A gastroenterologist treats diseases of the pancreas in Nizhny Novgorod.
The pancreas plays a huge role in the human body.
The pancreas is responsible for metabolic and digestive processes in the body.
The pancreas is the most important secretory organ of the human body.
Today, the most popular diseases of the pancreas are treated in Nizhny Novgorod - pancreatitis, pancreatic necrosis, cancer, cysts and diabetes.
Acute pancreatitis.
Acute pancreatitis is an acute inflammation of the pancreas.
Acute pancreatitis usually appears against the background of a person’s abuse of alcoholic beverages and previous alcohol poisoning.
Acute pancreatitis can also be caused by:
- improper or poor quality nutrition (eating fatty, spicy foods, frequent overeating);
- urolithiasis – the presence of kidney stones;
- heredity;
- trauma to the pancreas: previous operations, injuries, mechanical damage;
- uncontrolled use of medications, antibiotics;
- endocrine diseases, hormonal disorders.
- infections and viruses.
Symptoms of acute pancreatitis in Nizhny Novgorod.
The main symptom of pancreatitis is acute pain in the epigastric region, hypochondrium (right and left). Over time, the pain begins to become encircling, affecting the back, lower and lateral areas of the abdomen.
Detection of acute pancreatitis in Nizhny Novgorod.
If you suspect the development of pancreatitis in the body, the gastroenterologist prescribes the following set of examinations:
- a general blood test, which allows you to find out about the presence of an inflammatory process;
- Ultrasound of the abdominal cavity, which allows you to see changes in the internal organs;
- a general urinalysis to detect amylase in the urine, the presence of which indicates the development of pancreatitis;
- FGDS.
Does the pancreas affect the heart?
The most important organs of the digestive system - the liver, stomach and pancreas - are located in the abdominal cavity in close proximity to the heart. Consequently, any pathology of these organs can negatively affect the heart. In medical practice, there are quite frequent cases of patient requests regarding complaints of pain in the heart, the cause of which is diseases of the digestive organs, in particular the pancreas.
Acute pancreatitis (inflammation of the pancreas), like myocardial infarction, is a serious pathology. If not treated promptly, the patient's condition becomes critical and can result in death. In the acute form of pancreatitis, the pain is sharp and cramping. The pancreas is located behind the stomach and slightly to the left. This can explain the nature of the pain radiating to the heart and left hypochondrium in acute pancreatitis. Often the pain that occurs with this pathology spreads upward, to the region of the heart, and radiates to the left shoulder blade.
Diseases of the pancreas are not the only cause of pain in the heart area. Gallstone disease may not manifest itself for a long time. But sooner or later, especially after intense physical activity or due to stress, gallstones begin to make themselves known. Biliary colic appears, accompanied by arrhythmia and shortness of breath, which are characteristic of cardiovascular pathology.
When pain in the chest was provoked by a heavy meal, it is necessary to assume pancreatitis, despite the anginal localization.
When diagnosing, the doctor pays attention to atypical manifestations of gastrointestinal diseases. For example, gastroesophageal reflux (heartburn) is often accompanied by heart rhythm disturbances and chest pain. According to some reports, this pathology is one of the most common causes of chest pain, along with coronary heart disease.
Extrasystole
In the acute form of pancreatitis, pain that appears in the heart area is often accompanied by cardiac arrhythmias, or extrasystole. Patients often complain of interruptions in the functioning of the heart, especially if the disease progresses and is accompanied by intoxication and general weakness. With pancreatitis, extrasystoles, or arrhythmic contractions of the heart muscle, can be caused by pain. Vomiting and diarrhea accompanying acute pancreatitis also provoke the development of extrasystole.
Tachycardia
Another complication of inflammatory processes in the pancreas can be tachycardia, or rapid heartbeat. In acute pancreatitis, tachycardia can be caused by a fever or pain syndrome, which is accompanied by a high level of stress. Also, tachycardia is often a consequence of low blood pressure, characteristic of acute pancreatitis. In general, tachycardia is a serious condition that requires immediate attention. It may be accompanied by acute lack of air, dizziness, even loss of consciousness.
