Types and symptoms of angina
Angina is divided into:
- stable;
- unstable;
- vasospastic.
The first signs of angina pectoris are an attack that begins with a sharp pain in the left side behind the sternum and gradually moves to the forearm and arm. Lasts up to 15 seconds, then subsides. The pain is pressing, squeezing, sometimes there is a feeling of fullness or burning. The attack is accompanied by an increase in pressure, sweating and paleness of the skin appear.
Classification of angina pectoris
Depending on the relationship between attacks and physical activity, angina pectoris is classified as exertional or resting. The latter can occur without the influence of provoking factors, so it is more difficult to control.
Angina pectoris can be divided into two types: stable and progressive. In the first case, the frequency and strength of attacks depends on the amount of physical activity; they are easily eliminated with the help of drug therapy. Progressive angina pectoris practically cannot be corrected with pharmaceutical drugs; the frequency of attacks increases over time.
The following functional classes of stable angina are distinguished:
- Pain appears only with intense or prolonged physical activity.
- The onset of an attack when walking more than 200 m or climbing more than one flight of stairs at a normal pace. With severe emotional stress.
- Pain when walking less than 200 meters or climbing one flight of stairs at a leisurely pace.
- Seizures occur with minor physical exertion or at rest.
There is Prinzmetal's angina or spontaneous (special, vasospastic) angina - caused by a sudden spasm of the coronary arteries. Attacks develop only at rest, at night or early in the morning.
Diagnosis of the disease
Diagnostics begins “from the threshold.” The first step is to collect an anamnesis and interview the patient about the nature of the attack, the duration of the course, and the intensity of the pain syndrome. What actions of the patient or nervous disturbances are the impetus for the occurrence of angina pectoris. The physical condition of the person (including weight) is necessarily assessed, blood pressure is measured and heart rate is calculated. Then the CBC (complete blood count) is examined, including biochemical analysis and blood sugar. An ECG is performed to determine the degree of cardiac ischemia.
Holter monitoring is possible - a monitor is attached to the patient for a day, which shows the work of the heart. Based on the daily readings of the device, the type of cardiac dysfunction, the frequency of attacks and their duration are determined.
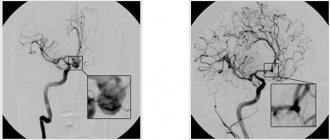
For more severe cases, coronary angiography is performed to diagnose the condition of the vessels. The degree of vasoconstriction and the presence of atherosclerotic lesions are revealed. During this study, an X-ray examination of the heart vessels is performed during the administration of a contrast agent.
In addition to the above, stress tests are sometimes performed on a bicycle ergometer. The doctor evaluates the work of the heart under stress.
Diagnostics
In diagnosing angina, a balanced and competent approach is necessary, because with unstable angina, the patient's condition may worsen until the development of myocardial infarction. Each study must be substantiated.
- ECG
- 24-hour ECG monitoring
- bicycle ergometry or treadmill (stress test with simultaneous ECG recording)
- EchoCG
- stress echocardiography
- coronary angiography
- myocardial scintigraphy
At the EXPERT Clinic, cardiologists are also functional diagnostics doctors. They will weigh all the risks before conducting the examination.
Treatment of angina
The goal of therapy is to relieve the patient from attacks and the risk of complications.
Drug treatment.
With a conservative method of treatment, the following are prescribed:
- short-acting nitrates;
- long-acting nitrates;
- statins;
- antiplatelet agents;
- calcium channel blockers.
To quickly stop an attack (first aid), nitroglycerin is prescribed. It has its effect and improves the patient’s condition in the first three minutes. This effect is achieved by temporarily reducing the myocardial oxygen demand.
Thanks to the constant use of drugs, the condition of the vessels that nourish the heart improves, the risk of plaque formation disappears, and blood flow increases.
Surgery
It is resorted to when therapeutic treatment does not bring positive dynamics or is considered ineffective.
