A person cannot independently find out whether there is a blood clot. Read the article, it describes diagnostic methods and the first signs of thrombosis.
A thrombus is a collection of white blood cells, red blood cells and platelets that form a clot that blocks the flow of blood. Localized in the veins and arteries of various organs. If a blood clot blocks a vein or artery, it is a major health hazard and can even be fatal. In this article, we will look at how to find out if there is a blood clot in the body, how to diagnose it, and how to help a loved one if the blood clot has broken loose.
How to find out if a person has blood clots in the body in the vessels: symptoms, signs
Thrombus
A thrombus is a blood clot that completely or partially closes the lumen of a vessel, formed due to stagnation of blood in various organs. Thrombosis is a disease in which the presence of blood clots in the human body is confirmed by a doctor.
Important: This diagnosis should only be made by a doctor. If you notice the first signs or symptoms, you should immediately consult a doctor.
So how can you tell if a person has blood clots in their blood vessels? Some symptoms indicate this, but depending on the location of the blood clot in a particular organ, they vary significantly. Signs of blood clots in the body and their location:
- In the brain it can cause dizziness, headaches, and fainting.
- In the lower extremities - swelling, bluish skin, bruising.
- In the heart - pain in this organ, arrhythmias, ischemic heart disease, hypotension, shortness of breath, numbness of the hands.
- In other organs there will also be noticeable disruptions in their functioning.
The very presence of blood clots in the body is usually without symptoms, and the person feels unwell only in the organ where the blood clot is located. The worst thing is a complication, namely the detachment of a blood clot.
Remember: In such cases, there is a high probability of disability and death. The process occurs rapidly, in most cases minutes count - heart attack, stroke, pulmonary embolism, failure of other organs.
In such cases, a person needs urgent medical attention. The administration of necessary medications should be carried out as soon as possible and only by qualified personnel to avoid complications.
Classification of thrombosis
Depending on the location of the pathological process:
Arterial:
- arteries of the brain;
- hearts;
- intestines (mesenteric thrombosis);
- liver;
- femoral artery and others.
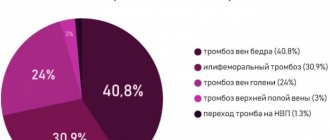
Venous (phlebothrombosis):
- veins of the lower limb;
- hemorrhoidal plexus;
- femoral and iliac veins;
- cavernous sinus (intracranial collector of venous blood);
- retinal veins.
According to the severity of the disease, acute
ー a sharp blockade of blood flow, and
a chronic
ー thrombus grows gradually, the tissues have time to adapt to this and compensate for pathological changes.
How to determine whether there are blood clots in the legs, is a blood clot in the leg dangerous?
thrombus
is a blood clot that completely or partially blocks the flow of blood in the vessels. Thrombophlebitis or thrombosis is the presence of a blood clot in the vessels of the legs. Is a blood clot in the leg dangerous? It all depends on the complexity of the disease and the location of the blood clot. There are diseases associated with the formation of blood clots:
- Thrombophlebitis, thrombosis - causes inflammation and subsequent necrosis of nearby tissues, the temperature of the affected area is usually increased.
- Phlebothrombosis is when one or more blood clots are located in the veins of the lower extremities. With this disease, the temperature of the affected area is normal or the limbs may even be cool.
- Thrombosis can be arterial or venous . The difference lies in the mobility of the formed blood clots. So, in the first case, the probability of mobility of clots is high. In the second, it is practically reduced to zero, due to the lack of pressure and the presence of valves in the veins, which are an additional barrier to the mobility of blood clots.
A blood clot in the leg is dangerous because it poses a health threat. If a doctor diagnoses such a disease, the patient is first prescribed drug treatment, so that the blood clot should resolve on its own. If this does not happen, blood clots are “broken” using modern technologies: laser and other techniques.
How to determine if there are blood clots in the legs:
- A person may suspect this disease if he has swelling and cyanosis, usually of one leg.
- Only a doctor can diagnose the presence or absence of the disease using ultrasound.
- If the diagnosis is confirmed, treatment is prescribed.
Remember: All of the above diseases are dangerous, because if left untreated, they can lead to gangrene, and ultimately the loss of a limb.
In addition, with the blood flow, clots can move to other organs and cause their failure and lead to death.
Coping with risk
Risk groups include people with cardiovascular diseases, the older generation, obese patients and men. The doctor also added that the risk of thrombosis is high in hypertensive patients and those with type 2 diabetes. Thrombosis can also affect heavy smokers.
Professor Roman Komarov noted that women taking contraceptives may be at risk.
“Risk factors include taking contraceptives, being sedentary and having high cholesterol,” the specialist added.
To reduce the risk of thrombosis, Drobyazgo advised timely examination, visiting a therapist and a cardiologist.
