dehydration, hypothyroidism, hyperparathyroidism. Most often, hypermagnesemia results from excessive intake of magnesium supplements or the use of certain medications (aspirin, lithium).
A study of the level of magnesium in the blood is used if there is a suspicion of excessive or insufficient intake of it in the human body, as well as if there is a suspicion of a violation of the processes of its absorption and excretion from the body.
Indications for the study
A blood test for magnesium can be prescribed at certain intervals to monitor the condition of patients whose diseases are accompanied by potassium or calcium deficiency. The test is also prescribed if the following symptoms are present:
- impaired clarity of consciousness;
- muscle weakness;
- heart rhythm disturbance;
- cramps or muscle twitching.
Also, the amount of this macroelement must be monitored in patients with alcoholism, malabsorption syndrome, diarrhea, and nutritional deficiency. For patients with diabetes and chronic kidney problems, this test is prescribed regularly at certain intervals. Its results are used to evaluate kidney function.
general characteristics
The fourth most abundant element in the human body and the second most abundant element in the cell after potassium. 60% of it is part of bone tissue, and most of the rest is in cells. Mg is a calcium antagonist. The higher the metabolic activity of a cell, the more Mg it contains. It is a cofactor for a number of enzymatic reactions, plays the role of a physiological growth factor, maintains the supply of purine and pyrimidine bases, and is necessary at all stages of protein synthesis. Magnesium deficiency during pregnancy contributes to the development of gestosis, miscarriages and premature birth.
Interpretation of results
The test uses venous blood. It is taken on an empty stomach after a 12-hour fasting break. Interpretation of the results is carried out taking into account the patient’s age, clinical picture, data from other laboratory and instrumental studies.
Flaw
macronutrient may indicate diabetes mellitus, Crohn's disease, hypoparathyroidism, diarrhea. It is also often observed in toxicosis of pregnant women. Low rates can also be explained by lack of nutrition (for example, in patients with alcoholism or in the elderly), long-term use of a number of medications. During pregnancy (second and third trimester), low levels are usually caused by an increased need for this macronutrient.
Oversupply
magnesium is observed in patients with renal failure, hypothyroidism, hypoparathyroidism, Addison's disease, and dehydration. Excessive accumulation of macronutrients can also be caused by medications (eg, certain antibiotics, aspirin).
In most cases, this test is not used as an independent study, but is prescribed in conjunction with tests for other electrolytes. If its results are within normal limits, this does not make it possible to completely exclude macronutrient deficiency. Due to natural compensation mechanisms, its level in the blood can be maintained within normal limits for a long time. In this case, macronutrient reserves are released from body tissues. To make an accurate diagnosis, additional examination is required in such cases.
Magnesium deficiency. Cases from the practice of a neurologist
Clinical observation 1. Hyperventilation syndrome Patient L., 40 years old, chief physician of one of the Moscow clinics. Complaints: low mood, irritability, fatigue, feeling of exhaustion; poor tolerance to changing weather conditions; lability of blood pressure with increases up to 140/100 mm Hg. and more, rapid heartbeat, frequent pain in the heart and dizziness against the background of emotional experiences, accompanied by a feeling of “lack of air” and “coma in the throat”; difficulty falling asleep and daytime sleepiness; increased sweating in the armpits, palms and feet, convulsive movements of the calf muscles. History of the disease. The mild complaints described above have been bothering me periodically over the last year, during which the patient notes a tense interpersonal situation at work and at home. Given the medical background, the patient neglected communication with his colleagues and was treated independently. The diagnostic search excluded somatic pathology. Sedative and restorative therapy was carried out. However, against the backdrop of 2 weeks of hard work and an escalation of the conflict with management, the intensity of the complaints increased. The usual treatment regimens did not improve the condition. Constant pain appeared in the heart area. This forced the patient to contact the Department of Pathology of the Autonomic Nervous System for examination and subsequent treatment. Life story. He grew up and developed as a strong, athletic child. At a young age, he suffered an injury to his right knee joint with full recovery. I was involved in bodybuilding. Among previous diseases, gastritis is indicated. He has been working as a general practitioner since the age of 23. Married, has two children. Upon examination, the condition is satisfactory, the physique is athletic. The background mood is reduced. No somatic disorders were identified. There are no meningeal signs in the neurological status. No pathology was detected from the cranial nerves. There are no paresis. Muscle tone is not changed. Tendon reflexes