Why are platelets in the blood determined in adults and children?
Platelet functions
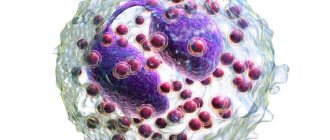
Platelets belong to the formed elements of blood in the same way as erythrocytes and leukocytes.
The difference from them is that red and white blood cells have a cellular structure. Platelets are a kind of plates that do not have a nucleus. They are smaller in size than a red blood cell. In the blood, platelets are formed from a large precursor cell, the megakaryocyte.
Inside these blood cells there are substances that are stored in the form of granules. Due to these compounds, platelet functions are ensured.
The main function of blood platelets is to stop bleeding. The size of the vessel does not matter much: in small ones a plug is formed, and in large ones a clot of fibrin is formed.
That is, when the vessel wall is damaged, platelets protrude processes, facilitating the interaction of the plates with each other. Activated platelets release various clotting factors, triggering the process of clot formation from fibrin monomers.
In addition to participating in blood clotting processes, these formed elements have other functions:
- releasing biologically active substances, they contribute to the narrowing of the lumen of the vessel;
- regulate the permeability of the vascular wall for various compounds;
- indicate the place of attachment of the fibrin clot to the vessel wall;
- activate compounds that prevent the formation of a blood clot or promote clot splitting;
- support the structure and functions of the vascular wall;
- Platelet growth factors promote the movement of endothelial and smooth muscle cells, performing a so-called reparative function.
Platelets are synthesized in the bone marrow, then released into the bloodstream, where they remain for about a week and then die.
Norm of platelets in the blood of children
In children, the platelet count that should be normal is slightly different from the level in adults. In newborns, the norm is considered to be from 100 to 400 * 10 * 9 per liter. Then, up to a year, their content increases slightly: the lower limit of the norm is considered to be 150 * 10 * 9 per liter. Then the level of platelets in the blood reaches 180 - 320 *10*9 per liter.
Normal in adults
The normal level of platelets in the blood of an adult is 180 – 400 *10*9 per liter. Thus, as children grow older, the normal content of platelets in children reaches the level of adults.
Normal for pregnant women
In connection with the birth of the fetus, the mother's body has to rebuild. Therefore, a decrease in platelet levels in a pregnant woman is considered normal. For example, the normal level of blood platelets in the first trimester is considered to be 170 - 340 * 10 * 9 per liter.
Considering the important functions platelets perform, it is necessary to monitor their levels during pregnancy.
Deviations
Minor deviations, within 5-10 units, should not alarm parents. A similar situation is possible against the background of changes in the biochemical composition of the blood and the functioning of enzymatic systems due to the emotional stress of the child before taking blood. As a rule, babies are afraid of venipuncture and may cry a lot. You should try to calm the child as much as possible and collect blood only after 15 minutes of rest.
To confirm the results, it is recommended to repeat the study - 3 times with a three to five day interval. In case of consistently minor or one-time strong deviations, additional studies are prescribed in order to establish the exact cause. Let's consider the main reasons why the indicator in question deviates from acceptable values.
Exceeding the norm
Main article: About the causes of thrombocytosis (increased platelets) in children
The most alarming causes of increased platelets in children include blood diseases. For example, leukemia or essential thrombocytosis.
Secondary forms of thrombocytosis arise as a result of the manifestation of pathologies that are not associated with the hematopoietic system. These include mechanical injuries, malignant neoplasms, bleeding and acute forms of infectious diseases.
Please note that platelet levels increase with blood loss, severe emotional stress or intoxication. The fact is explained by the fact that the hematopoietic systems try to compensate as much as possible for the loss of blood and its formed elements, beginning to intensively synthesize them. Therefore, on the first day, a significant excess of the norm is recorded.
What additional tests will be required to clarify the reasons for the increase in platelet levels in the child’s blood? In this case, it is advisable to conduct an ultrasound examination of the abdominal and pelvic organs, a laboratory test to determine the level of C-reactive protein, iron, a coagulogram, a biochemical blood test and a general urine test.