All men after 35–40 years old should undergo a vascular examination. It is advisable to do an ultrasound examination of the carotid arteries, since atherosclerosis is a generalized condition. If there are plaques in the carotid artery and arteries of the lower extremities, then we can assume that they are in the heart and in other locations
Sergey Drobyazgo.
According to the phlebologist, even if no plaques are found after the examination, then after six months or a year you need to visit a cardiologist and record your condition. At the same time, it is worth examining your cholesterol level and prescribing diet and medications in accordance with it.
If the patient has thrombosis, there is a small chance of recovery. Drobiazgo said that the patient was immediately hospitalized, coronary angiography, balloon angioplasty was performed and blood supply was restored. Drobyazko warned that if these procedures are not carried out in the first hours, then part of the person’s heart muscle will die. During a stroke, doctors also have a narrow window of opportunity when blood flow can still be restored and many body functions will be preserved.
Blood clot in the heart: what is it, symptoms, what to do?
Blood clot in the heart
If a blood clot is located in the vessels of the heart, then if it breaks off, it can lead to a heart attack, or its free movement to other organs and blockage of blood vessels. When a blood clot appears in the left atrium, the patient may experience the following symptoms:
- Fainting
- Numb hands
- Dyspnea
- Low blood pressure
- Heartache
- Pale skin
If a blood clot is found in the heart on the right:
- Cyanosis or blueness of the skin
- Dyspnea
- Weakness
- Hand tremors
- Nausea
The thrombus can move between the ventricles or be attached to a certain place by a kind of stalk. What to do at the first symptoms of a blood clot in the heart?
- Providing first aid consists of calling an ambulance.
- Providing assistance on your own is prohibited!
- The risk of an acute condition resulting in the death of the patient within a few minutes is very high.
- Therefore, the speed of providing qualified medical care is important.
Upon arrival, doctors immediately administer anticoagulants, for example:
- Heparin
- Enoxaparin
- Nadroparin
- Dalteparin
The patient should also receive treatment with fibrinolytics:
- Thromboflux
- Streptokinase and others
Important to know : If a person notices the first symptoms of such an ailment, it is necessary to urgently call doctors, otherwise the consequences may be irreversible.
Diagnosis and treatment of thrombosis in Medical
Specialists from the Paracelsus Medical Center will help in diagnosing and eliminating this pathology, provide support during the rehabilitation period, and give recommendations for further prevention.
Our center uses expert-class equipment from leading global manufacturers for diagnosis and treatment. The consultation is conducted by practicing phlebologist surgeons.
On the basis of "Operating Room No. 1" phlebological operations are performed for venous disease. The key advantage of the Paracelsus Medical Center network is highly qualified professional surgeons with extensive practical experience.
Drug treatment
The basis of drug therapy is anticoagulants (thin the blood, prevent the growth of a blood clot), fibrinolytics and thrombolytics (dissolve existing clots), antiatherosclerotic drugs (lower cholesterol levels). If necessary, analgesics, anti-inflammatory drugs, cardiotonic drugs, vitamins, minerals, etc. may be needed as symptomatic therapy.
Surgery
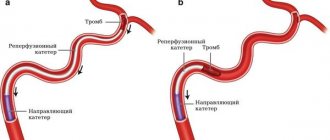
There are such methods of surgical treatment of the disease:
- thrombectomy ー removal of a blood clot;
- stenting (expansion using a frame) and shunting (creating a bypass path for blood flow) for atherosclerotic artery disease;
- arteriovenous shunting.
If the thrombus cannot be removed, a vena cava filter can be installed - the device is placed in the vein above the level of blockage to prevent it from moving and closing the lumen of the vessels of vital organs.
How to check if there are blood clots in the heart?
Ultrasound of the heart
Stagnation of blood in the body leads to such a serious disease as thrombosis. It is difficult to identify immediately or independently, due to the lack of obvious symptoms. But how can you check if there are blood clots in the heart?
The patient should consult a doctor if he is concerned about:
- Chest pain
- Dyspnea
- Tachycardia
With a moving thrombus, the following are possible:
- Frequent fainting
- Pale skin
- Suffocation
- You may also feel dizzy often
- Break out in a cold sweat
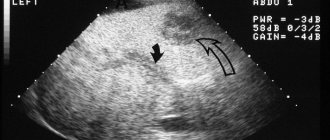
To check whether there are blood clots in the heart, the cardiologist refers to the following types of diagnostic procedures:
- Ultrasound of the heart.
- Ultrasound of the abdominal cavity.
- Echocardiography.
- X-ray of the heart.
- Scintigraphy - shows what is happening inside the blood vessels and their position in the body.
- Dopplerography - measures heart pressure, speed, direction of blood flow in this organ.