- CABG (coronary artery bypass grafting) is an anastomosis between the artery and the aorta below the site of its narrowing.
- Balloon dilatation of the coronary arteries - a catheter is inserted into the area of narrowing of the coronary vessel, and the inflating balloon flattens the plaque that has narrowed the lumen. The patency of the vessel improves.
It should be remembered that the effect of surgery does not last forever and a person must follow a diet in the future (avoid increasing cholesterol levels) and lead a correct lifestyle.
Treatment of chronic coronary heart disease
Ischemic (coronary) heart disease (CHD), which develops as a result of atherosclerosis of the coronary arteries, is the leading cause of disability and mortality in the working population throughout the world. In Russia, the prevalence of cardiovascular diseases and coronary artery disease is growing, and in terms of mortality from them, our country is one of the first places in the world, which necessitates the use of modern and effective methods of their treatment and prevention by doctors. Among the population of Russia, the prevalence of the main risk factors for the development of coronary artery disease remains high, of which smoking, arterial hypertension, and hypercholesterolemia are the most important.
Atherosclerosis is the main cause of the development of coronary artery disease. It proceeds covertly for a long time until it leads to complications such as myocardial infarction, cerebral stroke, sudden death, or to the appearance of angina pectoris, chronic cerebrovascular insufficiency, and intermittent claudication. Atherosclerosis leads to gradual local stenosis of the coronary, cerebral and other arteries due to the formation and growth of atherosclerotic plaques in them. In addition, such factors as endothelial dysfunction, regional spasms, impaired microcirculation, as well as the presence of a primary inflammatory process in the vascular wall as a possible factor in the formation of thrombosis take part in its development [1]. An imbalance of vasodilating and vasoconstrictor stimuli can also significantly change the state of the tone of the coronary arteries, creating additional dynamic stenosis to the already existing fixed one.
The development of stable angina can be predictable, for example, in the presence of factors that cause an increase in myocardial oxygen demand, such as physical or emotional stress (stress).
Patients with angina pectoris, including those who have already suffered a myocardial infarction, constitute the largest group of patients with coronary artery disease. This explains the interest of practicing physicians in the issues of proper management of patients with angina pectoris and the choice of optimal treatment methods.
Clinical forms of IHD . IHD manifests itself in many clinical forms: chronic stable angina, unstable (progressive) angina, asymptomatic IHD, vasospastic angina, myocardial infarction, heart failure, sudden death. Transient myocardial ischemia, usually resulting from narrowing of the coronary arteries and increased oxygen demand, is the main mechanism for the development of stable angina.
Chronic stable angina is usually divided into 4 functional classes according to the severity of symptoms (Canadian classification).
The main goals of treatment are to improve the patient's quality of life by reducing the frequency of angina attacks, preventing acute myocardial infarction, and improving survival. Antianginal treatment is considered successful in the case of complete or almost complete elimination of angina attacks and the patient’s return to normal activity (angina pectoris not higher than functional class I, when painful attacks occur only under significant loads) and with minimal side effects of therapy [2, 3].
In the treatment of chronic ischemic heart disease, 3 main groups of drugs are used: β-blockers, calcium antagonists, organic nitrates, which significantly reduce the number of angina attacks, reduce the need for nitroglycerin, increase exercise tolerance and improve the quality of life of patients.
However, medical practitioners are still reluctant to prescribe new effective drugs in sufficient doses. In addition, if there is a large selection of modern antianginal and anti-ischemic drugs, outdated and insufficiently effective ones should be excluded. A frank conversation with the patient, an explanation of the cause of the disease and its complications, and the need for additional non-invasive and invasive research methods helps to choose the right treatment method.
According to the results of the ATP-survey (Angina Treatment Patterns), in Russia, when choosing antianginal drugs with a hemodynamic mechanism of action in monotherapy, preference is given to nitrates (11.9%), then b-blockers (7.8%) and calcium antagonists (2 .7%) [4].