In what diseases does the platelet count in the blood change?
Increasing
A high number of platelets in the blood can trigger the formation of clots, then blood clots in the vessels, which will lead to disruption of blood flow through them.
The reasons for a high concentration of blood platelets may be:
- neoplasms in the place of synthesis and maturation of all formed elements - the bone marrow;
- polycythemia is a disease that is accompanied by an increase in the number of all blood elements, including platelets;
- the presence of an infectious process in the body;
- there is no possibility of old plates being destroyed due to the absence of an organ (spleen) where this happens to them;
- kidney dysfunction;
- autoimmune pathology;
- with loss of large volumes of blood. This gives impetus to the synthesis of new cells and in large quantities to replenish what was lost.
Thus, a high platelet count in the blood is dangerous due to the occurrence of thrombosis.
Decreases
A decrease in the number of blood platelets can lead to serious consequences, including death. Therefore, it is impossible to allow a decrease in the level of formed elements.
A lack of platelets in the blood can lead to bleeding. It will also be difficult for the body to stop it. And a person can die from blood loss.
Therefore, if a small number of platelets is detected, it is necessary to find out what could lead to this.
A low platelet count is commonly called thrombocytopenia.
Thrombocytopenia may be caused by:
- increased destruction of these formed elements in the spleen;
- disruption of their synthesis in the bone marrow;
- infectious process;
- oncological diseases;
- the appearance of antibodies - specific molecules to platelets, which contribute to their rapid destruction, reducing their lifespan.
Uncontrolled use of blood thinners can lead to low platelet levels.
Thrombocytosis in children
Thrombocytosis is an increase in the number of platelets in the blood to values several times higher than normal. Most often, thrombocytosis is a consequence of a viral or bacterial infection. In particularly severe cases, an increase in blood cells may indicate the development of cancer.
How to determine: symptoms
The symptoms of thrombocytosis are similar to the clinical manifestations of thrombocytopenia, although there are still some differences. If a child has at least one of the listed signs, you should immediately consult a doctor and take a blood test.
Symptoms of thrombocytosis in childhood:
- frequent and severe nosebleeds;
- blue skin;
- the appearance of subcutaneous hemorrhages;
- itching and burning in certain areas of the skin;
- tingling sensation on the skin;
- cold hands and feet at a comfortable ambient temperature;
- dyspnea;
- increased heart rate.
The child may also complain of frequent headaches. In some cases, pressure surges and blood clots may form.
Causes
To correctly determine the cause of the increase in platelets, it is necessary to diagnose what type of thrombocytosis is developing in the child. The treatment regimen and tactics for managing a small patient will depend on this.
- Platelets: normal for women by age (table). What determines the platelet count in the blood?
| Type of thrombocytosis | Causes |
| Clonal | Bone marrow stem cell defects |
| Primary | Pathologies in the functioning of bone marrow cells, the formation of several sites of hematopoiesis |
| Secondary |
|
Recommendations for thrombocytosis
- Consult your doctor about the use of products that contain acetylsalicylic acid (for thinning the blood).
- During the day, offer your child compotes and fruit drinks made from blueberries, lingonberries and cranberries as often as possible.
- Monitor the iodine content in the body, and if there is a deficiency, ensure sufficient consumption of fish and seafood.
- If the child does not have problems with the gastrointestinal tract, it is recommended to add fresh garlic and ginger (in minimal quantities) to food.
- In the morning, you can give your baby cocoa without sugar (a prerequisite is that the drink must be consumed on an empty stomach).
- Olive and flaxseed oils, as well as foods rich in magnesium and B vitamins, should be mandatory products in a child’s diet for thrombocytosis.
- Avoid dehydration (the water norm for a child is 1 liter per day).
- Increase the amount of fruits and vegetables (tomato juice and lemons are especially useful).
What affects the platelet count in a healthy child?
Before the analysis, it is advisable not to take risks and not to overload the child with physical activity, to avoid injury. Emotional calm is also important.