- MRI helps to see the heart from the inside and determine the presence of a particular disease.
You should know: Call an ambulance immediately if a person experiences sharp, severe chest pain and blurred vision. Without timely medical care, a blood clot can break off and lead to a heart attack, stroke, or death.
Danger of blood clots
Phlebologist Sergei Drobyazgo explained to “360” that thrombosis is divided into two types - arterial and venous. The latter are deep vein thrombosis and often cause thromboembolism or blood clot rupture. And arterial thrombosis can cause a person to have a heart attack and stroke, since the functioning of the arteries supplying blood to the heart and brain is disrupted.
“In light of the pandemic, the risk of all thromboses has increased,” the specialist added.
Another process is also associated with thrombosis - atherosclerosis, which refers to the formation of plaques in the lumen of the arteries. At some point, the plaque bursts and leads to blockage of the artery, which causes thrombosis.
Roman Komarov, professor at the Clinic of Aortic and Cardiovascular Surgery at Sechenov First Moscow State Medical University, recalled that the main symptoms of arterial thrombosis are pain in the limbs and heart, and swelling.
Can a blood clot break off: is it dangerous, does a blood clot hurt?
Thrombus in the leg
As mentioned above, a thrombus is a clot of red blood cells, leukocytes and platelets that block the lumen of the vessel partially or completely. It depends on how it is attached:
- Parietal - attached to one side of the vessel wall.
- Central - located in the center and blood flows around it.
- Lining - encircles the vessel.
Does a blood clot hurt? Such a blood clot can be felt if it is in the superficial veins of the legs, in the form of a compaction. The surrounding tissues have a bluish tint. When you press on the damaged area, a sharp pain syndrome occurs.
Is a blood clot dangerous? Can it come off? It is dangerous when it is torn off, as it can block a vessel leading to a specific organ, causing negative consequences for the entire body as a whole.
This is why a detached blood clot is dangerous - pathologies, the consequences of which can be irreversible:
- Stroke occurs when a blood vessel in the brain is blocked.
- A heart attack is when a blood clot enters the heart.
- Pulmonary thromboembolism - when a blood clot migrates to the lungs.
- Swelling, inflammation of the tissues of the legs and the development of subsequent gangrene, threatening amputation.
- Failure of the liver, kidneys.
We have all been hearing about the danger of such a pathology for a long time. Doctors talk about this from TV screens. Therefore, when the first signs or unpleasant pain symptoms appear, you should immediately contact a doctor for examination and diagnosis.
When to go to the doctor
–
How does thrombosis manifest itself in very early stages?
– Initially, blood clots do not form in large veins – there is powerful blood flow there. They arise in small veins and have an ascending nature - they grow and move to veins of a larger caliber. With thrombosis of small veins, there is no clear clinical picture: some incomprehensible and unpleasant sensations, discomfort. At this stage, people often turn to other specialists - for example, a neurologist. When thrombosis moves to veins of a larger caliber, edema already occurs, and diagnosis - even according to clinical data - does not present any particular difficulties. There is no need to bring it to a state of edema. It is very important to diagnose thrombosis in the early stages, before it spreads to large veins. Covid partly contributed to the fact that people went to get checked because of the fear of thrombosis, which is now on everyone’s lips.
–
Who should get checked first after Covid?
- Absolutely everyone should. As I already said, regardless of age and severity of the disease. But if we talk about risk factors and groups in general, then these are:
- elderly patients;
- cancer patients;
- patients with chronic venous insufficiency (who once had thrombosis);
- women who are prescribed hormone therapy;
- overweight people;
- leading a sedentary lifestyle (hypodynamia);
- bedridden and trauma patients;
- An additional risk factor is any operation, which can be complicated by thrombosis.
It is worth mentioning separately about varicose veins. For various reasons, this is a fairly common disease today. Varicose veins are an expansion of superficial veins and a prerequisite for the occurrence of thrombosis. The veins are dilated, and, accordingly, the speed of blood movement is less. Eddy currents may occur, which means the risk of blood clots is higher. One of the serious complications of varicose veins is varicothrombophlebitis.
–
If a person suffers from varicose veins, does he need surgical treatment?
– One group of patients is those for whom elective surgery is indicated. I explain exactly the extent of surgical care required, prescribe supportive therapy and give an opinion. Next, the patient goes to a therapist or surgeon at his place of residence and receives a referral for hospitalization. Or - if the operation is simple - you can contact private clinics that deal with this.
Another group of patients are those for whom drug treatment is indicated. This is also quite enough.
A blood clot has broken off - how to find out: can you feel and see a blood clot, is it possible to save a person?
Thrombus
Only a doctor can see the presence of a blood clot using ultrasound diagnostics. It is almost impossible to feel it, but you can only feel the consequences of its presence in the body. Also, when you press on the skin in the area where the blood clot is located, you will feel pain.
