The postpartum period is probably the most beautiful and most awaited time for every woman. Due to the fact that the body undergoes many changes at this stage, the expectant mother should be regularly examined by a specialist.
The most common procedure is a general blood test. One of the most important indicators is platelets during pregnancy.
This examination is necessary for the early detection of abnormalities that are dangerous not only for the woman, but also for her unborn child.
Description of cells
Platelets are very thin discs that help blood clot. Their peculiarity is the ability to stick together when a cut or wound forms.
As a result of this process, clots are formed that block the blood vessels and prevent large amounts of blood from leaking out. Against this background, a crust appears on the surface of the skin. If it is removed, bleeding may resume.
In addition, platelets perform a protective function, protecting the body from the penetration of pathogenic bacteria and viruses.
They contribute to the formation of the immune system and are regularly updated.
The number of platelets in the blood is a temporary indicator. It is constantly changing depending on the influence of internal and external factors. For example, it changes during pregnancy and during the menstrual cycle.
Decoding indicators
A description of the results is given by a geneticist.
A genetic blood test for the presence of polymorphisms in the prothrombin (F2) and Leiden factor (F5) genes reveals the patient's predisposition to thrombosis.
Genetic polymorphism, or genetic diversity, is different variations of genes. The presence of gene polymorphism explains disturbances in the structure and properties of those proteins that are produced in the body. With genetic polymorphism, changes in the function of synthesized proteins can be beneficial for the body, neutral or negative.
The F2 gene encodes the amino acid sequence of the protein prothrombin (a protein called blood clotting factor II, which is produced in the liver and is a precursor to thrombin). The presence of polymorphisms in the F2 gene leads to an increase in prothrombin several times, which increases the risk of venous thrombosis, including thrombosis of the brain and heart, especially at a young age. The mutation has an autosomal dominant type of inheritance, so even a heterozygous carrier of the altered gene suffers from thrombophilia. Patients who carry this altered gene have an increased risk of developing fetoplacental insufficiency, placental abruption, fetal growth retardation, fetal loss in the first trimester of pregnancy, and the development of thromboembolism after surgical interventions. Taking oral contraceptives in this group of people also increases the risk of thrombosis.
The F5 gene encodes the amino acid sequence of the protein proaccelerin - coagulation factor V, which is synthesized in the liver, participates in the blood coagulation cascade, and activates the transition of prothrombin to thrombin. A change in the gene (replacement of arginine with glutamine at position 534 - “Leiden mutation”) makes the active form of coagulation factor V resistant to cleavage, which is manifested by recurrent venous thrombosis and thromboembolism. The presence of the mutation increases the risk of venous thrombosis by more than 3 times. Taking oral contraceptives increases this risk by more than 30 times. The risk of myocardial infarction increases by more than 2 times, the risk of developing pregnancy pathologies (miscarriage, preeclampsia, chronic placental insufficiency and fetal growth restriction syndrome) increases by more than 3 times.
Patients who are carriers of both the prothrombin gene mutation and the Leiden mutation are even more at risk of developing thrombosis and thromboembolism.
The indicator is normal
The platelet count in a pregnant woman is an important indicator that should always be monitored. It may decrease during pregnancy due to an increase in blood volume and the formation of a placental circle of blood flow. The average volume considered normal in pregnant women is about 140-340 thousand/mcL.
This number depends on when you became pregnant. The normal platelet count in the blood is:
- I trimester - 170-340 thousand / microliter;
- Second trimester - 160-330;
- 2nd trimester - 160-330; III trimester - 140-320.
After childbirth, a woman's body undergoes some changes, the main purpose of which is to reduce blood loss. This is due to increased blood clotting. After the end of the postpartum period, all indicators return to normal.
Clinical and laboratory features during pregnancy
Pregnancy
is the period of time during which the fetus develops inside a woman's uterus, ending with the birth of the child.
During pregnancy, numerous physiological changes occur to meet the needs of the growing fetus and the mother's body, which adapts to them. Most of these changes begin soon after conception and continue until late pregnancy. Physiological adaptation is reflected in changes in the values of laboratory parameters. Some of the changes are well known, for example, a decrease in hematocrit and hemoglobin, creatinine; others, on the contrary, are known to a lesser extent and therefore their observation in the analysis result form can lead to incorrect interpretation.
The cardiovascular system
Changes in the functioning of the cardiovascular system occur among the very first. Their profound restructuring begins already in the early stages of gestation. The main events are physiological vasodilation and fluid retention in the body. Peripheral vasodilation leads to a decrease in vascular resistance and an increase in cardiac output, an increase in heart rate, and an increase in venous pressure.