A child's diet can also affect platelet levels. It is recommended to exclude fatty and smoked foods. Switch to a healthier diet.
Be careful with foods rich in vitamin C. They can thin the blood and change the level of detectable blood elements.
You should not take any medications on your own. Any medications should be prescribed only by a pediatrician or other doctor.
Causes of elevated platelets
A condition in which the content of blood platelets is higher than normal is called thrombocytosis. More often adults are susceptible to it, but it can also occur in children, and even lead to thrombus formation and blockage of blood vessels. As a rule, there are no specific signs of thrombocytosis. Children usually complain of headaches and general weakness, but such symptoms are characteristic of many other diseases. Thrombocytosis can have different origins:
- Primary develops with congenital or acquired blood diseases, such as thrombocythemia, myeloid leukemia, erythremia and others.
- Secondary thrombocytosis is caused by infectious diseases, including pneumonia, toxoplasmosis, hepatitis, and meningitis. At the same time, the body increases the production of blood platelets to quickly suppress the infection. An increase in white blood cell levels is usually observed at the same time.
Thrombocytosis in children is often associated with infectious diseases
Secondary thrombocytosis can occur under severe stress, after infectious diseases, after taking medications, after surgery, especially after removal of the spleen, one of the functions of which is the destruction of spent blood platelets.
Thus, the causes of thrombocytosis can be different, but, as a rule, it is a sign of pathology. If the analysis shows that platelets are elevated, this may indicate certain diseases and conditions, including:
- iron deficiency anemia;
- pulmonary tuberculosis;
- acute rheumatic fever;
- ulcerative colitis;
- malignant tumors at the stage of formation of secondary foci;
- condition after removal of the spleen;
- taking certain medications;
- condition after prolonged bleeding;
- condition after surgical interventions.
Methods for determining the level of platelets in the blood
The study of the content of blood platelets is one of a number of indicators that are determined in a general clinical blood test. In a modern laboratory, this analysis is performed on an automatic hematology analyzer. As a rule, cell counting errors are kept to a minimum. But there are situations when a clot forms in the sample, which makes it impossible to count these plates.
The material for determining the level of blood platelets is blood taken from a vein or from a finger.
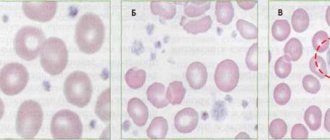
The solution in this situation is to count platelets manually. That is, a blood smear is prepared, it is painted with special dyes so that the plates are visible. After all the manipulations, the smear is examined under a microscope. 1000 red blood cells are counted, and in parallel, how many platelets were observed are noted. After which the calculation is made.
How is platelet count determined?
The platelet count is assessed using a clinical blood test. All doctors call this study the most important in childhood. To carry it out, the child’s blood can be taken from a finger, as well as from a vein. For the youngest children, blood can be drawn from the heel. Platelets are counted per liter of blood, indicating them in the analysis form as 109/l.
A blood test can be prescribed to a child as planned, even if he does not have any complaints.
An unscheduled referral for analysis is given to children who experience bleeding gums, episodes of nosebleeds, prolonged bleeding after a cut, frequent bruising, complaints of fatigue, pain in the limbs and other ailments.
Also, platelets must be checked in case of anemia, enlarged spleen, leukemia, viral infections, systemic and other diseases that can provoke a change in the number of these blood cells.
How to lower platelets?
Treatment for thrombocytosis depends on the cause of its development. If it is caused by another disease, then it needs to be treated. After the disease is eliminated, platelets will return to normal.
If they are elevated due to hematopoietic disorders, drugs are prescribed that reduce the production of blood platelets and promote blood thinning.
With thrombocytosis, the blood becomes viscous, and there is a risk of blood clots even in young children. If your platelet count is significantly elevated, you may not need medical treatment. In this case, it is necessary to take anticoagulant drugs. In addition, it is recommended to change your diet. Doctors advise including the following foods on the menu:
- grenades,
- lemons,
- beets,
- garlic,
- sea buckthorn,
- viburnum,
- cranberries
If the child’s platelets are high, the child’s diet should contain as many healthy foods as possible, vegetables, berries, fruits, garlic, onions, etc.