If a blood clot breaks off, how can you tell, can you feel it or see it? If an attached blood clot has come off, you can tell by the person’s condition. Depending on the location of the vessel, painful symptoms may be as follows:
- In the brain , this will lead to a stroke. As a result, asymmetry of facial features, difficulty swallowing, and unclear speech.
- heart attack is possible in - pressing, sharp pain in the chest, or complete blockage of the heart vessels, which leads to death.
- In the intestines - a feeling of sharp pain in the abdomen and peritonitis.
- If a blood clot has blocked a vessel in the leg , swelling, blueness, redness, and severe pain are observed. In the absence of proper treatment - gangrene and amputation.
- Blockage in the lungs , also known as pulmonary embolism, is an acute condition that requires immediate hospitalization. It is characterized by a lack of oxygen, due to which the patient’s skin acquires a blue tint, shortness of breath is observed, and untimely assistance can lead to respiratory arrest and death.
Is it possible to save a person and how to provide first aid?
- An ambulance must be called immediately.
- In this case, painkillers and antispasmodics are important, but they should be taken only as directed by the emergency doctor.
- You also need to help the person find a comfortable position.
Often the correct actions of people around them help a person with an acute condition save a life.
Symptoms of thrombosis
The clinical manifestations of this pathology vary depending on the location.
Symptoms of venous thrombosis
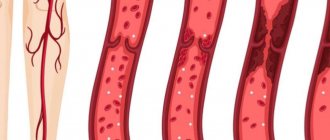
When a vein is blocked, the outflow of blood is hampered, so the tissues beyond the blockage swell and turn blue. The waste products of cells accumulate, therefore tissue intoxication develops, this is accompanied by pain, impaired sensitivity (the sensation of “crawling goosebumps”). If you do not intervene in time, the tissues begin to die.
Symptoms of venous thrombosis of the lower extremities:
- swelling of the leg, a sharp increase in size, cyanosis;
- cramps of the calf muscles;
- constant pain in the leg, which intensifies when walking;
- increased venous pattern on the thigh.
Cavernous sinus thrombosis:
The dura mater contains channels into which venous blood from the brain drains. Blockage of one of these sinuses, the cavernous sinus, is dangerous because several cranial nerves and the internal carotid artery pass through it. The most common causes of cavernous sinus thrombus formation are inflammatory diseases of the nose, sinuses, facial skin and scalp. Signs:
- headache;
- decreased visual acuity, double vision;
- confusion;
- heat, fever;
- swelling of the eyelids and periocular area;
- pain in the neck when turning or tilting the head;
- impaired facial skin sensitivity.
Among the consequences of such thrombosis: stroke, loss of vision, coma.
Hemorrhoidal thrombosis
Develops against the background of hemorrhoids. Chronic constipation, physical stress, pregnancy and childbirth, and alcohol abuse contribute to it. Signs:
- pain, burning and itching in the anal sphincter area;
- discharge of blood with feces and regardless of the act of defecation;
- prolapse of hemorrhoids.
Retinal vascular thrombosis
The pathology is a typical complication of diabetes mellitus and hypertension, but can also develop for other reasons. Symptoms:
- deterioration of vision, up to complete loss (usually one-sided);
- the appearance of spots, mesh, veils before the eyes.
Symptoms of arterial thrombosis
Blockage of the artery leads to oxygen and energy starvation of tissues, which quickly leads to their death. Arterial forms of the disease are often acute.
Thrombosis of the cerebral arteries
This process leads to necrosis of the area of the brain that the affected artery supplies blood to - ischemic stroke. Signs:
- hemiparesis ー lack of movement in the right or left half of the body (opposite affected area);
- asymmetry of the smile - one corner of the mouth is lowered, does not take part in conversation and smile;
- unclear speech;
- when the patient sticks out his tongue, it deviates to the side.
Thrombosis of the coronary arteries of the heart
Partial blockage of these vessels leads to attacks of angina pain, complete blockage leads to myocardial infarction. Symptoms:
- pressing, burning pain behind the sternum, radiating to the left shoulder blade, arm, shoulder, half of the face and neck;
- dyspnea;
- with angina pectoris, rest and nitroglycerin help, with a heart attack there is no improvement, urgent medical attention is needed.
Pulmonary artery thrombosis
It is a complication of thrombosis of the veins of the lower extremities, endocarditis, myocardial infarction. It develops rapidly and has a high mortality rate. Signs:
- sharp stabbing pain in the chest;
- swelling of the veins of the neck;
- shortness of breath, feeling of lack of air;
- hemoptysis;
- increased heart rate.
