Congenital heart defects (CHD) are developmental anomalies that lead to disruption of the morphological structure of the heart, including the valve apparatus and great vessels.
CHDs occur during the period of intrauterine development (usually at 2-8 weeks) as a result of disruption of embryogenesis processes. These anomalies can occur either alone or in combination with each other.
The overall prevalence of this group of diseases is up to 5-8 cases per 1000 births. Congenital defects can be associated with chromosomal abnormalities, however, non-chromosomal congenital heart defects are often diagnosed.
The overall incidence of non-chromosomal congenital heart disease is up to 7 cases per 1000 births, of which up to 3.5% are perinatal losses, 20% are diagnosed prenatally, 5.6% of pregnancies are terminated due to a detected fetal anomaly. Complex non-chromosomal heart defects are less common, approximately 2 cases per 1000 births. The outcome in 8% of cases is perinatal death, 40% are diagnosed in utero, and 14% cause termination of pregnancy.
general description
Congenital heart defects (heart defects) are an abnormal structure of the heart chambers, large vessels or valves (combinations are not uncommon) due to genetic predisposition, intrauterine development disorders, infectious, autoimmune, metabolic and other diseases, injuries received by the mother during pregnancy.
Valve lesions can be congenital (due to disorders of intrauterine development) or acquired, that is, occurring during life under the influence of diseases, infections or injuries. In most cases, complex congenital defects require surgical correction in both children and adults.
Is the noise dangerous?
However, the accuracy of intrauterine diagnostics is only 50%. After all, some complex defects are almost impossible to identify before birth.
Often, in appearance, babies with congenital heart disease cannot be distinguished from healthy children - many of them are plump and active. It is also impossible to judge the presence or absence of a disease by heart murmurs. Up to 50% of complex defects do not make any noise.
To screen for the disease, pediatric cardiologists today use special devices - pulse oximeters, which make it possible to assess the degree of oxygen saturation in the blood and see heart rhythms.
If suspicions remain that the child has heart problems, parents need to perform an echocardiogram (ultrasound of the heart) as early as possible (preferably in the first week of the baby’s life). And in order to sleep peacefully, at the same time, also do an ultrasound of the abdominal cavity and neurosonography (ultrasound of the brain).
If, neither during pregnancy nor after birth, the child has no heart problems and no complaints subsequently arise, then standard examinations by a cardiologist and an ECG (before enrollment in kindergarten and school) are sufficient.
What are the types of congenital heart defects?
- pulmonary valve stenosis
- stenosis of the aortic valve, aortic orifice, subvalvular stenosis;
- mitral stenosis - narrowing of the bicuspid atrioventricular valve;
- Mitral valve insufficiency - incomplete closure of the bicuspid atrioventricular valve;
- Mitral valve prolapse - excessive length of one or two valve leaflets;
- aortic valve insufficiency;
- tricuspid stenosis;
- triscupidal insufficiency;
- defects of the interatrial and interventricular septum;
- anomalies in the development of heart cavities: Ebstein's anomaly, single atrium, single ventricle;
- transposition of large vessels - aorta and pulmonary artery;
- tetralogy of Fallot;
- open arterial (Botallov) duct;
- coarctation of the aorta;
- The most common congenital heart defect is an abnormal communication between the atria—atrial septal defect.
Application of instrumental diagnostic methods
The most common methods used when severe heart pathologies are suspected include:
- X-ray. It involves the introduction of a special contrast agent. The X-ray image helps to track pathological changes in the heart area; electrocardiography. This diagnostic method is used to identify various heart pathologies. When conducting electrocardiography, electric fields arising from myocardial oscillations are recorded. This diagnostic technique helps to identify the presence of abnormalities in the cardiovascular system;
- ultrasonography. This diagnostic method is considered to be one of the safest and most effective.
Diagnosis and treatment of heart disease
Cardiac surgeons can recognize and eliminate the defect in a timely manner. In most cases, x-ray surgeons close the defect using catheter technology without resorting to an incision.
- A defect may appear between the ventricles of the heart - a ventricular septal defect.
- Often the defects are combined with anomalies of the valvular apparatus of the heart or large vessels.
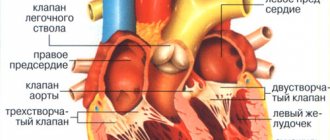
The valvular apparatus of the heart consists of four valves: mitral (bicuspid), tricuspid (three-cuspid), aortic and pulmonary valve. The functioning of the heart depends on the coordinated and correct functioning of these structures.There are two main types of valve disease: valve insufficiency and stenosis.
When there is insufficiency, the valve leaflets do not close completely, leaving a gap through which blood is thrown in the opposite direction to the normal direction. And with stenosis, the valves do not open completely, preventing normal blood flow. Isolated lesions of the heart valves are relatively rare; they are very often observed in other congenital heart defects. For example, a bicuspid acortical valve is often found in people with a patent ductus arteriosus. With this defect, part of the blood (rich in oxygen) from the aorta, which is not closed after the birth of the child, enters the pulmonary artery, causing an overload of the right side of the heart. In children and adolescents, such an abnormal message is most often eliminated without surgery, by installing a “plug” through the catheter.
- Another congenital malformation is stenosis of the descending aorta.