Blood pressure decreases in the first and second trimesters, but rises to levels in non-pregnant women in the third trimester.
Water balance
Low blood pressure during pregnancy leads to activation of the renin-angiotensin aldosterone system, resulting in increased release of antidiuretic hormone. There is a tendency to retain water and sodium, and the likelihood of edema formation increases.
Hematological changes
Pregnancy is accompanied by stimulation of hematopoietic processes. There is a general increase in plasma, red blood cell (RBC) counts, and total circulating blood volume. Plasma volume increases during normal pregnancy. An increase of 15% occurs in the first trimester; in the second trimester, this trend continues, reaching a maximum at 32 weeks. By this time, the plasma volume has increased exactly by half.
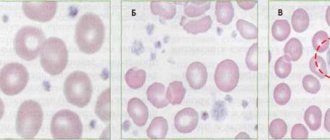
The number of red blood cells increases, but occurs more slowly compared to plasma, making the blood more dilute and leading to the “physiological anemia” of pregnancy. There is a decrease in hemoglobin and hematocrit and mean erythrocyte hemoglobin content (MCH). The maximum decrease in hemoglobin levels is observed at 32–34 weeks of pregnancy.
During pregnancy, the volume of red blood cells changes. During the first 8 weeks of pregnancy, MCV decreases, by week 16 it returns to normal values, as in non-pregnant women, and then MCV increases.
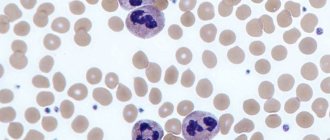
White blood cell (WBC) levels increase by an average of 20%. The following changes are noted in the leukocyte formula: the absolute number of neutrophils (band and segmented) increases, the number of lymphocytes decreases.
The platelet count (PLT) changes ambiguously. Pregnancy is associated with increased platelet turnover.
An increase in blood volume is accompanied by an increase in ESR. In the first trimester, the ESR value is 15 mm/hour, in the second - 25 mm/hour, in the third - 40 mm/hour.
Hemostasis indicators
Throughout the entire period of pregnancy, the body prepares for the upcoming blood loss, so certain changes occur in the hemostatic system.
Changes in the blood coagulation system during pregnancy lead to a physiological state of hypercoagulability or increased susceptibility to thrombosis. In the third trimester, coagulation activity is twice as high as normal. The procoagulant activity of the hemostasis system increases, on the other hand, the activity of the fibrinolysis system decreases.
The concentrations of factors VII, VIII, IX, X, XII and von Willebrand factor increase.
Factor XI values decrease to 60–70% of those in non-pregnant women.
Fibrinogen levels increase significantly - up to 50%.
Levels of protein S and antithrombin III gradually decrease during pregnancy, while protein C activity remains unchanged.
Plasma fibrinolytic activity decreases throughout pregnancy but returns to normal within one hour after delivery.
Thrombin is generated as the gestational age increases. The D-dimer value increases throughout pregnancy. Only 3–5 days after delivery, the D-dimer value returns to its original values.
A shortening of APTT is observed in the second and third trimester and is associated with an increase in the activity of procoagulants in the blood. In the third trimester, a shortening of prothrombin time is observed.
Carbohydrate metabolism
Pregnancy is a diabetogenic condition because it is associated with the development of insulin resistance. An increase in the level of estrogen and progesterone in the initial stages leads to hypertrophy of pancreatic cells that secrete insulin. As a result, insulin secretion and tissue sensitivity to it increase in the early stages.
In the second trimester, insulin resistance begins to appear, reaching a peak in the third trimester. This results from the secretion of contrainsular hormones: human placental lactogen, growth hormone, progesterone, cortisol and prolactin. These hormones cause a decrease in the sensitivity of peripheral tissues to insulin, especially in adipose tissue and skeletal muscle, by interfering with insulin receptor signaling.
Insulin levels during pregnancy increase during fasting, after eating.
Fasting glucose levels often decrease due to:
- increasing storage of tissue glycogen reserves;
- increased use of peripheral glucose;
- decreased liver glucose production;
- glucose absorption by the fetus.
Insulin resistance and relative hypoglycemia lead to an increase in the process of lipolysis - the formation of fats, which primarily allows the use of fat as fuel, preserving glucose and amino acids for the fetus. The placenta allows the transfer of glucose, amino acids and ketones to the fetus, but is impermeable to large lipids. If a woman's endocrine pancreatic function is impaired and she cannot overcome the insulin resistance associated with pregnancy, she develops gestational diabetes.