Hepatic artery thrombosis
Death (infarction) of liver tissue is a complication of endocarditis, myocardial infarction or liver transplantation and manifests itself as follows:
- severe pain under the right rib;
- nausea, vomiting, bitterness in the mouth;
- yellowness of the skin and whites of the eyes.
Femoral artery thrombosis
This form of pathology is manifested by pain when walking, coldness, and paleness of the limb. The pulse in the popliteal fossa and on the foot is palpable weakly or not detected at all.
Can a blood clot form after a leg injury, surgery, or blood draw?
Blood clot in the leg
Post-traumatic blood clot formation is not uncommon. Its serious consequences frighten and worry many people. When might he appear? Can a blood clot form after a leg injury, surgery, or blood draw?
- Any strong mechanical impact on the human body can cause damage to the vessel wall.
- Platelets rushing to help release thromboplastin and thrombin. These elements increase blood viscosity.
- In the injured area, a future thrombus is formed from fibrin fibers.
- This is a natural reaction of the body aimed at protecting against blood loss.
Surgical operations, blood drawing, and punctures in the body are directly related to the dissection and injury of blood vessels.
- With excessive platelet activity, the formation of an enlarged clot is inevitable.
- It may not have any negative impact in the future, or it may become a big problem.
- It all depends on the individual characteristics, health status, and lifestyle of the person.
Leg bruises are also not harmless.
- With a strong blow, a hematoma is formed - a bruise.
- This is a manifestation of rupture of small capillaries with slight hemorrhage.
- However, larger vessels located nearby may also be damaged.
To avoid severe outcomes and the development of thrombosis, you need to know the possible causes of blood clots and try to minimize them in your life.
Is it possible to detect and feel a blood clot on your own? Does a blood clot hurt in your leg?
Blood clot in the leg
Thrombosis is one of the serious diseases of the circulatory system. The reasons for the development of this pathology are injuries, surgical interventions, hormonal disorders, and increased blood viscosity. Is it possible to detect and feel a blood clot on your own? Does a blood clot in your leg hurt?
It will not be easy to independently detect a blood clot visually or by palpation. However, if you suspect the presence of blood clots, you should pay attention to the combination of symptoms. Signs of a blood clot in a vein are:
- Tissue swelling.
- Red or bluish areas on the skin near the vessel, their soreness.
- Increased body temperature.
- Pain that increases with movement of the affected limb.
- With long-term absence of treatment, the vascular network begins to stand out significantly.
With thrombophlebitis, superficial thrombosis, the pathological process develops closer to the skin. It will not be difficult for a knowledgeable person to feel a blood clot; upon palpation, the patient will feel pain and discomfort. But the pain syndrome may not appear if a small vessel is clogged and other veins and arteries take over its role.
Remember: There is no need to try to find a blood clot yourself, as this can be dangerous. The blood clot may be loosely attached to the wall of the vein or artery and may break off.
The best solution would be to consult a doctor who will conduct an examination, a series of studies and make an accurate conclusion about your health status.
Mechanism of development and causes of thrombosis
There are three pathological parts in the process of intravascular thrombus formation:
- Violation of the integrity of the vascular wall. When the internal lining of blood vessels is damaged, enzyme systems are activated, which trigger the process of blood clotting.
- Slowing blood flow. This occurs when the outflow is disrupted (compression of veins, varicose veins), prolonged absence of limb movement, or heart failure.
- Blood thickening. Caused by dehydration, autoimmune diseases, chemotherapy, and oral contraceptives.
A blood clot often forms against the background of such diseases:
- atherosclerosis;
- heart failure;
- aneurysms of blood vessels and heart;
- diabetes;
- obesity;
- bone fractures;
- hormonal disorders;
- oncological diseases.
Do people die from a blood clot: mortality statistics
Thrombus
The formation of a blood clot can occur in different parts of the body and it is very difficult to predict where exactly the blood clot is located. At a critical moment, it breaks away and begins to move, which is instantly fatal. People die from blood clots if treatment is not started in a timely manner and the person does not seek the help of doctors for a long time.
- Mortality statistics are such that more people die from thrombosis than from breast or prostate cancer.
- More than 10 million cases of thromboembolism occur worldwide each year.
Smoking, alcohol, and stress can develop this disease. If you want to be healthy, you should pay more attention to physical education, do morning exercises and worry less. It is also necessary to eat properly and drink clean water. This will guarantee your good health.
Thrombosis in children
Possible causes of blood clot formation in children:
- thrombophilia - congenital deficiency of anticoagulant blood factors;
- leukemia, other oncological diseases;
- cutaneous fulminant purpura, disseminated intravascular coagulation syndrome (develops with severe intoxication, inflammatory diseases: pancreatitis, peritonitis, etc.);
- the presence of antiphospholipid antibodies, lupus anticoagulant, and other autoantibodies (antibodies to one’s own cells).