β-blockers are the first choice drugs for the treatment of patients with angina pectoris, especially in patients who have had a myocardial infarction, as they lead to a reduction in mortality and the incidence of recurrent infarction. Drugs of this group have been used in the treatment of patients with coronary artery disease for more than 40 years.
β-blockers cause an antianginal effect by reducing the myocardial oxygen demand (due to a decrease in heart rate, lowering blood pressure and myocardial contractility), increasing oxygen delivery to the myocardium (due to increased collateral blood flow, its redistribution in favor of the ischemic layers of the myocardium - subendocardium ), antiarrhythmic and antiaggregation effects, reducing calcium accumulation in ischemic cardiomyocytes.
Indications for the use of β-blockers are the presence of angina, angina with concomitant arterial hypertension, concomitant heart failure, “silent” myocardial ischemia, myocardial ischemia with concomitant rhythm disturbances. In the absence of direct contraindications, β-blockers are prescribed to all patients with coronary artery disease, especially after myocardial infarction. The goal of therapy is to improve the long-term prognosis of a patient with coronary artery disease.
Among β-blockers, propranolol (80–320 mg/day), atenolol (25–100 mg/day), metoprolol (50–200 mg/day), carvedilol (25–50 mg/day), bisoprolol (5 - 20 mg/day), nebivolol (5 mg/day). Cardioselective drugs (atenolol, metoprolol, betaxolol) have a predominantly blocking effect on β1-adrenergic receptors.
One of the most widely used cardioselective drugs is atenolol (tenormin). The initial dose is 50 mg/day. In the future, it can be increased to 200 mg/day. The drug is prescribed once in the morning. In case of severe renal impairment, the daily dose should be reduced.
Another cardioselective β-blocker is metoprolol (Betaloc). Its daily dose is on average 100–300 mg, the drug is prescribed in 2 doses, since the β-blocking effect can be observed for up to 12 hours. At present, long-acting metoprolol preparations have become widespread - betaloc ZOK, metocard, the duration of the effect of which reaches 24 hours.
Bisoprolol (Concor), in comparison with atenolol and metoprolol, has more pronounced cardioselectivity (in therapeutic doses it blocks only β1-adrenergic receptors) and a longer duration of action. It is used once a day at a dose of 2.5–20 mg.
Carvedilol (Dilatrend) has a combined non-selective β-, α1-blocking and antioxidant effect. The drug blocks both β1- and β2-adrenergic receptors, without having its own sympathomimetic activity. Due to the blockade of α1-adrenergic receptors located in the smooth muscle cells of the vascular wall, carvedilol causes pronounced vasodilation. Thus, it combines β-adrenergic blocking and vasodilating activity, which is mainly responsible for its antianginal and anti-ischemic effect, which persists with long-term use. Carvedilol also has a hypotensive effect and inhibits the proliferation of smooth muscle cells, which plays a proatherogenic role. The drug is able to reduce the viscosity of blood plasma, aggregation of erythrocytes and platelets. In patients with impaired left ventricular (LV) function or circulatory failure, carvedilol has a beneficial effect on hemodynamic parameters (reduces pre- and afterload), increases ejection fraction and reduces LV size. Thus, the administration of carvedilol is indicated primarily for patients with coronary artery disease who have suffered a myocardial infarction, with heart failure, since in this group of patients its ability to significantly improve the prognosis of the disease and increase life expectancy has been proven. When comparing carvedilol (average daily dose 20.5 mg) and atenolol (average daily dose 25.9 mg), it was shown that both drugs, prescribed 2 times a day, are equally effective in the treatment of patients with stable angina pectoris [5]. One of the guidelines for the adequacy of the dose of beta-blockers used is a decrease in heart rate at rest to 55–60 beats/min. In some cases, in patients with severe angina, resting heart rate may be reduced to less than 50 beats/min.