During pregnancy, physiological transient glycosuria is often observed, which is associated with an increase in the glomerular filtration rate and an increase in the permeability of the renal tubular epithelium.
Protein metabolism
Throughout pregnancy, a woman needs more protein, since anabolic processes prevail over catabolic processes.
There is a physiological decrease in blood albumin; dilution of the blood also contributes to a decrease in the proportion of albumin.
The proteinogram in the first and second trimester has the following features: a decrease in albumin levels, a slight increase in the a-2 and b-1 globulin fraction. In the third trimester, there is a sharp increase in the a-1 globulin fraction.
And due to increased protein metabolism, a positive nitrogen balance is observed. Due to an increase in GFR by 75%, creatinine and urea levels decrease. A decrease in creatinine occurs mainly in the first and second trimesters, when intensive growth of the uterus is observed. The level of urea falls due to increased protein utilization, especially pronounced in the third trimester.
Lipid metabolism
The general effects of altered lipid metabolism during pregnancy are the accumulation of fat reserves in the mother's body in the first half and increased mobilization of fats in the second half of pregnancy.
Hypercholesterolemia is caused by increased production of sex steroid hormones, changes in metabolism in the liver and adipose tissue. Elevated triglyceride values provide the mother with energy needs. An increase in LDL cholesterol is associated with an increase in progesterone, in addition, LDL cholesterol is a source of placental progesterone. Increased concentrations of estrogen during pregnancy cause an increase in total cholesterol, LDL cholesterol and triglycerides.
Regional fat deposition in the mammary glands and subcutaneous fat is associated with increased conversion of carbohydrates into fats under the influence of insulin.
Mineral metabolism
Pregnancy causes an increase in the need for iron by 2-3 times for the synthesis of hemoglobin, for the production of certain enzymes. The need for folic acid increases 10–20 times, the need for vitamin B12 doubles.
The third trimester marks the peak demand for calcium.
During pregnancy, the concentration of total calcium in the blood serum decreases due to a decrease in the proportion of blood albumin, but the level of ionized calcium remains unchanged.
Reasons for increase or decrease
In some cases, the number of these blood cells decreases or increases. There could be many reasons for this. The main factors for low platelet levels are:
- the occurrence of an allergic reaction;
- intrauterine fetal death;
- viral diseases;
- Poor nutrition leading to insufficient intake of vitamin B12 and folic acid;
- drug poisoning;
- long-term use of antibiotics;
- obstetric hemorrhage, for example caused by placental abruption;
- autoimmune thrombocytopenia;
- neuropathic diseases;
- increased death of red blood cells due to hormonal imbalances.
In some cases, low levels of these cells can be observed under the influence of physiological factors. In this case, no special treatment is required. However, it is important to keep track of all times. For this purpose, blood tests are carried out regularly.
There is also a secondary form of the pathological condition, in which there is a decrease in the number of platelets. In this case, the cause may be radiation or toxic poisoning.
Factors that contribute to the appearance of an increased platelet count include:
- cardiovascular abnormalities;
- predisposition to thrombosis;
- phlebeurysm;
- allergic reactions;
- lack of iron in the body;
- formation of malignant neoplasms;
- taking certain medications;
- infectious diseases;
- pathologies of the autoimmune system;
- increased toxicity in early pregnancy.
Sometimes a high cell count occurs when there is no fluid in the body.
A complex test, including a group of laboratory tests to determine the general health, functioning of the main systems and organs of a pregnant woman in the third trimester of pregnancy.
Synonyms Russian
Pregnancy, III trimester.
English synonyms
Pregnancy third (III) trimester.
What biomaterial can be used for research?
Venous blood, an average portion of morning urine.
How to properly prepare for research?
- Eliminate alcohol from your diet for 24 hours before the test.
- Eliminate fatty foods from your diet for 24 hours before the test.
- Do not eat for 12 hours before the test; you can drink clean still water.
- Avoid (in consultation with your doctor) taking diuretics for 48 hours before collecting urine.
- Completely avoid (in consultation with your doctor) taking medications for 24 hours before the test.
- It is recommended to collect urine before menstruation or 2-3 days after it ends.
- Avoid physical and emotional stress for 30 minutes before the test.
- Testing for HIV infection can be carried out anonymously and confidentially. During a confidential examination, it is mandatory to present a passport.
- Do not smoke for 30 minutes before the test.
General information about the study
The third (III) trimester of pregnancy includes the period between 27 (28) and 38 (40) weeks of pregnancy. During this period, active growth of the fetus occurs, improvement of organ systems, in particular the respiratory system, development of sensory organs, and maturation of the nervous system. Clinical laboratory diagnostics are aimed at assessing the functioning of major organs and systems, in particular the kidneys, liver, blood coagulation system, endocrine system of a pregnant woman, as well as controlling infection during pregnancy.