Episodes of blood clots in a child should prompt a serious examination to determine the cause.
Is it possible to prevent a blood clot: prevention
Sport is the best prevention of thrombosis.
Every year in Russia alone, hundreds of thousands of people die from stroke. The most common type of stroke is ischemic, caused by a blockage of a blood vessel or a blood clot. It occurs 4 times more often than strokes due to vascular rupture. Is it possible to prevent a blood clot?
- Prevention of thrombosis involves thinning the blood. We need to accelerate it so that there is no stagnation.
- Any physical exercise will help you do this . You should exercise at least 30 minutes a day. It is important to walk a lot in the fresh air.
- People who are inactive most often suffer from stroke , so prevention in the form of daily physical activity is mandatory.
As mentioned above, in order to avoid the appearance of blood clots, you need to follow a drinking regime. You should drink at least two liters of water daily. To be completely sure, you can take medications that improve blood circulation. But this should be done only after consulting a doctor.
Remember : Self-medication is dangerous!
Danger at the gene level - thrombophilia
Genetic analysis allows us to identify polymorphisms in the genes of factors and components of the hemostasis system, which lead to their abnormal synthesis or disruption of functional activity. This allows you to assess the risks of developing cardiovascular pathology and obstetric and gynecological complications, thromboembolism, venous and arterial thrombosis.
In 30-50% of cases, the disease is caused by genetic pathology of blood cells, as well as defects in the blood coagulation system.
Structurally, the hemostasis system is divided into:
- plasma link (coagulation factors and fibrin formation - genes F2, F5, F7, F13, FGB, PAI-1);
- platelet link (platelet adhesion to the vascular wall, vascular contraction, platelet aggregation, thrombus formation - ITGA2, ITGB3 genes).
Functionally, the following systems are distinguished: coagulation, anticoagulation (anticoagulant) and fibrinolysis. Individual polymorphisms make different contributions to the development of pathological conditions.
The most important mutations are in the F2 and F5 genes; they are transmitted according to an autosomal dominant mode of inheritance. As a result of the mutation, factors II and V become resistant to the effects of activated protein C, which leads to uncontrolled thrombus formation in the venous and arterial beds, microcirculation zones, including in the vessels of the placenta.
The influence of other genetic factors is less pronounced, but the combination of several polymorphisms significantly increases the risk of developing thrombophilic conditions.
During pregnancy, the tendency to blood stasis in combination with hypercoagulation predisposes to the development of thrombosis and thromboembolism; in this case, venous thrombosis predominates (about 80%). Genetic factors increase the risk of thromboembolism in pregnant women tenfold, so genetic diagnosis of thrombophilia to prevent obstetric complications should be carried out before pregnancy.
However, it must be remembered that a genetic predisposition to thrombophilia is not a diagnosis, but a tendency to develop thrombosis and other CVDs in certain situations.
In order to understand whether a genetic predisposition is being realized, the condition of patients must be monitored with routine laboratory tests.
In addition to those discussed, an extremely important problem is the prescription of oral contraceptives and menopausal hormone therapy (MHT). It has been shown that hormonal contraception and MHT themselves slightly increase the risk of thrombosis, but when carrying a certain genotype, the danger increases sharply.
According to the National Medical Eligibility Criteria for Contraceptive Methods 2012 and the fourth edition of the “Medical Eligibility Criteria for the Use of Contraceptive Methods” developed by WHO in 2009, identification of thrombogenic mutations is recommended to prevent thrombosis and thromboembolic complications when taking oral contraceptives.
According to the Criteria, in the presence of a thrombogenic Leiden mutation, the use of estrogen-containing drugs is contraindicated (category four of the eligibility criteria). When prescribing progestin-based contraception or copper-containing or hormone-containing intrauterine devices, women with thrombogenic mutations fall into the second category of eligibility criteria (taking the drug under medical supervision).
Indications for genetic analysis:
- Repeated thrombosis.
- Thrombosis of unknown etiology after 50 years.
- A case of thrombosis at any age with a family history.
- Thrombosis of unusual localization (portal, mesenteric, cerebral veins).
- High-risk situations: major surgical interventions; pregnancy and postpartum period; use of hormonal contraception or hormone replacement therapy; long-term immobilization.