If the platelet level is slightly elevated, and no diseases have been diagnosed, as a rule, no medications are prescribed. In this case, a special diet is of great importance. It is necessary to exclude all foods that can worsen the condition and eat only healthy foods. Doctors advise adhering to the following rules:
- Increase the amount of liquid you drink, but not carbonated drinks, but green tea, juices from berries (preferably sour ones), fruits, and vegetables. Drinking regimen during thrombocytosis is very important, since an insufficient amount of fluid leads to dehydration, the blood vessels narrow, and the blood thickens even more, which leads to a deterioration in the child’s condition.
- Avoid spicy, fatty, fried and smoked foods.
- Avoid foods that increase blood clotting. These include walnuts, bananas, lentils, chokeberries, pomegranates, and mangoes.
- Vegetables and fruits should always be present on the table; preference is given to blue and red fruits.
- Give your child foods that thin the blood: sour berries, onions, olive and flaxseed oil, fish oil. For high platelet counts, garlic is especially effective, as it thins the blood and dissolves existing blood clots.
- It is necessary to use caution with medications that can thicken the blood. If treatment with such medications is required, you should consult your doctor.
- Temporarily avoid animal foods (with the exception of dairy products).
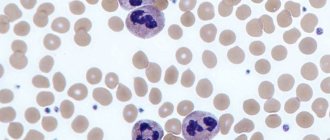
Theoretical and clinical aspects of thrombocytopenia in newborns
Thrombocytopenia includes conditions in which the number of peripheral blood platelets is less than 150 × 109/L. This is a fairly common hematological syndrome in the neonatal period. In 1–5% of children, thrombocytopenia is registered at birth, but in only 0.1–0.5% of newborns it is severe (platelet count less than 50.0 × 109/L) [1, 2]. In approximately half of cases, thrombocytopenia manifests itself as hemorrhagic syndrome.
The causes of thrombocytopenia in newborns are highly variable [3]. These may be primary thrombocytopenias, which, as a rule, are based on immunopathological processes. Secondary (symptomatic) thrombocytopenia occurs against the background of various conditions, among which more often viral or bacterial infections, severe hypoxic manifestations, immunodeficiency states, intravascular coagulation syndrome, etc. All forms of thrombocytopenic purpura, according to the mechanism of occurrence, are acquired, even in cases of birth of a child with clinical picture of thrombocytopenic purpura.
The mechanisms of development of thrombocytopenia in the neonatal period are different. Among them are:
1. Increased destruction of platelets - as a result of immune processes:
a) isoimmune (alloimmune) thrombocytopenic purpura. The development of this disease is similar to hemolytic disease, however, the immunological conflict is caused by the incompatibility of the fetus and mother in platelet antigens (most often the PLA1 antigen, which is absent in the mother). Antiplatelet antibodies appear in the sensitized maternal body, which, penetrating the placenta, cause the destruction of platelets in the fetus. Isosensitization can occur both during the second and during the first pregnancy. Occurs with a frequency of 1 case per 1000 newborns [4]; b) transimmune thrombocytopenic purpura develops in children born to mothers suffering from autoimmune thrombocytopenia. This happens with idiopathic thrombocytopenic purpura, systemic lupus erythematosus, autoimmune thyroiditis, Evans syndrome, etc. Maternal autoantibodies penetrate the placenta and cause the destruction of platelets in the fetus. Since after the birth of a child the penetration of antibodies from mother to child stops, this form of the disease has a favorable prognosis.
Mechanical destruction of platelets as a result of their increased consumption in cavernous vascular formations occurs in Kasabach-Merritt syndrome.
2. Increased consumption of platelets in intravascular coagulation syndrome, artificial ventilation, hemolytic-uremic syndrome.