Nebivolol (nebilet) is a new selective β1-blocker that also stimulates the synthesis of nitric oxide (NO). The drug causes hemodynamic unloading of the heart: it reduces blood pressure, pre- and afterload, increases cardiac output, and increases peripheral blood flow. Nebivolol is a b-blocker with unique properties, which lie in the ability of the drug to participate in the process of synthesis of relaxing factor (NO) by endothelial cells. This property gives the drug an additional vasodilating effect. The drug is used primarily in patients with arterial hypertension with attacks of angina pectoris.
Celiprolol (200–600 mg/day) - a third-generation β-blocker - differs from other β-blockers in its high selectivity, moderate stimulation of β2-adrenergic receptors, direct vasodilating effect on blood vessels, modulation of the release of nitric oxide from endothelial cells, and the absence of adverse metabolic effects. The drug is recommended for patients with coronary artery disease with chronic obstructive pulmonary diseases, dyslipidemia, diabetes mellitus, and peripheral vascular diseases caused by tobacco smoking [6]. Celiprolol (200–600 mg/day), atenolol (50–100 mg/day), propranolol (80–320 mg/day) have comparable antianginal efficacy and equally increase exercise tolerance in patients with stable angina pectoris.
β-blockers should be given preference when prescribed to patients with coronary artery disease if there is a clear connection between physical activity and the development of an angina attack, with concomitant arterial hypertension; the presence of rhythm disturbances (supraventricular or ventricular arrhythmia), previous myocardial infarction, severe anxiety. Most of the adverse effects of β-blockers are due to blockade of β2 receptors. The need to monitor the prescription of β-blockers and the side effects encountered (bradycardia, hypotension, bronchospasm, increased signs of heart failure, heart block, sick sinus syndrome, fatigue, insomnia) lead to the fact that the doctor does not always use these drugs. The main medical errors when prescribing β-blockers are the use of small doses of drugs, their administration less frequently than necessary, and the discontinuation of drugs when a heart rate at rest is less than 60 beats/min. One should also keep in mind the possibility of developing withdrawal syndrome, and therefore β-blockers must be discontinued gradually.
Calcium channel blockers (calcium antagonists). The main point of application of drugs of this group at the cellular level are slow calcium channels, through which calcium ions pass into the smooth muscle cells of blood vessels and the heart. In the presence of calcium ions, actin and myosin interact, ensuring contractility of the myocardium and smooth muscle cells. In addition, calcium channels are involved in the generation of pacemaker activity of sinus node cells and conduction of impulses through the atrioventricular node.
It has been established that the vasodilating effect caused by calcium antagonists occurs not only through a direct effect on the smooth muscles of the vascular wall, but also indirectly, through potentiation of the release of nitric oxide from the vascular endothelium. This phenomenon has been described for most dihydropyridines and isradipine, and to a lesser extent for nifedipine and non-hydropyridine drugs. For long-term treatment of angina from dihydropyridine derivatives, it is recommended to use only prolonged dosage forms or long-acting generations of calcium antagonists. Calcium channel blockers are powerful vasodilators; they reduce myocardial oxygen demand and dilate coronary arteries. The drugs can be used for vasospastic angina and concomitant obstructive pulmonary diseases. Additional indications for the prescription of calcium antagonists are Raynaud's syndrome, as well as (for phenylalkylamines - verapamil and benzodiazepines - diltiazem) atrial fibrillation, supraventricular tachycardia, hypertrophic cardiomyopathy. The following calcium antagonists are used in the treatment of coronary heart disease: nifedipine, immediate action 30–60 mg/day (10–20 mg 3 times) or prolonged action (30–180 mg once); immediate-release verapamil (80–160 mg 3 times daily); or prolonged action (120–480 mg once); immediate-release diltiazem (30–60 mg 4 times a day) or long-acting (120–300 mg/day once); long-acting drugs amlodipine (5–10 mg/day once), lacidipine (2–4 mg/day).