are moderately animated D=S, there are no pathological signs. The Romberg test is negative, coordination is not impaired. No sensory disorders were identified. When assessing the autonomic nervous system, acrocyanosis of the hands and feet, sweating in the armpits, palms and soles, frequent sighs, uneven depth and frequency of breathing, and emotional lability were noted. When studying neuromuscular excitability at rest, Khvostek's symptom was negative; after 3 minutes of hyperventilation, an increase in neuromuscular excitability was noted (III degree Khvostek's symptom in combination with convulsive sensations in the feet and paresthesia in the calves). Paraclinical examination. Consultation with an ophthalmologist, therapist, ECG, ultrasound examination of the brachiocephalic vessels, radiography of the skull and cervical spine did not reveal any significant pathology. Pathologists did not reveal a general blood and urine test or a biochemical blood test. A study of the microelement composition of hair and psycho-vegetative testing was carried out (Table 1). Its results did not reveal a pronounced anxiety-depressive syndrome in the patient; there was a decrease in the quality of night sleep, levels of well-being, activity and mood. There were autonomic dysfunction and pronounced signs of hyperventilation syndrome, a decrease in stress resistance and quality of life in our patient. Carrying out the “30:15” cardiovascular test and spectral analysis of heart rate variability in a state of relaxed wakefulness and active orthotest made it possible to assess the autonomic regulation and adaptive capabilities of the patient. A decrease in parasympathetic influences on the heart was revealed in the form of a low index “30:15” and a low representation of respiratory influences at rest against the background of excessive sympathicotonia, which led to rigidity of the heart rhythm against the background of tachycardia and increased blood pressure. When an orthostatic load was presented, the detected sympathetic reactivity was provided not by segmental regulatory mechanisms, but by excessive activation of suprasegmental structures, which reflects not only the strain of functioning under normal conditions, but also a violation of adequate adaptive mechanisms in this patient. Hair analysis determined magnesium deficiency compared to normal. Based on the obtained clinical and paraclinical data, the patient was diagnosed with psychovegetative syndrome. Syndrome of vegetative dystonia against the background of chronic emotional stress with hyperventilation manifestations and decreased adaptive capabilities. The patient was prescribed a 2-month course of Magne B6 therapy at a dose of 1 ampoule of a drinking solution 3 times a day for 2 weeks, followed by a transition to taking 1 ampoule 2 times a day with meals. While taking the drug, complaints were reduced. The background mood and sleep improved, activity and performance increased, blood pressure stabilized, heart palpitations, a feeling of lack of air, and cramps in the calf muscles stopped bothering me. Subjective improvement was noted from the middle of the second week of taking the drug. However, increased sweating during excitement and poor tolerance to changes in weather conditions still persisted, but the intensity of these manifestations was much lower. Against the background of an increase in magnesium content in the body, positive dynamics of psycho-vegetative indicators were noted. Despite the fact that magnesium levels only reached subthreshold values, improvements were found in test scores. There was also a beneficial effect on autonomic regulation at rest (vagotonia and increased heart rate variability, normalization of blood pressure and pulse) and orthotest (increased “30:15” index and segmental sympathetic influences in terms of hemodynamics and heart rate variability). This indicates an improvement in vegetative support and the formation of adequate adaptation mechanisms. This, in turn, helps reduce hyperventilation syndrome and increase his resistance to stress while staying in our patient’s previous living conditions. Conclusion. Clinical manifestations of chronic emotional stress were expressed in a decrease in adaptive abilities and were accompanied by a decrease in magnesium content in the body and clinically pronounced autonomic dysregulation in the form of hyperventilation syndrome. Even partial replenishment of magnesium deficiency contributed to the reduction of subjective and objective manifestations of the latter. Clinical observation 2. Episodic tension headaches Patient L., 52 years old, complained of frequent (up to 15 times a month) diffuse headaches of a compressive nature in the second half of the working day or after emotional stress, of average intensity (intensity according to the visual analog scale was 6–7 points). The headache was accompanied by a feeling of rapid heartbeat, pain in the heart area, numbness in the hands and feet, and difficulty breathing like a “coma in the throat.” The headache was not accompanied by nausea, photo- or phonophobia, and was not aggravated by the patient’s usual activities. Headaches decreased after taking analgesics in combination with muscle relaxants and sedatives (for example, No-shpalgina with Valocardin). The patient also complained of low