In the thoracic segment, the aorta is attached to the posterior wall, closer to the spine. At this point, the aorta is sometimes significantly narrowed, and the internal organs do not receive enough arterial blood. Previously, this condition, called coarctation of the aorta, could only be corrected with surgery. But today, in most cases, narrowing during coractation of the aorta is eliminated by balloon dilation and installation of a stent frame. It should be emphasized that if valve stenosis is an isolated lesion, it is often eliminated by balloon expansion, in a minimally traumatic way.
How to get a deferment or exemption
To receive a deferment, a conscript must submit to the military registration and enlistment office a medical document that proves that he has a congenital or acquired heart defect that requires treatment both conservatively and surgically. The basis for a delay may also be evidence that the patient is undergoing a rehabilitation period after heart surgery. After the expiration of the recovery period, the conscript appears at the military registration and enlistment office and undergoes a second examination. If it is determined that health is fully restored after the operation, then he is sent to serve in the Armed Forces.
To receive exemption from the army under non-conscription category B, a conscript must have functional class 2, 3, 4 heart failure, severe heart rhythm disturbances, blood flow conduction failure, 2 and 3 degrees of mitral canal prolapse.
Congenital heart disease cannot be a reason for exemption from military service. To receive a non-conscription category or deferment, a conscript must prove the presence of a heart pathology that corresponds to a specific paragraph of Article 42 of the Schedule of Diseases.
How do heart valve diseases manifest?
Most often, patient complaints are nonspecific: shortness of breath, rapid pulse, arrhythmia, fatigue, cyanosis, dizziness.
The severity and nature of symptoms depend on the location of the affected valve. With valve defects of the left half of the heart (mitral and aortic), the lungs are primarily affected, because Blood stagnates in their vessels, which manifests itself as shortness of breath. There are also signs of insufficient blood supply to all organs and systems, primarily the brain and the heart itself. Dizziness, fainting, and angina occur. If the functioning of the valves of the right half of the heart (tricuspid and pulmonary valves) is disrupted, blood stagnates in the vessels of the systemic circulation, i.e. all organs except the lungs are affected. Swelling of the legs and feet, ascites (fluid in the abdominal cavity), enlargement of the liver, etc. develop (LIVER INCREASES, ETC.).
Heart valve defects are dangerous due to their complications and impact on the body, so the main prevention of pathological conditions is regular examinations and treatment of diseases leading to the formation of valve defects.
Military service and arrhythmia
A young man is taken into the army with arrhythmia if it takes the following varieties:
- tachycardia, accompanied by rapid heartbeat;
- bradycardia. With this type of arrhythmia, the heart rate slows down;
- extrasystole. With this pathology, single arrhythmic beats occur. With extrasystole, there is no change in heart rate.
If certain types of arrhythmia are present, the conscript receives the right to be assigned category “D”. These include:
- paroxysmal tachycardia. With this pathology, heart contractions increase sharply. Adverse symptoms such as weakness, fear of death, shortness of breath, and a feeling of pressure in the chest area may appear;
- presence of Adams-Stokes-Morgagni attacks. With this pathology, complications such as loss of consciousness or respiratory arrest may occur;
- weak sinus node syndrome;
- ventricular extrasystole.
Read more about whether people with tachycardia are accepted into the army.
Heart disease. Symptoms
Heart disease. Symptoms in a newborn
Small defects in the structure of the heart may not be detected in the first days and months of life. More significant damage is manifested by the following clinical signs:
- increased or decreased heart rate;
- cyanosis (blue discoloration) of the nasolabial triangle and limbs;
- pallor, sweating and decreased temperature of the feet, palms, and tip of the nose;
- dyspnea;
- frequent regurgitation and difficulty sucking;
- poor weight gain;
- swelling;
- fainting states
- heart murmurs.
Heart disease. Symptoms in a child
An asymptomatic course is typical for minor defects and defects with late manifestation. In other situations, the “set” of clinical signs varies somewhat depending on the type of damage, but some of the most common symptoms can be identified:
- developmental delay (physical);
- shortness of breath during exercise (significant or minor - depends on the severity of the condition);
- cyanosis of the extremities and nasolabial triangle (appearing or worsening during exercise);
- symptom of “drum sticks” and “watch glasses” - characteristic of a number of cardiac, pulmonary, and liver pathologies, thickening of the terminal phalanges of the fingers (sometimes of the toes) and a change in the shape of the nail bed;
- tendency to lung infections;
- arrhythmias;
- chest pain;
- orthopnea (difficulty breathing when lying down);
- swelling of the lower extremities;
- loss of consciousness, etc.
Heart disease. Symptoms in adults
In adults, the congenital defect manifests itself with the signs described above. Especially if the first symptoms appeared after 15–20 years. If the defect was operated on in a timely manner, clinical manifestations may be minor or absent altogether.
Acquired defects behave differently. There are heart defects (for example, mitral stenosis) with very slow progression (the first symptoms that cause concern appear 10 years after diagnosis).
In general, it all depends on the degree of damage to the valve.
The leading symptoms of heart disease in adults are:
- tachycardia and arrhythmias (up to atrial fibrillation);
- chest pain;
- weakness, shortness of breath on exertion and at rest;
- cyanosis of the face and limbs;
- orthopnea;
- attacks of cardiac asthma;
- angina pectoris;
- fainting;
- swelling;
- lung diseases; (up to swelling);
- with right ventricular failure - pain in the right hypochondrium, nausea.
First, characteristic signs of left or right ventricular failure appear (depending on the location of the defect). But over time, doctors are faced with symptoms of both types.