Activation of the sympathoadrenal system by dihydropyridines (nifedipine, amlodipine) is currently considered as an undesirable phenomenon and is considered the main reason for a slight increase in mortality in patients with coronary artery disease when taking short-acting dihydropyridines for unstable angina, acute myocardial infarction and, apparently, with long-term use in patients with stable angina pectoris . In this regard, it is currently recommended to use retard and prolonged forms of dihydropyridines. They have no fundamental differences in the nature of pharmacodynamic action with short-acting drugs. Due to gradual absorption, they are devoid of a number of side effects associated with sympathetic activation, so characteristic of short-acting dihydropyridines.
In recent years, evidence has emerged indicating the possibility of slowing down damage to the vascular wall with the help of calcium antagonists, especially in the early stages of the development of atherosclerosis.
Amlodipine (Norvasc, Amlovas, Nordipine) is a third generation calcium antagonist from the group of dihydropyridines. Amlodipine dilates peripheral blood vessels and reduces cardiac afterload. Due to the fact that the drug does not cause reflex tachycardia (since the sympathoadrenal system is not activated), energy consumption and myocardial oxygen demand are reduced. The drug dilates the coronary arteries and increases the supply of oxygen to the myocardium. Antianginal effect (reducing the frequency and duration of angina attacks, daily requirement for nitroglycerin), increasing tolerance to physical activity, improving systolic and diastolic heart function in the absence of a depressing effect on the sinus and atrioventricular node and other elements of the conduction system of the heart put the drug in one of the first places in the treatment of angina pectoris.
Lacidipine, a third-generation drug from the class of calcium antagonists, has high lipophilicity, interaction with the cell membrane, and independence of tissue effects from its concentration. These factors are leading in the mechanism of antiatherosclerotic action. Lacidipine has a positive effect on the endothelium, inhibits the formation of adhesion molecules, proliferation of smooth muscle cells and platelet aggregation. In addition, the drug is able to inhibit the peroxidation of low-density lipoproteins, i.e., it can affect one of the early stages of plaque formation.
The European Lacidipine Study on Atherosclerosis (ELSA) compared the intima-media thickness of the carotid artery in 2334 patients with arterial hypertension during 4 years of therapy with lacidipine or atenolol. In the patients included in the study, the carotid arteries were initially normal and/or altered. Treatment with lacidipine was accompanied by a significantly more pronounced decrease in intima-media thickness, both at the level of the bifurcation and the common carotid artery, compared to atenolol. During treatment with lacidipine compared with atenolol, the increase in the number of atherosclerotic plaques in patients was 18% less, and the number of patients in whom the number of plaques decreased was 31% more [7].
Thus, calcium antagonists, along with pronounced antianginal (anti-ischemic) properties, can have an additional anti-atherogenic effect (stabilization of the plasma membrane, preventing the penetration of free cholesterol into the vessel wall), which allows them to be prescribed more often to patients with stable angina pectoris with damage to arteries of different localizations. Currently, calcium antagonists are considered second-line drugs in patients with angina pectoris, following β-blockers. As monotherapy, they can achieve the same pronounced antianginal effect as β-blockers. The undoubted advantage of β-blockers over calcium antagonists is their ability to reduce mortality in patients who have had myocardial infarction. Studies of the use of calcium antagonists after myocardial infarction have shown that the greatest effect is achieved in individuals without severe left ventricular dysfunction, suffering from arterial hypertension, and having had a myocardial infarction without a Q wave.
Thus, the undoubted advantage of calcium antagonists is a wide range of pharmacological effects aimed at eliminating the manifestations of coronary insufficiency: antianginal, hypotensive, antiarrhythmic. Therapy with these drugs also has a beneficial effect on the course of atherosclerosis.
Organic nitrates . The anti-ischemic effect of nitrates is based on a significant change in hemodynamic parameters: a decrease in pre- and afterload of the left ventricle, a decrease in vascular resistance, including coronary arteries, a decrease in blood pressure, etc. The main indications for taking nitrates are angina pectoris and rest in patients with coronary artery disease (also in in order to prevent them), attacks of vasospastic angina, attacks of angina, accompanied by manifestations of left ventricular failure.