3. Insufficient production of platelets - a-, hypomegakaryocytosis. There are exclusively amegakaryocytic thrombocytopenias, which are not combined with any other types of pathology. Hypomegakaryocytoses are combined either with absent radius syndrome (TAR syndrome), or with other bone and organ defects and dysplasias. Pancytopenia - when a-, hypomegakaryocytosis is combined with aplasia of other hematopoietic germs, with various pigmentation disorders, congenital anomalies of the skeleton, eyes, ears, heart.
In addition to the above mechanisms and forms of the disease, heteroimmune thrombocytopenia is distinguished, in which antibodies are produced against a foreign antigen located on the surface of platelets. Examples of foreign antigens are drugs and viruses. It is also possible to develop thrombocytopenia as a result of changes in the antigenic structure of platelets, under the influence of viral exposure. After the medicine is removed from the body or the viral infection is recovered, the signs of the disease disappear and the patient recovers.
A number of toxic and dosage forms used by pregnant women also contribute to the development of thrombocytopenia in newborns. These include alcohol, thiazide drugs, hydralazine, sulfonamides, furazolidone, phenylbutazone, estrogens, heparin therapy, etc.
The mechanism of development of thrombocytopenia during intrauterine infections is quite complex and is associated with insufficient production of platelets by the bone marrow, inhibition of the megakaryocyte lineage by pathogen toxins, hypersplenism, and disseminated intravascular coagulation syndrome.
The diagnostic search algorithm in case of detection of thrombocytopenia in a newborn includes:
1) collection of anamnestic data: the mother has autoimmune thrombocytopenia (idiopathic thrombocytopenic purpura, systemic lupus erythematosus, autoimmune thyroiditis, Evans syndrome, etc.); abnormalities of the placenta (chorioangiomatosis, abruption, thrombosis), use of medications. The newborn has a premorbid background (hypoxic conditions, prematurity, intrauterine growth retardation (IUGR), postmaturity, etc.); the presence of an underlying disease (intrauterine infection, immunodeficiency conditions, giant hemangioma, etc.);
2) determination of the nature of thrombocytopenia - primary or secondary;
3) study of clinical data: hemorrhagic syndrome in the first days of a child’s life in the form of skin manifestations (petechiae, ecchymosis), bleeding from the microvasculature (nasal, gingival, etc.), bleeding from the umbilical cord, melena. Hemorrhagic syndrome with thrombocytopenia is characterized by spontaneity, asymmetry, polymorphism and polychrome. The localization of hemorrhages in the sclera and conjunctiva should be regarded as a prognostically unfavorable sign in terms of the occurrence of hemorrhages in the brain. In the transimmune form, the hemorrhagic syndrome gradually declines, since the supply of antiplatelet antibodies to the child from the mother stops and platelet destruction does not occur [5]. In the case of secondary thrombocytopenia, hemorrhages develop against the background of the underlying disease; a characteristic symptom is hepatoslenomegaly. The severity of hemorrhagic syndrome in newborns with TORCH infections depends not only on the pathogen, but also on the gestational age at which the fetus was exposed to the infectious agent. Kasabach–Merritt syndrome is characterized by the development of neonatal melena;
4) assessment of laboratory parameters. The presence of thrombocytopenia is indicated by:
- the number of platelets in peripheral blood is less than 150 × 109/l against the background of normal other indicators;
- increase in duration of bleeding according to Duque more than 4 minutes;
- reduction in blood clot retraction less than 60%;
- hyperplasia of the megacryocyte lineage (more than 54–114 in 1 μl) in the myelogram;
- absence of deviations in laboratory tests characterizing the coagulation link of hemostasis.
The detection of antiplatelet antibodies confirms the immune nature of the disease. Detection of a diagnostically significant increase in antibody titer to any pathogen (cytomegalovirus (CMV), Epstein-Barr virus, rubella virus, herpes simplex, etc.) confirms the secondary nature of thrombocytopenia (heteroimmune forms of the disease).
Only consistent and thorough conduct of all stages of the diagnostic search allows the doctor to obtain a clear understanding of the processes occurring in the child’s body and develop the correct treatment tactics.