Chronic pancreatitis.
Chronic pancreatitis is diagnosed when the disease develops as a result of a protracted inflammatory process occurring in the pancreas. Men over 40 are most susceptible to the disease.
Symptoms and causes of chronic pancreatitis in Nizhny Novgorod.
The most common causes of chronic pancreatitis are the presence of cholelithiasis in the patient and excessive consumption of alcoholic beverages.
Eating fatty, low-quality foods, carbonated drinks, and alcohol also contributes to the development of chronic pancreatitis.
The presence of chronic pancreatitis is indicated by cutting pain. Also, belching, vomiting, bloating, problems with bowel movements, lack of appetite, weight loss are symptoms of chronic pancreatitis.
Methods for diagnosing chronic pancreatitis at Only Clinic.
If chronic pancreatitis is suspected, a gastroenterologist at the Only Clinic prescribes the following set of examinations to the patient:
General blood test: with chronic pancreatitis, there is an increase in the concentration of leukocytes in the blood, an increase in the erythrocyte sedimentation rate, and an increase in amylase levels.
- General urinalysis: shows an increase in amylase.
- Ultrasound of the abdominal cavity and pancreas.
- CT, MRI to identify foci of disease and the presence of stones.
Pain and pancreas
Lecture transcript
XXV All-Russian Educational Internet Session for doctors
Total duration: 20:42
00:00
Oksana Mikhailovna Drapkina, Secretary of the Interdepartmental Scientific Council on Therapy of the Russian Academy of Medical Sciences, Doctor of Medical Sciences, Professor:
— The next message will be made by Professor Oleg Samuilovich Shifrin: “Pain and the pancreas.”
Oleg Samuilovich Shifrin, Doctor of Medical Sciences:
— Dear colleagues! I will begin my presentation with a small clinical example. A 55-year-old patient came to our clinic (under the leadership of Academician Vladimir Trofimovich Ivashkin) with complaints of epigastric pain radiating to the back, left hypochondrium, occurring 40-50 minutes after eating, as well as at night. The pain is quite intense, sharply reducing the patient’s quality of life.
From the history of the disease. Considers himself sick for three years when similar pain sensations began to arise after eating. At first less intense, but then increasingly intensifying. From the anamnesis, it was noted that for a long time the man smoked intensively, consuming up to one and a half, two packs of cigarettes per day.
The patient was already diagnosed with chronic pancreatitis at the prehospital stage. Various enzyme preparations containing bile acids were prescribed in combination with proton pump blockers. There was no effect. The patient continued to experience intense pain, including at night. The addition of antispasmodics also did not radically improve the situation.
In our clinic, the patient was diagnosed with a painful form of chronic pancreatitis. Pancreatin tablets that do not contain bile acids, in the form of Mezim 10000, were prescribed as an antianginal agent. Against this background, an almost radical improvement occurred. Pain symptoms have practically disappeared.
Abdominal pain is the most important cardinal symptom of the initial stages of the development of chronic pancreatitis. This slide shows work from the end of the last century, in which, based on an assessment of a significant number of observations, it was established that abdominal pain bothers almost 90% of patients with chronic pancreatitis in the initial stages. At the same time, other symptoms of chronic pancreatitis (diarrhea, symptoms of pancreatic diabetes mellitus, jaundice) are much less likely to bother patients.
02:52
But pain is different. Pain in chronic pancreatitis has different origins. We must evaluate it differently. What may be associated with abdominal pain in chronic pancreatitis? First of all, with the actual inflammation of the pancreas tissue. The inflammatory exudate compresses the nerve endings, naturally causing pain.
If alteration predominates in the process of inflammation, then biologically active substances damage the hyaline membranes of nerve fibers and affect the nerve plexuses. Abdominal pain in these cases will be even more intense.
I gave examples of the etiology of the so-called type A pain. Pain associated directly with inflammation of the pancreas tissue. But with pancreatitis, other pain is often encountered. Fundamentally different pain in nature! Pain associated with the actual complication of inflammation in the tissues of the pancreas.