mood, tearfulness, fatigue, sleep disturbances in the form of difficulty falling asleep and early morning awakenings, poor tolerance of stuffy rooms, and periodic pain in the heart area. History of the disease. She became ill 9 years ago when, due to chronic emotional stress (divorce from her husband), sleep was disturbed and periodic diffuse pressing headaches occurred. She was treated on an outpatient basis with nootropic, vascular and vitamin preparations with a positive effect. I noticed an improvement in my health in the spring and summer, during vacations. About a year ago, due to dismissal from work and the onset of menopause, headaches became more frequent and more intense. Conventional treatment regimens did not improve the patient's condition. Against this background, pain appeared in the heart area and sensations of respiratory distress. Life story. Among previous diseases, gastritis is indicated. Referred by a therapist to the Department of Pathology of the Autonomic Nervous System for examination and treatment. Upon examination, the condition is satisfactory. The background mood is reduced. No somatic disorders were identified. There are no meningeal signs in the neurological status. No pathology was detected from the cranial nerves. There are no paresis. Muscle tone is not changed. Tendon reflexes are moderately reduced D=S, there are no pathological signs. The Romberg test is negative, coordination is not impaired. No sensory disorders were identified. The temporal, masticatory, trapezius and splenius muscles of the neck without an accent on the side, the pectoralis major and minor muscles with an accent on the left and without the presence of trigger points in them are sharply painful and tense during palpation. When assessing the autonomic nervous system, increased neuromuscular excitability (III degree Chvostek's symptom), persistent pink dermographism, lability of heart rate, generalized sweating, frequent sighs, uneven depth and frequency of breathing, and decreased mood were noted. Paraclinical examination. Consultation with an ophthalmologist, therapist, ECG, ultrasound examination of the brachiocephalic vessels, radiography of the skull, cervical and thoracic spine did not reveal any significant pathology. Psychovegetative testing was carried out, the results of which revealed that the patient had moderate depression (12 points on the Beck test with a norm of up to 9 points), reactive anxiety (43 points on the Spielberger test with a norm of up to 30 points), as well as a decrease in the quality of night sleep (13 points with a norm of 22 points) and quality of life (by 80% with a norm of up to 10%). When studying the magnesium content in a hair biopsy, the level of the microelement was low and amounted to 19 μg/g. Thus, the patient had the following syndromes: 1. Cephalgic syndrome (frequent, but not more than 15 days a month, diffuse bilateral contracting headaches with an intensity of 6–7 points on a visual analogue scale, not aggravated by habitual daily physical activity, but significantly disrupting social activity of the patient, reducing her performance, worsening her quality of life). 2. Psychovegetative syndrome (in the form of moderate depression, anxiety, asthenia, dyssomnia, cardialgic and hyperventilation syndromes). 3. Painful tension of the pericranial, cervical and pectoral muscles. 4. Established magnesium deficiency. Based on this, the patient was diagnosed with psychovegetative syndrome. Anxiety-depressive syndrome of moderate severity. Episodic tension headaches with tension in the muscles of the neck, scalp aponeurosis and pectoral muscles. Menopause. The patient was prescribed a 2-month course of therapy with Magne B6 at an initial saturating dose of 2 tablets 3 times a day for 2 weeks, followed by transfer to a 2-time dose for 2 months. During this period, the patient actively kept a “Headache Diary”, in which she noted the duration in hours and intensity in points on the visual analogue scale of headaches. During 2 weeks of therapy, pain intensity (4 points) and frequency (1–2 times a week) significantly decreased, and sleep improved (20 points). By the end of the 8th week, the patient was not bothered by headaches. A repeat examination after 2 months revealed a pronounced positive trend in the form of an increase in magnesium content in the body (41 mcg/g). This was accompanied by a reduction in cephalgic, psychovegetative syndromes and painful muscle tension. Headaches did not bother me. My mood improved and I felt more energetic. Depressive and anxiety symptoms were not detected either clinically or based on the results of psychometric testing. There were no signs of hyperventilation syndrome. Cardialgia and interruptions in heart function did not bother me. The drug had a beneficial effect on the muscular component of the pain syndrome: there was no tension in the pericranial, cervical and pectoral muscles. The patient's quality of night sleep significantly improved (23 points). All this contributed to improving the patient’s quality of life. Conclusion. A course of Magne B6 in a patient suffering from episodic tension headaches with moderately severe psychovegetative syndrome and painful muscle tension contributed to the reduction of the latter, thereby significantly improving the patient’s quality of life and her social adaptation.