A clinical blood test allows you to evaluate the qualitative and quantitative composition of blood according to the main indicators: red blood cells, leukocytes and their varieties in absolute and percentage terms, platelets. Detection of deviations in these indicators may indicate the presence of pathological processes and diseases in a pregnant woman. A reduced number of red blood cells and the hemoglobin content in red blood cells may indicate the presence of anemia in pregnant women. This condition can lead to placental insufficiency - the main cause of miscarriage, low birth weight babies and fetal death. Changes in the leukocyte formula may indicate a wide range of changes in the body of a pregnant woman. These may be laboratory signs of inflammatory and infectious diseases, pathologies that a woman has, but have not previously been diagnosed. The platelet count during pregnancy may be lower than normal, which must be taken into account. Significant changes in these indicators and developing thrombocytopenia require special monitoring, as they may be indirect signs of pathologies of the blood coagulation system, as well as such a severe complication of pregnancy as DIC syndrome (disseminated intravascular coagulation syndrome). Changes in ESR can be observed in the presence of acute and chronic inflammatory diseases and infectious processes. A slight increase in ESR can be observed during pregnancy. This test has high sensitivity but low specificity and is prescribed in combination with other indicators.
A general urinalysis with microscopy of urinary sediment is a set of diagnostic tests that allow one to assess the general properties of urine, its physicochemical properties, the content of metabolic products, and identify the qualitative and quantitative content of a number of organic compounds. These tests reflect the functional state of the kidneys and urinary tract, allow one to judge general metabolic processes, and suggest the presence of possible disorders, infectious and inflammatory processes. The detection of glucose and ketone bodies in the urine may indicate the development of impaired carbohydrate tolerance, diabetes mellitus, and pregnancy diabetes. Detection of protein in the urine may be a sign of developing nephropathy in pregnancy; proteinuria more than 0.3 g in daily urine may indicate the development of a severe complication of pregnancy - preeclampsia. The severity of this condition varies greatly. Thus, with the development of mild preeclampsia after 36 weeks, the prognosis is usually favorable. On the contrary, the threat to the health of the mother or fetus increases significantly if preeclampsia develops early (before 33 weeks) and is aggravated by the presence of concomitant diseases.
In the third trimester of pregnancy, it is also necessary to monitor the functional state of the blood coagulation and fibrinolysis system. The prothrombin time test is used to evaluate the extrinsic clotting pathway. The following indicators are obtained as results: Quick prothrombin time and international normalized ratio. Activated partial thromboplastin time (aPTT) characterizes the intrinsic pathway of blood coagulation. Fibrinogen is factor I (the first) factor of the blood plasma coagulation system. These indicators make it possible to assess the functional state of the liver, the main pathways of the blood coagulation system, and assess the functional state of its components. Their determination is important for predicting thrombosis during pregnancy, diagnosing a complication such as disseminated intravascular coagulation syndrome, and planning the necessary therapy during childbirth - a process accompanied by massive blood loss. It should be noted that there is a physiological increase in the levels of prothrombin and fibrinogen in the third trimester of pregnancy. But a sharp increase in these indicators requires special monitoring and prescription of the necessary therapy. The level of D-dimer also increases during the physiological course of pregnancy, especially at 35-40 weeks, but a sharp increase in the concentration of D-dimer may indicate a large number of blood clots, which is most often caused by venous thromboembolism or disseminated intravascular coagulation syndrome.
Determination of such biochemical parameters as alanine aminotransferase (ALT), aspartate aminotransferase (AST), total bilirubin and direct bilirubin fraction, total protein in serum allows us to assess the functional state of the liver. ALT levels may be slightly elevated, while AST levels are decreased. A significant increase in the concentration of transaminases may indicate the presence of liver damage, hepatitis, and the development of preeclampsia. A decrease in the level of total protein in the blood serum along with the loss of protein in the urine and with an increase in blood pressure more than 140/90 mm Hg. Art. is also a sign of developing preeclampsia.
To exclude the development of diabetes in pregnant women (gestational diabetes), the development of complications, in particular diabetic nephropathy, it is necessary to determine the level of glucose in the blood plasma.
