Many people have probably heard sad stories about someone’s sudden death due to a broken blood clot. Almost everyone understands that a “severed blood clot” is something life-threatening, but at the same time, not everyone knows what a blood clot is, when it forms and in general why and where it “breaks off”. Therefore, now we’ll talk about blood clots and their role in the body.
What are blood clots
Human blood is a multicomponent substance. It consists of plasma and different types of cells: red blood cells, white blood cells and platelets. The first are the so-called red blood cells, which have the role of transporting oxygen throughout the body. Leukocytes are white blood cells. Their task is to protect the body from pathogenic substances that enter the blood. And platelets, due to their specific role, are called “repair cells”. They take part in the formation of blood clots.
Content:
- What are blood clots
- When blood clots do not cure, but cripple
- What is a “detached thrombus”
- When do blood clots break off more often?
- How to protect yourself from dangerous blood clots
The ability of the circulatory system to form blood clots is, without exaggeration, of vital importance. Thrombosis is a kind of protective reaction of the body. If it were not for blood clots, then even the slightest injury would lead to complete blood loss and, consequently, death.
When a lesion occurs on the body of a healthy person, accompanied by hemorrhage, platelets are immediately activated and sent to the wound. The blood repair cells stick together and form a clot, a “patch,” which clogs the damaged vessel. To make protection more reliable, platelets bind to a protein substance – fibrin. Together they create a blockage in the “breakthrough” area. In this way, the body protects itself from blood loss.
After the injury site has healed, the blood clot dissolves without affecting the thickness of the blood. But if something in this mechanism malfunctions, the process of formation and resorption of blood clots is disrupted.
Causes of pathology
In addition to tissue rupture, thromboembolism occurs for the following reasons:
- Due to disruption of blood flow
. Blood clots do not form when blood flows quickly through the vessels, even if the vascular walls are damaged. But a slow current with stagnation provokes their appearance. The root causes of such phenomena are lack of movement, compression of veins and arteries, and varicose veins. - Due to changes in blood composition
. It can become thicker due to lifestyle and environmental influences. Density can be affected by viruses and bacteria, and some medications.
This pathogenic phenomenon is common to many diseases. In some cases it becomes its cause, in others it becomes a complication.
When blood clots do not cure, but cripple
A lack of platelets leads to blood clotting disorders and improper wound healing. If there are too many of these blood cells and they stick together unnecessarily, there is a risk of thrombosis - blockage of blood vessels. In this case, blood circulation is disrupted, causing some organs and tissues of the body to receive less oxygen and nutrients. The World Health Organization has estimated that approximately a quarter of the world's population has a tendency to form blood clots in blood vessels. And this can happen for various reasons.
One of the most common causes leading to the development of thrombosis is vessels with damaged walls. They are perceived by the body as a possible source of danger, so platelets are grouped and sent to “patch” the walls of blood vessels, which ultimately does more harm than good. Vascular walls are damaged, as a rule, due to inflammatory processes - phlebitis (in the veins) or arteritis (in the arteries). Therefore, it is important for people with such disorders to regularly check the condition of blood vessels and blood density.
Another common cause of blood clots is impaired blood flow. With this pathology, in places where the vessel expands or narrows, peculiar “turbulences” can form, where blood clots accumulate.
There is another factor contributing to the development of thrombosis – genetic. Some hereditary diseases affect blood viscosity, making the substance in the vessels thicker. In addition, the thickness of the blood can be affected by taking certain medications, as well as smoking. During pregnancy, if the blood vessels of the placenta are blocked by clots, there is a serious risk to the fetus.
Features of intracardiac localization
Blood clots differ in structure and appearance. In vessels it is customary to distinguish:
- in the arteries - “white” blood clots formed by platelets, leukocytes, fibrin;
- in the veins - “red”, consisting of the same cells + red blood cells;
- hyaline - formed in the capillary bed, do not contain fibrin, it is replaced by proteins.
Cardiac thrombi are mixed, have a motley pattern, a characteristic appearance, and therefore are also called layered. According to their structure, they can be distinguished:
- head (more similar to a “white” blood clot);
- body;
- tail (looks like a “red” blood clot).
The head of the thrombus is attached to the inner wall (endocardial epithelium).
Some properties of intracardiac clots are important in the manifestation of symptoms.
Depending on the ability to move inside the cavity, blood clots can be:
- mobile - move freely in the atria or ventricles, most often formed in the left atrium;
- motionless - one end is attached to the wall, sometimes a “leg” is formed, like in polyps.
In addition, in relation to the cardiac cavity, there are:
- parietal thrombi - more often occurs during an inflammatory process in the endocardium with a transition to the valves, attached to the atrial appendages in case of chronic heart failure, ischemia, to the wall of the aneurysm, leaving a passage for blood flow;
- obstructive - completely block the lumen of the cavity, causing death.
As wall formations grow, they become capable of blocking blood flow
Comparative diagnostics allows us to classify this type as progressive and assume the imminent possibility of complete obturation. Thrombi of the left atrium gradually take on a complete volumetric shape and are called spherical.