This pain may be associated with increased pressure in the pancreatic ducts due to obstruction by calcifications or compression of fibrotically altered pancreatic tissue.
When the pressure in the pancreatic ducts increases, the tiled epithelium lining them desquamates. Aggressive pancreatic juice affects the nerve plexuses contained in their wall.
Another cause of this type of pain is pseudocysts, peculiar wounds in the body of the pancreas, where aggressive pancreatic juice also affects the exposed nerve endings.
A common cause of such pain (type B pain): compression of the common bile duct by the enlarged head of the pancreas or stenosis of the duodenum due to the same reason.
Briefly summarizing the main causes of pancreatic pain, we can reduce them to the following factors. Increased intraductal pressure and stretching of the pancreatic capsule. Compression of the pancreatic ducts due to fibrotic changes in the organ tissue. Ischemia of pancreatic tissue. Destruction of ductal epithelium.
05:31
Pain may also be associated with the changes that occur during chronic pancreatitis in other organs. These are, first of all, gastroduodenal ulcers, which arise due to a decrease in the alkalizing role of the bicarbonate solution that the pancreas produces in conditions of illness.
Thrombosis of the splenic vein is possible with the development of acute pancreatitis. Finally, in severe forms of acute pancreatitis, pleurisy may also occur, which also in some cases causes severe abdominal pain.
Pain may also occur due to decreased exocrine pancreatic function. A decrease in the production of enzymes and a decrease in the production of bicarbonate solution by the pancreas leads to excessive acidification of the initial parts of the duodenum, impaired motility and the natural development of such a symptom as flatulence.
Moreover, it is sometimes very difficult for the patient to distinguish what is bothering him: flatulence or pain. These symptoms may subjectively overlap with each other.
At the end of the last century, classical controlled studies were conducted to compare the effect of various types of enzyme preparations on the level of abdominal pain in chronic pancreatitis. This study included thousands of patients. It was found that traditional tablet preparations of pancreatin significantly reduced the pressure in the pancreatic ducts of the pancreas and reduced the level of abdominal pain.
At the same time, microgranular preparations of pancreatin did not significantly reduce the elevated level of pressure in the pancreatic ducts and did not reduce the severity of abdominal pain in patients.
Why is this happening? Enteric-coated pancreatin particles contained in a microgranular preparation, entering the upper duodenum and stomach, cannot be broken down in time due to the fact that the function of producing bicarbonates by the pancreas suffers primarily in exocrine insufficiency.
As a result, acidification of the upper parts of the duodenum occurs. Pancreatin microgranules begin to break down in the deeper parts of the duodenum, where the releasing system no longer works.
08:44
At the same time, pancreatin tablets, in which the particles of the active substance are not protected by an enteric coating, begin to disintegrate and begin their biological function already in the upper parts of the duodenum, where the releasing system operates.
Accordingly, according to the law, the production of pancreatic enzymes by the pancreas decreases through a negative feedback mechanism. The pressure in this organ, in its ducts and in the parenchyma decreases. The level of pain decreases.
Let's consider the algorithm for treating the painful form of chronic pancreatitis, proposed by the American Gastroenterological Association at the end of the last century.
At the first stage, we must confirm the diagnosis. Pain in the upper abdominal cavity is not only caused by pancreatitis. This could be a peptic ulcer, pancreatic cancer, or many other diseases, so the pain from which the patient suffers cannot be reduced only to chronic pancreatitis.
The diagnosis requires confirmation (this is a complex diagnosis). Using modern ultrasound methods, computed tomography, magnetic resonance imaging, and modern laboratory methods, we can and must confirm this diagnosis.
In some rare cases, it is possible to use ERCP, but when referring a patient for this study, it should be remembered that in almost 10% of cases it is complicated by the development of acute pancreatitis, and therefore should be performed only according to strict indications.