To assess the functional state of the kidneys, in particular the integrity of glomerular filtration processes, several diagnostic parameters are used. The most important and characteristic is the determination of the levels of urea and creatinine in the blood serum, as well as the assessment of the glomerular filtration rate. It is important that creatinine levels are reduced by almost half in pregnant women due to increased blood volume, increased blood flow in the kidneys and, accordingly, an increased degree of filtration. Also, an increase in renal filtration causes a decrease in the amount of urea in pregnant women.
Typically, pregnancy occurs with normal levels of thyroid-stimulating hormone (TSH) in the blood. This euthyroid state is maintained by all components of the thyroid system and placental hormones, in particular human chorionic gonadotropin and human chorionic thyrotropin. The thyroid hormone systems of the mother and fetus are independent of each other and weakly penetrate the mature placenta. The TSH level in the blood of pregnant women may increase with the development of preeclampsia.
In the third trimester of pregnancy, it is also recommended to retest for hepatitis B - HBsAg, hepatitis C - anti-HCV, antibodies, HIV infection - HIV 1.2 Ag/AbCombo (determination of antibodies to HIV types 1 and 2 and p24 antigen), syphilis - antibodies to Treponema pallidum. The incubation period for some infections varies greatly and a negative result from tests taken early in pregnancy may change in the last weeks of pregnancy or remain negative. This is necessary to prevent infection of the fetus during childbirth, prescribe the necessary treatment or perform a planned cesarean section.
What is the research used for?
- For preventive examination of pregnant women in the third trimester of pregnancy.
- If there is a suspicion of deviations in the normal functioning of the systems and organs of pregnant women.
- To diagnose complications of the third trimester of pregnancy.
When is the study scheduled?
- Pregnant women in the third trimester at 27-38 (40) weeks of pregnancy.
What do the results mean?
Reference values
For each indicator included in the complex:
- [02-005] Clinical blood test (with leukocyte formula)
- [02-006] Urinalysis with microscopy
- [02-007] Erythrocyte sedimentation rate (ESR)
- [03-001] D-dimer
- [03-003] Activated partial thromboplastin time (APTT)
- [03-007] Coagulogram No. 1 (prothrombin (according to Quick), INR)
- [03-011] Fibrinogen
- [06-003] Alanine aminotransferase (ALT)
- [06-010] Aspartate aminotransferase (AST)
- [06-015] Plasma glucose
- [06-021] Serum creatinine (with GFR determination)
- [06-034] Serum urea
- [06-035] Total protein in serum
- [06-036] Total bilirubin
- [06-037] Direct bilirubin
- [07-009] anti-HCV, antibodies
- [07-025] HBsAg
- [07-032] HIV 1.2 Ag/Ab Combo (determination of antibodies to HIV types 1 and 2 and p24 antigen)
- [07-049] Treponema pallidum, antibodies
- [08-118] Thyroid-stimulating hormone (TSH)
What can influence the result?
- The use of medications, in particular hormonal ones.
Symptoms
Although the diagnosis is made solely on the basis of test results, in most cases an abnormality can be suspected by the appearance of certain symptoms.
If your platelets have dropped, you may experience symptoms such as:
- The formation of bruises on the body, which can be provoked even by a light blow to the skin;
- small rashes;
- Bleeding gums during oral hygiene procedures;
- Nose bleed;
- Poor blood clotting due to skin changes;
- Dark-colored stool;
- Bloody discharge from the genital tract.
The symptoms of an increase in the number of cells are in many ways similar to the symptoms of thrombocytopenia. This is due to the fact that, despite the various factors that provoke the development of these pathological conditions, the manifestation is common: blood cells in the vessels begin to be distributed unevenly.
To avoid negative consequences that can be dangerous for both the pregnant woman and the fetus, constant monitoring of platelet levels in the body is necessary.
What changes occur in the female body?
Physiological changes occurring in a woman’s body are necessary to ensure an adequate course of the gestational period, development and growth of the fetus, preparation for the birth of a child and breastfeeding. On the one hand, these processes are associated with increased stress on organs and systems, on the other hand, various pathological conditions can develop during pregnancy, even if they are latent. The mother delivers all the necessary nutrients to the fetus and removes metabolic products, which causes the load. Its degree may vary during pregnancy and increases with each month. A significant restructuring of the vital functions of the female body is accompanied by changes in the blood systems, hemostasis, hormonal status, immunity, and changes also occur at the biochemical level.
Laboratory indicators of a pregnant and non-pregnant woman are very different from each other, so it is very important to determine their “norm”. Knowledge of these indicators is necessary to optimize monitoring, effective prevention and timely treatment of various complications.
- The cardiovascular system . Changes in its work occur among the first: deep restructuring begins in the early stages. During pregnancy, physiological vasodilation and fluid retention in the body occur. As a result, the heart rate increases, cardiac output increases, and venous pressure increases. Blood pressure, on the contrary, decreases in the I-II trimester.