Sublingual nitroglycerin (0.3–0.6 mg) or nitroglycerin aerosol (Nitromint 0.4 mg) is intended for the relief of acute attacks of angina due to the rapid onset of action. If nitroglycerin is poorly tolerated, nitrosorbide, molsidomine or the calcium antagonist nifedipine can be used to relieve an attack of angina, chewing or dissolving the tablets when taking them under the tongue.
Organic nitrates (preparations of isosorbide dinitrate or isosorbide-5-mononitrate) are used to prevent angina attacks. These drugs provide long-term hemodynamic unloading of the heart, improve blood supply to ischemic areas and increase physical performance. They try to prescribe them before physical activity that causes angina. Of the drugs with proven effectiveness, the most studied are cardiquet (20, 40, 60 and 120 mg/day), nitrosorbide (40–80 mg/day), olicard retard (40 mg/day), mono poppy (20–80 mg/day ), mono mac depot (50 and 100 mg/day), efox long (50 mg/day), mono cinque retard (50 mg/day). For patients with stable angina pectoris class I-II, intermittent administration of nitrates is possible before situations that can cause an attack of angina. For patients with more severe angina pectoris class III-IV, nitrates should be prescribed regularly; In such patients, one should strive to maintain the effect throughout the day. In case of class IV angina (when angina attacks can also occur at night), nitrates should be prescribed in such a way as to ensure an effect throughout the day [8].
Nitrate-like drugs include molsidomine (Corvaton, Sidnopharm, Dilasidom), a drug that differs from nitrates in chemical structure, but is no different from them in its mechanism of action. The drug reduces vascular wall tension, improves collateral circulation in the myocardium, and has anti-aggregation properties. Comparable doses of isosorbide dinitrate and corvatone are 10 mg and 2 mg, respectively. The effect of Corvaton appears after 15–20 minutes, the duration of action is from 1 to 6 hours (on average 4 hours). Corvaton retard 8 mg is taken 1-2 times a day, since the effect of the drug lasts more than 12 hours.
The weakness of nitrates is the development of tolerance to them, especially with long-term use, and side effects that complicate their use (headache, palpitations, dizziness), caused by reflex sinus tachycardia. Transdermal forms of nitrates in the form of ointments, patches and discs, due to the difficulty of dosing them and the development of tolerance to them, have not found widespread use. It is also unknown whether nitrates improve the prognosis of a patient with stable angina with long-term use, which makes the advisability of their use in the absence of angina pectoris (myocardial ischemia) questionable.
When prescribing drugs with a hemodynamic mechanism of action in elderly patients, the following rules should be observed: start treatment with lower doses, carefully monitor unwanted effects, and always consider changing the drug if it is poorly tolerated and insufficiently effective.
Combination therapy . Combination therapy with antianginal drugs in patients with stable angina of class III-IV is carried out for the following indications: impossibility of selecting effective monotherapy; the need to enhance the effect of monotherapy (for example, during periods of increased physical activity of the patient); correction of unfavorable hemodynamic changes (for example, tachycardia caused by nitrates or calcium antagonists from the dihydropyridine group); when angina is combined with arterial hypertension or heart rhythm disturbances that are not compensated for in cases of monotherapy; in case of patient intolerance to generally accepted doses of drugs during monotherapy, small doses of drugs can be combined to achieve the desired effect.
The synergism of the mechanisms of action of various classes of antianginal drugs is the basis for assessing the prospects of their combinations. When treating a patient with stable angina, doctors often use various combinations of antianginal drugs (β-blockers, nitrates, calcium antagonists). In the absence of effect from monotherapy, combination therapy is often prescribed (nitrates and β-blockers; β-blockers and calcium antagonists, etc.).