Discussion. The presented clinical case shows the development of tension headaches in a patient with increased anxiety during a period of hormonal changes who is not receiving adequate therapy. In the treatment of episodic tension headaches in this patient, it was necessary to influence the main mechanisms involved in the formation of headaches: correction of mental disorders (anxiety), reduction of muscle tension. Chronic stress, combined with hormonal changes in the body, led to decompensation and transformation of rare episodic tension headaches into frequent ones. It should be noted that the clinical picture of such headaches is combined with pain syndromes of other localization, for example, pain in the heart and abdomen, which are somatic masks of depression. Frequent comorbid syndromes with headaches are permanent or paroxysmal psychovegetative disorders.
Clinical observation 3. Chronic fatigue A 33-year-old woman complained of feeling exhausted, daytime sleepiness, increased fatigue, decreased concentration and memory, emotional lability in the form of sudden mood swings, irritability and tearfulness, as well as diffuse muscle pain, including left half of the chest, sleep disturbances in the form of difficulty falling asleep and shallow sleep, which did not bring a feeling of rest and recuperation. When the weather changes, there is a deterioration in health, poor tolerance of cold and heat. History of the disease. Throughout the year, general weakness, fatigue, attention problems, and irritability have been a concern. 6 months ago, after the sudden death of my father, sleep disturbances and tearfulness appeared. Diffuse muscle pain also developed. The patient underwent a comprehensive diagnostic examination, which made it possible to exclude organic somatic pathology. Slightly expressed radiological signs of spinal osteochondrosis were revealed. The attending physician referred the patient for consultation with subsequent therapy to the Department of Pathology of the Autonomic Nervous System of the Research Center MMA with a diagnosis of “Neurocirculatory dystonia. Astheno-neurotic syndrome." Life story. The patient, from her first normal pregnancy, grew up and developed as a healthy child, but since childhood she was easily vulnerable, tried to avoid conflict situations, and suffered from grievances for a long time. She was interested in music, drawing, and writing poetry. She was the only child in the family. Denies chronic diseases of internal organs. Menstrual function was not impaired, there were no pregnancies or childbirths. Social status – unmarried, works as a leading accountant in a large foreign company. On examination, the condition is satisfactory, the physique is asthenic. The background mood is reduced. No somatic disorders were identified. There are no meningeal signs in the neurological status. No pathology was detected from the cranial nerves. There are no paresis. Diffuse painful muscle tension is noted in the head, neck, and chest. Otherwise, muscle tone is unchanged. Tendon reflexes are alive D=S, there are no pathological signs. The Romberg test is negative, coordination is not impaired. No sensory disorders were identified. When assessing the autonomic nervous system, spotty hyperemia on the neck, face and chest, increased sweating of the palms and feet, and emotional lability were noted. When studying neuromuscular excitability at rest, grade II Khvostek’s symptom, after 3 minutes of hyperventilation, an increase in neuromuscular excitability was noted (grade III Khvostek’s symptom in combination with paresthesia in the feet). Paraclinical examination. Based on the results of the studies, minimal manifestations of spinal osteochondrosis were identified. The use of algometry made it possible to identify a decrease in pain sensitivity thresholds in the studied muscles of the head, neck and pectoral muscles, which manifested itself in the occurrence of intense pain with a slight pressure force (on average 4–5 lb/sm2) at standard points. A study was carried out on the microelement composition of hair, psychological and vegetative testing. The results showed that the patient had an established magnesium deficiency (the magnesium content in the hair biopsy, the microelement level was 26 mcg/g, with a norm of 50 mcg/g) was accompanied by a psychovegetative syndrome in the form of anxiety (16 points on the hospital anxiety scale with a norm of up to 7 points), asthenia (33 points on the activity scale with a norm of 50 points), sleep disturbance (16 points on the night sleep quality scale with a norm of 22 points), a decrease in quality of life by 35%. Autonomic dysfunction was manifested in increased activity of the sympathetic-adrenal system at rest and insufficient activation of functional reserves when test loads were presented. Based on the obtained clinical and