- Water balance . Reduced blood pressure activates the renin-angiotensin-aldosterone system, which is manifested by increased secretion of antidiuretic hormone. The body begins to retain water and sodium, and the risk of edema increases.
- Hematological changes . During pregnancy, the processes of hematopoiesis change - the amount of plasma increases (by 15% in the first trimester), the number of red blood cells and the total volume of circulating blood increases. As a result, hemoglobin and hematocrit levels decrease. The concentration of leukocytes increases by an average of 20%, which is accompanied by changes in the leukocyte formula. An increase in blood volume leads to an increase in ESR - erythrocyte sedimentation rate.
- Hemostasis . During the entire period of pregnancy, a woman’s body prepares for upcoming blood loss, which is accompanied by changes in the hemostatic system. Changes in the blood coagulation system cause a physiological state of hypercoagulation - an increased tendency to form blood clots: by the third trimester, coagulation activity is twice the norm. The concentration of coagulation factors and fibrinogen levels increases.
- Carbohydrate metabolism . Pregnancy is a diabetogenic condition, as it is associated with the development of insulin resistance. An increase in the concentration of estrogen and progesterone in the early stages leads to hypertrophy of pancreatic cells that produce insulin. Insulin resistance begins to appear in the second trimester, reaching a peak in the third. Fasting glucose levels often decrease.
- Protein metabolism . Throughout pregnancy, a woman needs more protein, which is due to the predominance of catabolism over anabolism. A physiological decrease in the level of albumin in the blood and an increase in a-2 and b-1 globulin fractions develop. As a result, a positive nitrogen balance is observed, the concentration of urea and creatinine decreases.
- Lipid metabolism . The general effects of changes in lipid metabolism during pregnancy are manifested by the accumulation of fat reserves. Increased production of sex steroid hormones leads to hypercholesterolemia. Regional fat deposition in the mammary glands and subcutaneous fat is associated with increased conversion of carbohydrates to fats under the influence of insulin.
- Mineral metabolism . During pregnancy, a woman’s body’s need for iron increases 2-3 times. It is necessary both for the synthesis of hemoglobin and for the production of certain enzymes. In addition, the need for folic acid and vitamin B12 increases. In the third trimester, there is a peak demand for calcium.
Taking care of your child’s health should begin from the moment you plan your pregnancy. Timely completion of laboratory examinations by the expectant mother when planning pregnancy and throughout this period is an important factor in the birth of a healthy baby. However, each trimester is characterized by different changes in the body, so it is very important to detect the slightest deviations from the norm and correct them in a timely manner.
What tests are needed?
To control the composition of the blood, certain laboratory tests are carried out. Only after a thorough examination of the biological material is a diagnosis made: low or high platelet count in pregnant women.
Diagnostics consists of performing tests such as:
- General examination of the patient by a gynecologist, therapist or hematologist;
- Blood test to determine platelet count, ferritin and serum iron levels;
- Ultrasound examination of internal organs.
If necessary, an additional bone marrow biopsy may be recommended.
Sometimes there are situations where, despite positive blood test results, you may find that you have a low blood clot level or a tendency to form one. In this case, the patient is referred for a coagulogram.
This testing method determines the level of cell aggregation, that is, their ability to bind to collagen. In the normal range, this ratio should be between 30 and 60 percent.
To obtain the most accurate results, you must be well prepared when submitting material for analysis. It is important that blood sampling is carried out on an empty stomach. For several days, it is recommended to avoid taking medications that can negatively affect the number of platelets in the blood.
In addition, it is better to refuse the analysis if three days before the study there was an injury accompanied by bleeding or a burn.
Treatment of thrombocytopenia and thrombocytosis
Treatment tactics will be chosen based on the diagnosis. In both cases, complex treatment will be required to correct the situation.
Drug therapy
The third trimester of pregnancy is considered the most dangerous period for low platelet levels. Treatment in this case should be aimed at eliminating the cause that caused the decrease in the number of cells.
The following drugs are used to increase the platelet count:
- Glucocorticosteroids, the course of which can be either systemic or short-term;
- intravenous immunoglobulins;
- lamellar mass, which is prescribed for complicated pathological conditions.
If conservative treatment methods do not bring positive results, a method is used in which the spleen is removed using laparoscopy.
If you have been diagnosed with elevated platelet levels, you should take medications such as:
- coagulants;
- antiplatelet drugs.
If thrombocytosis is incompatible with labor, your doctor will advise you to terminate the pregnancy.