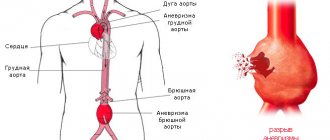
With aneurysms, thrombus formation contributes to an increase in volume and expansion. Such a thrombus is called dilatational; it accelerates the thinning of the wall and its rupture.
What is a “detached thrombus”
We have already figured out what platelets are and what the mechanism of blood clot formation is. It's time to understand what the expression “a blood clot has come off” means.
Clumped platelets can form blood clots in arteries and/or veins. If a blood clot has formed in an artery, this is already a potential risk of ischemia. This is the death of living tissue due to insufficient blood supply. As long as the blood clot is retained on the vessel wall without blocking the blood path, it does not pose a threat to life. But everything changes dramatically as soon as a clot of glued platelets breaks away from the vessel wall and enters any organ with the bloodstream.
If a severed blood clot enters the heart, blocking the lumen of a vessel and preventing normal blood supply, myocardial infarction occurs. A heart attack can occur in any organ that receives blood from an artery.
A heart attack of the kidneys, spleen or even the eye is possible. If a blood clot travels to the brain, it is referred to as a stroke. And if it is in the lungs, a pulmonary embolism occurs. In such cases, it is very important to dissolve the clot as quickly as possible, otherwise death is inevitable. To save the life of a patient with a blood clot in the heart, action must be taken within an hour and a half. In case of a stroke, the first 3-3.5 hours after the incident are decisive.
Treatment
In the early stages of the disease, thrombosis is treated with medications.
When a blood clot has formed, for example, after using a catheter on the arm, effective treatment is possible by administering drugs that dissolve the blood clot (streptokinase, urokinase, etc.).
To relieve pain, non-steroidal painkillers (diclofenac, ibuprofen and others) are used.
If the patient has increased blood viscosity, which is prone to thrombosis, anticoagulants are used. As a rule, heparin is prescribed first, and then drugs with a milder effect (warfarin).
Specific therapy is complemented by antibacterial treatment (sulfonamide and tetracycline groups of antibiotics).
In the later stages, there is nothing more effective than surgery to remove the blood clot (thrombectomy).
The classic version of thrombectomy consists of making an incision over the blood clot, injecting saline solution to soften the blood clot, after which it is removed with a special clamp.
In endovascular surgery, an incision is made along the edge of the blood clot, a catheter is inserted, filled with saline, and pulled back out along with the blood clot.
When do blood clots break off more often?
There are many conditions in which the risk of blood clot formation and rupture increases several times. One of them is atherosclerosis.
People suffering from this disease are at increased risk of heart attack, stroke and thrombosis of the lower extremities, which is complicated by gangrene. The main factor leading to such complications is atherosclerotic plaques that accumulate on the walls of blood vessels.
Sometimes it happens that atherosclerotic plaques rupture, releasing the lipids it contains. Platelets perceive these particles as something similar to a wound and stick to them. This is how large blood clots form, which, if they break off, pose a serious danger to life. To prevent disastrous consequences, patients with atherosclerosis are usually prescribed aspirin, which prevents platelets from sticking together and, consequently, the formation of blood clots.
Atrial fibrillation is a fairly common cardiovascular disease, which also increases the risk of becoming a victim of a broken blood clot. With atrial fibrillation, an irregular contraction of the ventricles of the heart is observed, which is why blood can stagnate in the atrium and blood clots form over time. Statistics indicate that the presence of atrial fibrillation increases the risk of heart attack by almost 6 times. Therefore, people with such cardiac disorders are prescribed anticoagulant drugs (slow down blood clotting). Taking anticoagulants prevents the formation of protein threads (fibrin), which, in fact, bind platelets into huge blood clots.
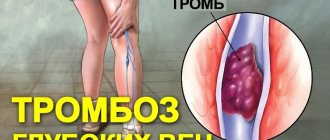
People who lead a sedentary lifestyle may also be at risk of blood clots.
The fact is that due to low physical activity, during sedentary work or when you have to stand in one place for a long time every day, stagnation of blood occurs in the veins. A similar effect is caused by varicose veins. In both cases, the risk of blood clot formation increases. If a clot breaks away from a vein, it will be carried directly into the lungs by the bloodstream, which, as already mentioned, causes a pulmonary embolism. Undesirable consequences can also be prevented by taking anticoagulants.
Diagnosis of pathology
Timely diagnosis will help you avoid surgical intervention and save your life. People who are at risk should undergo the examination.
It is worth systematically diagnosing both young men and women, because the disease is noticeably younger.
The following methods help to identify the presence of a detached blood clot:
| Method name | What is its essence |
| Thrombin generation test | Shows the state of the blood coagulation system |
| Thrombodynamics | Allows you to identify disorders and a tendency to thrombosis in the early stages |
| Thromboelastography | The process of blood clotting and fibrinolysis is determined graphically |
| Prothrombin time test. | Includes indicators for external assessment of blood clotting |
To reduce the risk of a pathological process, it is important to engage in prevention.