The presence of hemorrhagic syndrome, regardless of the nature of thrombocytopenia (primary or secondary), makes the relief of hemorrhagic manifestations the basis of treatment measures.
For immune thrombocytopenia in the case of a mild disease accompanied only by skin syndrome. The drugs of choice are angioprotectors - etamsylate 12.5% solution 0.1 ml/kg IV or IM 2-4 times a day or 500 mg 4-6 times a day orally. The pharmacological effect of the drug is associated with increasing the stability of capillaries, reducing their permeability, improving microcirculation, as well as stimulating the formation of blood coagulation factor III and normalizing platelet adhesion [6]. Fibrinolysis inhibitors - epsilon-aminocaproic acid at a dose of 50 mg/kg intravenously once a day. Its action is based on inhibiting the activating effect of streptokinase, urokinase and tissue kinases on fibrinolysis, neutralizing the effects of kallikrein, trypsin and hyaluronidase, and reducing capillary permeability [6]. Suppression of the immunopathological process is achieved by using glucocorticoids - prednisolone at a dose of at least 2 mg/kg per day in two doses. Alternative therapy is possible - normal human immunoglobulins (Immunovenin, Pentaglobin, Octagam) at a dose of 0.4 g/kg per day IV for 5 days. The positive effect of immunoglobulins is due to the blockade of Fc receptors of macrophages, which reduces opsonization of platelets and prevents their destruction in the bloodstream. The use of immunoglobulins allows you to obtain a faster (after 24–48 hours), but less lasting effect than with the use of glucocorticoids. Therefore, they often resort to the combined use of these drugs. However, according to foreign authors, the use of prednisolone and immunoglobulins in the alloimmune form of the disease remains controversial [7, 8].
In case of life-threatening bleeding, the use of platelet concentrate is indicated. Its use requires a careful and balanced approach, since in immune forms, transfusion of platelet concentrate is contraindicated, since its use can further aggravate the process due to excessive formation of antibodies. The indication for platelet transfusion is a platelet count of less than 20/nl without signs of bleeding and less than 30/nl with signs of bleeding [7]. The estimated dose for transfusion of platelet concentrate is 10 ml/kg, however, the optimal dose can be obtained by performing an individual mathematical calculation in terms of one of the parameters (body weight, circulating blood volume, body area). After transfusion, platelet levels must be monitored. The clinical criterion for the effectiveness of transfusions of platelet concentrate is the relief of hemorrhagic syndrome, an increase in the patient’s platelet count 1 hour after transfusion by at least 50–60 × 109/l and retention of the result after 24 hours.
In case of secondary thrombocytopenia, it is necessary to treat the underlying disease, since the prognosis is determined precisely by its course.
Thus, the diagnosis of thrombocytopenia in newborns is a very complex process, the competent implementation of which largely determines the success of therapeutic measures, and therefore the prognosis and quality of life of the patient.
We present our own clinical observation of a newborn diagnosed with isoimmune thrombocytopenic purpura, which was diagnosed in a child with a concomitant disease - congenital heart disease.
Georgy V., was admitted to the department for newborn children of the Municipal Children's Hospital of Belgorod on the 8th day of life from the maternity hospital.
Anamnesis of life. From the first pregnancy, it occurred against the background of candidal colpitis. Examination for prenatal infections, IgG antibodies to herpes simplex virus type 1 were detected. Delivery at term, birth weight 3060 g, length 53 cm. Attached to the breast immediately, suckling actively. At birth, multiple elements from petechiae to ecchymoses, sometimes confluent, were noted on the skin. In the early neonatal period, physiological jaundice appeared on the third day of life, the level of total bilirubin was 170 µmol/l, glucose - 4.3 mmol/l, C-reactive protein (CRP) less than 5 ng/ml. The maximum loss of initial body weight was 8.5%; the umbilical remnant fell off on the fourth day of life. Mild neurological symptoms were noted in the form of decreased reflex activity and muscle hypotension. Hemogram on the first day of life: hemoglobin 150 g/l, erythrocytes - 4.6 × 1012/l, color index - 0.9, leukocytes - 9.4 × 109/l, band neutrophils - 3%, segmented neutrophils - 65%, lymphocytes - 27%, monocytes - 4%, eosinophils - 1%. ESR 3 mm/hour. During the early neonatal period, cutaneous hemorrhagic syndrome persisted and tended to intensify in the form of the appearance of new elements. Treatment was carried out: etamsylate, menadione sodium bisulfite (Vikasol), phototherapy. Due to the lack of positive dynamics, the child was transferred to the second stage of treatment.