Good - the diagnosis of pancreatitis was confirmed. In any case, the patient is prescribed a low-fat diet. The patient must exclude alcohol, I emphasize, for any form of chronic pancreatitis! Both with alcohol and non-alcohol. The patient must avoid smoking. This is the most important pancreatogenic factor, the importance of which, unfortunately, is not yet sufficiently appreciated by either patients or even doctors.
In order for the attending physician to properly assess the patient’s condition, the patient is recommended to keep a daily diary of monitoring his well-being, in which he assesses the level of abdominal pain. If pain persists, the patient can and should use antianginal drugs. For example, such as trimebutine and paracetamol.
11:35
Are these activities ineffective? Then the patient is prescribed a long course of tablets containing pancreatin, and in high doses. These drugs can be combined with inhibitors of gastric secretion: primarily with proton pump blockers. H2 blockers are much less effective here.
Are we not helping the sick? Does he still have abdominal pain? Then the patient should be offered a choice between watchful waiting and surgical treatment. But at the same time, the positive possibilities of surgical treatment and possible complications of surgical treatment must be explained to the patient.
If there is dilatation of the ducts, the patient is sent for drainage operations. If the ducts are not dilated, then surgical denervation of the pancreas or even resection of part of this organ is performed.
So, the main treatment directions in the management of patients with a painful form of chronic pancreatitis. At the first stage, this is a diet, a complete cessation of alcohol consumption (I will add - smoking). Prescription of analgesics. Tableted enzyme preparations in high doses. Firstly, in order to create functional rest of the organ and as a replacement therapy.
Treatment of spastic disorders that naturally occur in chronic pancreatitis from smooth muscle organs, from the bile ducts, from various parts of the intestine. It is advisable to prescribe trimebutine, a drug that has both antispasmodic and analgesic effects.
We must not forget about medical denervation of the pancreas. Well-known cyclic antidepressants can help us here.
Finally, if all these measures are ineffective, the patient is referred for a consultation with an endoscopist and surgeon to decide on further management tactics.
13:55
Our clinic conducted an uncontrolled comparison of the effect on pain of traditional pancreatin tablets in the form of Mezim 10,000 and a microgranular preparation also containing 10,000 units of lipase. The observation period is 4 weeks. The groups of patients were approximately the same type. They consisted of patients with chronic pancreatitis of alcoholic, biliary etiology and mixed etiology.
We were convinced that the tablet preparation of pancreatin reduces the severity of abdominal pain to a greater extent than the microgranular preparation. Moreover, the effect on the level of flatulence turned out to be approximately the same.
It is important to note that the pancreatin tablet preparation caused constipation less frequently than the microgranular preparation. I would like to emphasize that we considered patients with relatively preserved exocrine pancreatic function. They did not have gross violations of the external secretory function in the form of severe diarrhea, malabsorption, and so on.
Prescribing adequate tableted pancreatic enzymes makes it possible to largely avoid the use of antisecretory drugs. This table shows that almost half of the patients to whom we prescribed Mezim 10,000 were able to stop using proton pump blockers.
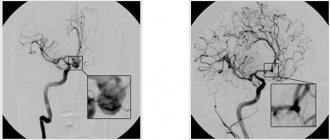
A separate group consists of patients with chronic pancreatitis with severe atherosclerosis of the mesenteric vessels. This slide shows an example of an elderly patient (72 years old) with severe calcification of the mesenteric vessels.
15:59
The management of these patients has some peculiarities. Since such patients are significantly more often diagnosed with gastroduodenal erosive lesions, they should not be prescribed NSAIDs as antianginal drugs, as discussed in the previous lecture.
It is better for these patients to be prescribed antianginal drugs such as paracetamol or trimebutine. They pose a much lesser threat in terms of the development of gastroduodenal bleeding.
A very important aspect is smoking. Smoking, in its importance, is obviously not much inferior to alcohol in terms of its negative pancreatogenic effect. Please note: all our efforts, all our efforts to treat abdominal pain in sick smokers suffering from pancreatitis, were, as a rule, ineffective.
In order for us to help them, they either needed to quit smoking or significantly reduce the number of cigarettes they consumed. At least less than 10 per day - so that their smoker index is low.