If there is a slight deviation in height from the norm, no special treatment is required. In this way, the body can respond to uteroplacental blood flow.
Diet
No less important for the normalization of platelets is the nutrition of the expectant mother. To increase your platelet count, you should follow certain recommendations:
- Include plenty of beets and beet juice in your diet.
- Consume plenty of sesame oil. It can be added to vegetable salads. This drug regulates platelet levels and improves blood clotting.
- Monitor your iron levels. The daily norm should be about 30 milligrams. Experts recommend eating buckwheat, beef and liver.
- Eat foods high in vitamin B12 and folic acid every day. This may include meat, fish, dairy products, nuts and eggs.
- Take ascorbic acid.
In addition, to normalize the reduced number of cells, it is good to drink rosehip tea, as well as nettle decoction.
If this indicator increases, it is necessary to include in the diet such foods as:
- juice (can be made from cranberries, tomatoes, citrus fruits, apples or cranberries);
- olive oil or flaxseed oil;
- mackerel and other fatty fish;
- Garlic;
- legumes and grains;
- milk and dairy products;
- Herbs.
- bananas;
- pomegranate juice;
- rosehip;
- lentils;
- Italian nuts;
- mango.
Fluid intake also plays an important role. The daily minimum allowable intake for pregnant women is at least one and a half liters of clean water.
Possible complications
If you do not take quick action to normalize your platelet levels, this can lead to serious consequences.
Deviation from the norm in a large direction leads to:
- intrauterine growth retardation;
- inevitable miscarriage;
- severe toxemia;
- phlebeurysm;
- thrombosis of the upper and lower extremities;
- heart attack or embolism.
When platelet levels are low, complications arise such as:
- uncontrolled heavy bleeding;
- premature birth;
- Thrombocytopenia in a child.
With early diagnosis and proper treatment, such problems can be avoided.
Prevention
To prevent the development of thrombocytopenia in a pregnant woman, it is important to follow certain rules:
- Eliminate all factors that can negatively affect the state of the immune system;
- Before planning a pregnancy, get all the necessary vaccinations against ARVI, rubella, chickenpox and other viral infections;
- Stop taking certain medications in early pregnancy;
- Change your diet.
To prevent thrombocytosis, the following preventive measures are taken:
- maintaining an active lifestyle;
- Excluding foods that increase blood viscosity from the menu;
- Drink more fluids and food to thin your blood.
Be sure to monitor your platelet count throughout your pregnancy. This is why it is so important not to neglect regular examinations by specialists and examinations.
Second trimester examinations
The second (II) trimester of pregnancy includes the period between 13 and 26 weeks. It is during this time period, closer to the 16th week, that all organs and systems of the fetus are finally formed, but continue to develop, the placenta is formed, and after the 23rd week the fetus is already considered fully viable and formed. Clinical laboratory diagnostics of a number of biochemical indicators during this period reflects not only the state of health of a pregnant woman and the functioning of the main organs and systems, but also makes it possible to detect diseases and possible complications.
Thus, Program 185 “Examination of a pregnant woman at 22-24 weeks of pregnancy” includes the following studies:
- General detailed blood test. Aimed at a basic assessment of the general state of health: the hematopoietic system, the presence of inflammatory, infectious (including viral), oncological diseases, as well as allergic processes in the body.
- General urine analysis. Allows you to assess the condition of the urinary tract and some extrarenal diseases, to identify the presence of gestosis.
- Glucose tolerance test, which makes it possible to evaluate disorders of carbohydrate metabolism (including hidden forms).
- HIV 1/1o/2 to detect HIV infection.
It is advisable to perform a general detailed blood test with leukocyte count and ESR (erythrocyte sedimentation rate) and a general urine test once a month.
A clinical blood test makes it possible to study the qualitative and quantitative composition of blood according to key indicators: red blood cells and their specific indicators, leukocytes and their varieties in absolute and percentage terms, platelets. Detection of abnormalities in these markers may indicate the presence of pathological processes in the body of a pregnant woman. A decrease in the level of red blood cells and hemoglobin in red blood cells is a sign of anemia in pregnant women. This can lead to placental insufficiency - the main cause of miscarriage, low birth weight babies and fetal death.
Changes in the leukocyte formula can indicate a wide range of changes in the body of pregnant women in the 2nd trimester. They can act as laboratory signs of previously undiagnosed inflammatory and infectious processes, which require more extensive additional examination - both instrumental and laboratory. The platelet count may decrease slightly during physiological pregnancy, but significant changes in this indicator, including developing thrombocytopenia, require special monitoring, since they may be indirect signs of a disorder of the blood coagulation system, as well as DIC syndrome (disseminated intravascular coagulation syndrome), which are severe complications of pregnancy.