paraclinical data, the patient was diagnosed with psychovegetative syndrome. Astheno-neurotic syndrome. The patient was prescribed a 2-month course of Magne B6 therapy at a dose of 1 ampoule of a drinking solution 3 times a day for 2 weeks, followed by a transition to taking 1 ampoule 2 times a day with meals. After 2 months of regular use, the patient’s condition improved, complaints were reduced. The patient became more active, her sleep and emotional background normalized, she became less sensitive to weather changes, sweating decreased, and muscle pain stopped bothering her. Objectively: against the background of an increase in magnesium content in the body to 47 mcg/g, positive dynamics of psycho-vegetative indicators were noted. Levels of anxiety and asthenia did not exceed standard values. The quality of night sleep, neuromuscular excitability and pain sensitivity threshold were restored. Indicators of autonomic tone did not differ from those of practically healthy people. When conducting an active orthotest, insufficient activation of adaptive mechanisms still remained, but there was already a tendency towards the adequacy of vegetative support. The patient's quality of life improved. Discussion. This clinical case illustrates the formation of astheno-neurotic manifestations of magnesium deficiency in a patient initially belonging to the asthenic type of people. Low constitutional functional activity of the body systems, combined with the developed energy deficiency against the background of stressors, led to the predominance of asthenic manifestations of psychovegetative syndrome. The use of a magnesium-containing drug made it possible to improve energy metabolism - a basic characteristic of the body's metabolism, which contributed to the improvement of vegetative status and maintenance, as well as the normalization of psycho-vegetative relationships and increased activity of the patient. Thus, the clinical cases presented demonstrate the importance of magnesium as a mineral that regulates the activity of the nervous system, its necessity in regulating optimal metabolism and the functioning of the body. However, the magnesium content in modern human food is decreasing. Reduced levels of the microelement were also found in people with certain chronic somatic and mental illnesses. All this showed the need to increase awareness of the importance of magnesium intake and its potential therapeutic role in a range of diseases. In their practice, doctors are already faced with clinical manifestations of established magnesium deficiency. Research in recent years shows the effectiveness of magnesium in neurological and mental pathologies, eclampsia and preeclampsia, arrhythmia, severe asthma and migraine. Magnesium-containing therapy has demonstrated promising results in reducing the risk of metabolic syndrome and insulin resistance, improving metabolism, reducing symptoms of dysmenorrhea, and reducing leg cramps in pregnancy. Because magnesium is excreted through the kidneys, it should be used with caution in patients with kidney disease. However, long-term intake of magnesium citrate helps to normalize the metabolism of purines and oxalates, which is used in the prevention and treatment of metabolic disorders. To prevent magnesium deficiency, it is recommended to include green leafy vegetables, nuts, legumes, and whole grain products in the diet [9]. In cases of established magnesium deficiency or in patients with symptoms similar to those described by us, it is recommended to supplement magnesium with bioorganic salts (lactate, pidolate or citrate), which have a high degree of absorption by the human body [4].
Literature 1. Pathophysiology. Lecture course; Textbook/P.F. Litvitsky, N.I. Losev, V.A. Voinov and others; Ed. P.F. Litvitsky.– M., 1995.–752 p., ill. 2. Spasov A.A. Magnesium in medical practice, Volgograd, 2000, 268 pp. 3. Durlach J, Bac P, Durlach V, Bara M, Guiet–Bara A. Neurotic, neuromuscular and autonomic nervous form of magnesium imbalance. //Magnes Res. 1997 Jun;10(2):169–95. 4. Gromova O.A. Magnesium and pyridoxine: basic knowledge, M.:, 2006, 223s 5. Jacka FN, Overland S, Stewart R, Tell GS, Bjelland I, Mykletun A. Association between magnesium intake and depression and anxiety in community–dwelling adults: the Hordaland Health Study. //Aust NZJ Psychiatry. 2009 Jan;43(1):45–52 6. Eby GA 3rd, Eby KL. Magnesium for treatment–resistant depression: a review and hypothesis. //Med Hypotheses. 2010 Apr;74(4):649–60 7. Nechifor M. Magnesium in major depression. // Magnes Res. 2009 Sep;22(3):163S–166S 8. Vorobyova O.V., Akarachkova E.S. Magne B6: experience of 5 years of clinical use in neurological and therapeutic practice // Farmateka 2008 No. 20 P. 73–80 9. Guerrera MP, Volpe SL, Mao JJ. Therapeutic uses of magnesium. //Am Fam Physician. 2009 Jul 15;80(2):157–62 RU.MGP.10.09.16