Pay attention to this table. The survey was conducted among patients suffering from chronic pancreatitis, Muscovites, usually with higher education.
Everyone knows that smoking negatively affects the lungs. Most people know that smoking has cardiotoxic effects. About half know that smoking has a negative effect on the stomach and potency in men. But only 10%, only three out of thirty patients suffering from chronic pancreatitis, socially active people with higher education, knew that smoking negatively affects the pancreas.
These are, of course, devastating figures that indicate the low effectiveness of our propaganda among patients.
So, let us once again emphasize the possible reasons for the ineffectiveness of antianginal therapy in patients with chronic pancreatitis. These are, first of all, inadequate doses of the drug, when the doctor knows that we should prescribe the medicine one tablet three times a day. This is completely wrong!
We must proceed from the fact that the clinical picture in each specific case is individual. The patient needs to be prescribed the amount of medicine that he needs to eliminate the symptoms of the disease and eliminate the further development of the disease.
Failure of the patient to comply with the treatment regimen. We have encountered cases where, for example, patients took enzyme preparations for pancreatitis half an hour after meals. They explained this by saying that they did not want to harm the stomach. The doctor did not explain at the prehospital stage when to take the drug. It would seem funny if it weren't sad.
Wrong choice of treatment regimen. As I have already given in a clinical example, they try to treat anginal pain in chronic pancreatitis with enzyme preparations containing bile acids.
Wrong diagnosis. Naturally, no drug (neither enzymatic nor secretory) will help with pancreatic cancer. In this case, the patient can only be helped by a timely diagnosis.
Finally, the attending physician should remember that sufficient time is needed to evaluate the effectiveness of the chosen treatment tactics. As a rule, at least 2-4 weeks. This is the only way we can help a patient with chronic pancreatitis suffering from abdominal pain.
Thank you very much.
20:42
Pancreatic necrosis.
Pancreatic necrosis is a severe form of pancreatitis, which results in changes in the parenchyma of the pancreas that are degenerative and destructive in nature.
Pancreatic necrosis is more common at a young age, women are most susceptible to it.
Causes of pancreatic necrosis.
Among the causes of pancreatic necrosis, gastroenterologists most often name cholelithiasis, cholecystitis, unhealthy diet, complications after surgery or injury, abuse of alcohol, nicotine, drugs, infections, viruses.
Symptoms of pancreatic necrosis.
Symptoms of pancreatic necrosis are pain in the abdominal area.
Repeated vomiting, attacks of nausea, constant dry mouth, skin pigmentation, attacks of shortness of breath, even at rest, may also indicate pancreatic necrosis; feeling of weakness, mental restlessness and tension.
Methods for diagnosing pancreatic necrosis.
To diagnose pancreatic necrosis, the same studies and tests are used as for pancreatitis.
First aid and treatment for heart pain
In all pathological conditions, it is necessary, first of all, to relieve pain with the help of antispasmodic intramuscular drugs, such as Papaverine or Platiphylline. Then, after the diagnosis is established, medications are prescribed to treat the pancreas. The most important condition for inflammation of the pancreas is to temporarily provide a state of rest for this organ using enzyme replacement therapy. For patients with pancreatitis, it is important to follow a strict diet that excludes fried foods and high-fat foods.
Complications of self-medication and lack of treatment for pancreatic diseases
Self-treatment of symptoms with painkillers and stomach pills leads to dire consequences. Acute pancreatitis is quickly complicated by the development of infection. Suppuration forms in the organ, and necrosis (death) develops in the gland tissue.
With severe inflammation of the pancreas, the symptoms sharply intensify - respiratory and kidney failure develops, and blood pressure decreases. Chronic pancreatitis can be complicated by the following disorders:
- diabetes;
- hepatitis;
- gastrointestinal bleeding;
- intestinal dysbiosis;
- peritonitis.
If left untreated, pancreatitis and cysts lead to pancreatic cancer. Therefore, self-medication on the Internet or on the advice of pharmacists in a pharmacy is life-threatening.