On admission. The condition is serious. The skin is pale pink, acrocyanosis, periorbital cyanosis at rest, hemorrhages throughout the body from small punctate to ecchymoses 3–4 cm in diameter, polychrome. The mucous membranes of the palate, pharynx, conjunctiva, and sclera are clean. On the part of the internal organs: breathing through the nose is free, upon auscultation, puerile breathing is performed over the entire surface of the lungs, there are no wheezes, percussion - a box-shaped percussion sound, respiratory rate is 45 per minute. The area of the heart is not visually changed; upon auscultation, the heart sounds are muffled, the rhythm is preserved, the heart rate is 123 per minute. The abdomen is soft on palpation, the liver is at the edge of the costal arch, the spleen is not palpable. The umbilical area is without features. Stool and diuresis are not disturbed. Over the next three days, the same condition remained: there were multiple hemorrhages on the torso, including “fresh” ones, and the appetite was reduced. From the side of the heart, upon auscultation in the second intercostal space on the left of the sternum, a systolic murmur of moderate intensity was heard. Liver +3.5 cm from under the edge of the costal arch, spleen +1.0 cm. Body weight 2850 g.
Examination. The dynamics of hemogram results are presented in the table.
The ESR did not exceed 6 mm/hour throughout the hospitalization. Urinalysis without deviations from the norm (five times). In a biochemical blood test, the level of CRP is less than 10 ng/ml, liver tests are normal, moderate hypoproteinemia. Enzyme-linked immunosorbent assay (ELISA) for specific antibodies to CMV antigens - negative, ELISA for specific antibodies to Ebstein-Barr virus antigens - negative, ELISA with herpes viruses type 1, 2 - IgM - negative, IgG - positive, avidity index 72 %. ELISA for specific antibodies to chlamydial antigen - negative, ELISA with mycoplasma antigen - negative, ELISA for toxoplasma antigen - negative. In the coagulogram: prothrombin test - international normalized ratio (INR) - 1.0, prothrombin index (PTI) - 100%, prothrombin time - 15.3 seconds; fibrinogen - 1.62 g/l, thrombin time - 16 seconds. Myelogram on the 14th day of life (5th day of hospitalization): blast cells 0.5%, neutrophil maturation index - 1.0, erythrokaryocyte maturation index - 0.8, leukoerythroblastic ratio - 1.3: 1.0 (normal 2.1:4.5). Conclusion: the type of hematopoiesis is normoblastic. The lacing of platelets is weakly expressed; there are many megakaryocytes of varying degrees of maturity.
A blood test of the mother did not reveal any abnormalities in the hemogram.
The electrocardiogram shows signs of hypertrophy of the right ventricle and interventricular septum. ECHO-CG study: additional trabecula of the left ventricle, atrial septal defect of 6 mm, and blood discharge from left to right were detected. The contractility of the ventricular myocardium is satisfactory, the ejection fraction is 68%. Ultrasound of the abdominal organs: liver 53 mm, homogeneous structure. The spleen measures 44 × 26 mm, the structure is homogeneous. Kidneys: on the left - pelvis 7 mm, size 46 × 21 mm, on the right - size 45 × 22 mm. Neurosonography: hypoxic changes and signs of immaturity of brain structures.