Changes in erythrocyte sedimentation rate (ESR) can be observed in acute and chronic inflammatory pathologies, infectious diseases, as well as oncological and autoimmune processes. At the same time, in pregnant women, the erythrocyte sedimentation rate normally increases slightly.
A general urine test allows you to evaluate the general properties of urine, its physicochemical properties, the presence of metabolic products, and detect the quantitative and qualitative content of certain organic compounds. This study reflects the functional state of the kidneys and urinary tract, allows one to assess general metabolic processes, and suggest the presence of infectious and inflammatory processes. The detection of glucose and ketone bodies in the urine may indicate the development of carbohydrate intolerance, diabetes mellitus, or “pregnant diabetes.” If protein is detected in the urine, this may be evidence of developing kidney pathology in pregnant women, as well as a sign of the development of a severe complication during pregnancy - preeclampsia for more than 20 weeks.
A glucose tolerance test can detect gestational diabetes (“diabetes during pregnancy”). If this abnormality is detected, the woman needs to monitor her sugar levels throughout pregnancy and after childbirth. It is very important to detect gestational diabetes early to prevent a number of undesirable consequences, including the birth of a large fetus and the threat of prenatal complications.
HIV research . To reduce the risk of infection of the fetus, it is very important to promptly detect the human immunodeficiency virus in a pregnant woman. Detection of HIV infection is an indication for preventing the transmission of HIV from mother to child, and not for terminating pregnancy. Without preventive measures, the risk of transmitting HIV infection from mother to fetus is 20-40%, but the use of special preventive measures reduces the likelihood of transmission of infection to 1-2%. Most cases of infection occur during the passage of the fetus through the natural birth canal. In addition, there is a high probability of infection during breastfeeding.
We have described the capabilities of Program 185 alone, “Examination of a pregnant woman at 22-24 weeks of pregnancy,” but there are a number of other important studies.
Prenatal screening of the second trimester is a “triple test”, including determination of the total unit of beta-hCG, AFP and unconjugated (free) estriol. It is carried out for the purpose of biochemical screening of a pregnant woman to assess the risks of certain chromosomal abnormalities of the fetus:
- Down syndrome. The disorder is accompanied by characteristic features of appearance, mental retardation, defects of internal organs, and short stature.
- Edwards syndrome. Most children with this syndrome die before the age of 3 months, only 5-10% survive to one year. The survivors have severe mental retardation.
- Patau syndrome. Accompanied by severe congenital malformations.
Also, prenatal screening in the second trimester makes it possible to assess the risk of fetal neural tube defects.
The study is performed between 14 and 21 weeks, optimally from 16 to 18 weeks of pregnancy. Down, Edwards and Patau syndromes are the most common chromosomal disorders. The ability to detect these disorders in the early stages allows for a timely assessment of the genetic health of the fetus.
An alternative to biochemical prenatal screening is the NIPT test. It is more accurate than biochemical, and its results are not affected by the course of pregnancy, medications taken, or somatic diseases of the woman. The difference from biochemical screening is that NIPT is a direct method that allows you to examine fetal DNA, while biochemistry is an indirect method. Biochemical screening has an accuracy of 70-80%, while NIPT has an accuracy of more than 99.9%.
Another important laboratory marker in the 2nd trimester is thyroid-stimulating hormone (TSH). This hormone is produced by the pituitary gland and is responsible for regulating the synthesis of the thyroid hormones thyroxine and triiodothyronine through a “feedback system” that allows maintaining a stable concentration of these hormones in the blood. Despite the fact that the thyroid hormone systems of the pregnant woman and the fetus do not depend on each other, her health and, accordingly, the course of the entire pregnancy depend on the normal functioning of the woman’s thyroid system. During pregnancy, TSH levels in the blood often remain stable. TSH is important for normal fetal development, in particular for the normal formation of the central nervous system. In iodine deficiency conditions, compensatory hyperplasia of the fetal thyroid gland may develop.
In the second and third trimester of pregnancy, it is important to assess the risk of one of the most serious complications of pregnancy - preeclampsia. Placental growth factor (PLGF), a marker of preeclampsia, has angiogenic properties and is necessary for the normal development of the placental vascular system. Normally, PlGF concentrations gradually increase until 30 weeks of pregnancy. In the case of preeclampsia, a decrease in PLGF is observed. Timely identification of increased risk allows us to predict the optimal tactics for managing pregnancy and childbirth.