What do the results mean?
| Gene | Polymorphism | Interpretation | Additional Research |
| F2 | G20210A | AG/AA – increased concentration of prothrombin in blood plasma. Increased risk of developing thrombosis and thromboebolic complications during pregnancy, when taking oral contraceptives and hormone replacement therapy. Risk of ischemic stroke. Increased likelihood of myocardial infarction in men by 1.5-2 times, in women by 4 times. | PTI INR Prothrombin time thromboelastogram |
| F5 | G1691A | AG/AA – increases hypercoagulability. Increases the risk of developing venous thrombosis and thromboembolism by 20 times (in heterosexuals by 7 times). Increased risks of developing thrombotic complications during pregnancy, when taking oral contraceptives and hormone replacement therapy. | Protein C Protein S APTV Thromboelastogram |
| F7 | G10976A | AG/AA – decrease in factor concentration in the bloodstream by 30%. protective effect regarding the development of thrombosis and myocardial infarction. | Thromboelastogram APTV |
| F13 | G103T | GT/TT risk of developing hemorrhagic stroke, hemarthrosis, hemorrhagic syndrome. Violation of the embryo implantation process, predisposition to recurrent miscarriage. | |
| FGB | G455A | AG/AA - increase in fibrinogen concentration by 20%. Increased risk of developing ischemic stroke, pregnancy pathologies (recurrent miscarriage, FPN) | Thrombin time thromboelastogram |
| PAI-1 | 675 | 4G5G/5G5G – increased risk of developing ischemic stroke, MI, arterial and venous thrombosis. Increased risks of developing pregnancy pathologies - early and late miscarriages, premature abruption of a normally located placenta, FPN, preelampsia, eclampsia. | Protein S Thromboelastogram |
| ITGA2 | C807T | CT/TT - increased platelet aggregation, increased risk of thrombosis and pregnancy complications. Increased risk of developing MI, ischemic stroke, postoperative thrombosis. | Number of platelets |
| ITGB3 | T1565C | TC/CC increased risk of thromboembolism, MI, early miscarriage, thrombocytopenia in newborns. |
Recommendations:
All of the above polymorphisms are the most common causes of congenital (genetic) thrombophilias.
After receiving the test result, the doctor prescribes anticoagulants, as well as drugs that affect platelet function and improve liver function.
Also, all patients who have an increased risk of developing thrombosis are prescribed an antithrombotic diet, from which they exclude: lard, fatty meat, legumes, full-fat milk, hard cheese, parsley, spinach. Preference is given to seafood, root vegetables, berries, dried fruits, seaweed, and ginger.
Ideally, regardless of age and gender, every person should know their genetic map, be examined for a tendency to form blood clots, exclude or establish a hereditary form of thrombophilia, a genetic tendency to develop stroke, myocardial infarction, arterial hypertension and cancer.
It is important to remember that:
— Detection of mutations in these genes does not establish or confirm a diagnosis; however, the lifetime risk of developing the disease in a carrier is 60-90%.
— The absence of frequent mutations in genes does not exclude other, more rare genetic changes.
Interpretation of study results must be carried out in conjunction with other genetic, clinical and laboratory data!
If you have blood clots in your legs, can you walk in heels, smoke and drink alcohol?
If you have thrombosis, it is forbidden to wear heels.
We are always told about the dangers of alcohol and smoking on the body. We can say with confidence that these habits provoke the development of thrombosis. For healthy people, as well as for patients with blood clots in the legs, it is harmful to smoke, drink alcohol and for women to walk in heels. Read more below.
Smoking:
- Doctors who often encounter a similar disease have concluded that tobacco plays a big role in the development of thrombosis.
- A person who smokes puts himself at great risk, as the blood thickens and a blood clot can form in the vessels.
- Accordingly, smoking is also harmful in the presence of thrombosis.
Drinking alcohol is also very dangerous for health:
- When a person is in a normal state, his blood moves through the veins at the correct speed.
- As soon as you drink a little strong alcohol, it begins to thicken and move through the veins at high speed.
- People believe that alcohol thins the blood, but this is not true. The speed of blood flow simply increases.
- At this moment, if there are blood clots in the body, they can break away from their base and death will occur instantly.
Women love to dress well and wear high heels:
- If a woman has varicose veins, then such shoes are strictly prohibited.
- The legs will be constantly under tension and this will cause stagnation of blood in the veins, which will have a detrimental effect on health.
- Also, such shoes can provoke the formation of a blood clot.
- If you already have blood clots in your legs, wearing heels is prohibited!
Sitting for long periods of time also has a negative impact on health. Therefore, for example, office workers and people who like to sit at the computer for a long time need to take breaks every hour for 10-15 minutes.
Advice: Try to move more, smoke less and do not drink alcohol, wear the right orthopedic shoes. This will help protect yourself from unwanted consequences.
How to donate blood for clotting
Determination of bleeding time is carried out using capillary blood; for other clotting tests, material must be taken from a vein.
The tests are carried out on an empty stomach; you can only drink water before the analysis. If you are taking any medications, you should tell your doctor about this, as some medications may affect the results obtained.
By regularly taking hemostasiogram tests, you can promptly diagnose many dangerous ailments.
Increased blood clotting and thrombus formation
Many factors can lead to increased blood clotting, restriction or blockage of blood flow, and as a result, blood clots. Blood clots can travel through arteries and veins, causing serious consequences including sudden death from embolism.