Treatment was carried out: etamsylate 12.5% solution 12.5 mg/kg IV 4 times a day for 14 days, normal human immunoglobulin 400 mg/kg/day IV for 6 days, prednisolone 2 mg/kg/day orally for 7 days , fresh frozen plasma 10 ml/kg IV twice, pentoxifylline 0.1 ml/kg IV, inosine 10 mg/kg IV, furosemide 1 mg/kg/day IV, levocarnitine 75 mg 3 times a day orally, recombinant human interferon alpha-2 150,000 2 times a day. The child was fed with human milk substitutes and breastfed from the sixth day of hospitalization. During treatment, by the fifth day of hospitalization, the platelet count increased sevenfold, and the cutaneous hemorrhagic syndrome did not recur. The child was discharged in satisfactory condition on the 26th day of life (18th day of hospitalization).
Thus, this clinical example demonstrates the difficulty of interpreting clinical and laboratory parameters in children of the neonatal period. Laboratory diagnosis of immune thrombocytopenia in many medical institutions in our country is not yet sufficiently developed. Only a clear diagnostic search algorithm will allow the doctor to quickly and clearly assess the variety of causes leading to the development of thrombocytopenia in newborns and promptly and correctly prescribe adequate therapy. Therefore, dissemination of information about the pathogenesis and existing methods for studying various forms of immune thrombocytopenia and the introduction of these methods into clinical practice is a necessary condition for improving diagnosis and increasing the effectiveness of treatment of these diseases.
Literature
- Maschan A. A., Rumyantsev A. G. Immune-mediated thrombocytopenia in newborns: differential diagnosis and principles of therapy // Issues of hematology/oncology and immunopathology in pediatrics. 2010, vol. 9, no. 3, p. 13–18.
- Pshenichnaya K.I. Congenital thrombocytopathies in children: features of diagnosis, symptoms and treatment: Abstract of thesis. diss. Dr. med. Sci. St. Petersburg, 2002. 28 p.
- Shabalov N.P. Neonatology: Textbook. allowance. T. 2. M.: MEDpress-inform. 2004. 640 p.
- Durand-Zaleski I., Schlegel N., Blum-Boisgard C. et al. Screening primiparous women and newborns for fetal/neonatal alloimmune thrombocytopenia: a prospective comparison of effectiveness and costs. Immune Thrombocytopenia Working Group // Am J Perinatol. 1996; 13 (7): 423–431.
- Golovko O.K., Linchevsky G.L., Vorobyova O.V. Clinical aspects of immune thrombocytopenia in neonatology // Child’s Health. 2006. No. 2. pp. 115–122.
- Register of medicines. M.: RLS-2005. 1440 pp.
- Rooz R. Neonatology. Practical recommendations: trans. with him. M.: Med. lit. 2011. 592 p.
- Berkowitz RL, Kolb EA, McFarland JG et al. Parralel randomized trials of risk-based therapy for fetal alloimmune thrombocytopenia // Am. J. Obstet Gynecol. 2006; 107(1):91–96.
N. M. Sudakova*, Doctor of Medical Sciences, Professor N. I. Grevtseva** O. M. Zubov** O. V. Lazareva**
* Belgorod State University, ** Municipal Children's Hospital, Belgorod
Contact information for authors for correspondence
Primary thrombocytopenia
Acute thrombocytopenic purpura is an autoimmune disease, the causes of which are unknown. Most often it is observed in children from 2 to 6 years old. It usually occurs after vaccination or a viral infection. The disease develops rapidly, and hemorrhagic manifestations are immediately observed:
- Both pinpoint and larger elements (petechiae and ecchymoses) appear on the skin;
- hemorrhages on the body can have different colors - from purple-violet to greenish;
- new elements appear suddenly;
- there is no specific localization, hemorrhages are located asymmetrically.
The acute phase of the disease is characterized by nosebleeds, as well as bleeding after tooth extraction; in the puberty period in girls - uterine bleeding. In severe cases, bleeding from the gastrointestinal tract is possible, as evidenced by blood in the stool. In some cases, hematuria (the presence of blood in the urine) and hemorrhages in the mucous membranes are observed. Sometimes hemorrhages occur in internal organs, in the retina, and in the brain. Some children have an enlarged spleen.