Indications for examination
Normal blood clotting is 2-5 minutes (according to Sukharev). An analysis to determine this indicator (coagulogram, hemostasiogram) is prescribed for:
- diseases of internal organs;
- suspected hereditary hemostatic pathologies;
- pregnancy;
- varicose veins, thrombus formation;
- diabetes mellitus;
- prescribing coagulants;
- during the preoperative and postoperative period.
Risk factors
Increased hemocoagulation often occurs when:
- increased number of blood cells and hemoglobin, radiation, cancer;
- hyperfunction of the spleen, acidification and dehydration of the body, most often associated with poor bowel function;
- increased consumption of sugar and carbohydrates;
- overweight, pregnancy, prolonged bed rest, sedentary lifestyle and sedentary work;
- lack of specific hormones and enzymes, use of birth control pills or hormone replacement therapy.
Sometimes the tendency to hyperclotting is congenital. This pathology is called thrombophilia. It is caused by a congenital decrease in the level of anticoagulants C and S, antithrombin III, coagulation factor VII, heparin cofactor II, dysfibrinogenemia, sickle cell anemia, hyperlipoproteinemia, increased activity of Hageman factors, Rosenthal factors and antihemophilic globulin. With this pathology, patients report similar cases among close relatives. Sometimes hereditary thrombophilias cause miscarriages in women.
Blood thickening in old age threatens to disrupt brain activity, and in pregnant women it can negatively affect the condition of the mother and fetus. Poor rheology leads to ischemia of organs and tissues, which negatively affects the condition of the entire organism.
How to suspect increased coagulability
- A sign indicating increased hemocoagulation is thrombus formation. If you notice painful bluish “vessels” or nodules on the limbs, this is a reason to consult a doctor and be examined for blood clotting indicators.
- Another symptom that should alert you is problems with the functioning of the heart. They should encourage you to get tested.
If the coagulogram indicators do not correspond to the norm, treatment must be started urgently to prevent thromboembolism.
Could there be a blood clot in the arm?
Blood clot in the arm
According to research and the experience of doctors, blood clots can form in various organs and in any part of the human body, including in the arm. When this happens, a person experiences the following symptoms:
- The affected hand is colder than the other. Due to impaired blood formation, the affected hand becomes colder than the other. But such a symptom is difficult to notice on your own.
- Decreased sensitivity. First, bodily sensations become weak, and then pain sensitivity decreases. A person may not even notice when he is burned by hot objects.
- Swelling of the hand. When there is a blood clot in a vein in the arm, it causes swelling. This symptom is almost impossible to ignore, as it brings severe discomfort.
- Increased body temperature. This happens if a blood clot appears in a vein. Body temperature rises slightly. Usually it is kept at 37.5 - 38.0 degrees.
The first signs of a blood clot:
- The person feels quickly exhausted and tired
- Breathing is difficult
- Dizziness and fainting may occur
- Palpitations, headache
The main danger of thrombosis is that often this disease is not traced and is not felt in any way by the human body. Only some external changes may appear in the affected area, but people often do not attach any importance to this. Therefore, it is important to prevent thrombosis: daily physical activity, do not sit in one place for a long time, monitor your weight and nutrition, drink plenty of water. Good luck!
Risk factors for thrombosis
Internal:
- arterial hypertension [7];
- pregnancy, childbirth, postpartum period [3];
- biochemical changes in blood [2,3,5,7];
- vasculitis [2];
- age over 40 years [5];
- congenital thrombophilia, thrombosis, varicose veins of the lower extremities [3,5];
- congestive heart failure [5, 6];
- malignant neoplasms, radiotherapy and chemotherapy [3];
- strokes [3, 6];
- myeloproliferation [2, 5, 7];
- nephrotic syndrome and renal failure [5, 6, 7];
- obesity (BMI over 30) [3];
- myocardial infarction [6];
- diabetes mellitus [6, 7];
- systemic lupus erythematosus [2];
- chronic pulmonary diseases [3];
- enterocolitis [5].
External:
- heroin addiction [2];
- hormonal therapy [3,5];
- dehydration due to vomiting, diarrhea, increased sweating, direct lack of fluid [6];
- immobilization [3];
- travel by plane, bus or in a seated car [3];
- infectious diseases, including COVID-19 [1, 3, 5, 9];
- catheterization of central and peripheral veins [2, 5];
- smoking [6, 7];
- sedentary lifestyle [3];
- operations [3];
- fractures of large bones, other injuries [3];
- taking oral contraceptives [5];
- taking Diazepam, Amiodarone, Vancomycin [2];
- sclerotherapy and thermal ablation [2];
- condition after joint replacement [3];
- holding an awkward position [3].