The results of the ATP-survey study (review of the treatment of stable angina) showed that in Russia 76% of patients receive combination therapy with hemodynamic drugs, while in more than 40% of cases - a combination of nitrates and b-blockers [4]. However, their additive effects have not been confirmed in all studies. The guidelines of the European Society of Cardiology (1997) indicate that if one antianginal drug is ineffective, it is better to first evaluate the effect of another, and only then use the combination [9]. The results of pharmacological controlled studies do not confirm that combination therapy with a beta-blocker and a calcium antagonist is accompanied by a positive additive and synergistic effect in the majority of patients with coronary artery disease. Prescribing 2 or 3 drugs in combination is not always more effective than therapy with one drug at an optimal dose [10]. We must not forget that the use of multiple drugs significantly increases the risk of adverse events associated with effects on hemodynamics.
The modern approach to combination therapy of patients with stable angina pectoris implies the advantage of combining antianginal drugs with multidirectional effects: hemodynamic and cytoprotective.
The main disadvantages of domestic pharmacotherapy for stable angina include the often erroneous, according to modern concepts, choice of a group of antianginal drugs (as a rule, nitrates are prescribed (80%)), the frequent use of clinically insignificant dosages and the unreasonable prescription of combination therapy with a large number of antianginal drugs [4] .
Metabolic agents. Trimetazidine (preductal) causes inhibition of fatty acid oxidation (by blocking the enzyme 3-ketoacyl-coenzyme A-thiolase) and stimulates the oxidation of pyruvate, i.e., it switches myocardial energy metabolism to glucose utilization. The drug protects myocardial cells from the adverse effects of ischemia, while reducing intracellular acidosis, metabolic disorders and damage to cell membranes. A single dose of trimetazidine is not able to relieve or prevent an attack of angina. Its effects are observed mainly during combination therapy with other antianginal drugs or during a course of treatment. Preductal is effective and well tolerated, especially in groups at high risk of developing coronary complications, such as patients with diabetes mellitus, the elderly and those with left ventricular dysfunction.
The combination of preductal with propranolol was significantly more effective than the combination of this β-blocker with nitrate. Trimetazidine (preductal 60 mg/day), preductal MB (70 mg/day) have an anti-ischemic effect, but more often they are used in combination with basic hemodynamic antianginal drugs.
In Russia, a multicenter, single-blind, randomized, placebo-controlled, parallel-group study, TAST (Trimetazidin in patients with Angina in Combination Therapy), was conducted, which included 177 patients suffering from class II-III angina, partially relieved by nitrates and β-blockers, to evaluate the effectiveness of the preductal in combination therapy with nitrates or β-blockers. Evaluation of the effectiveness of treatment was carried out according to the following criteria: time until the onset of ST segment depression by 1 mm during stress tests, time of onset of angina pectoris, increase in the duration of the stress test. It was found that the preductal significantly increased these indicators. There are a number of clinical situations in which trimetazidine, apparently, can be the drug of choice in elderly patients, with circulatory failure of ischemic origin, sick sinus syndrome, with intolerance to antianginal drugs of the main classes, as well as with restrictions or contraindications to their use [eleven].
Drugs with antianginal properties include amiodarone and other “metabolic” drugs (ranolazine, L-arginine), as well as ACE inhibitors, selective heart rate inhibitors (ivabradine, procolaran). They are used mainly as an adjuvant therapy, prescribed in addition to the main antianginal drugs [12, 17].
The problem of drug treatment of patients with coronary artery disease is the patients’ insufficient adherence to the chosen therapy and their insufficient willingness to consistently change their lifestyle. During drug treatment, proper regular contact between the doctor and the patient is necessary, informing the patient about the nature of the disease and the benefits of prescribed drugs to improve the prognosis. When trying to influence the prognosis of a patient’s life with the help of drug therapy, the doctor must be sure that the medications he prescribes are actually taken by the patient, and in appropriate doses and according to the recommended treatment regimen.
Surgery . If drug therapy is ineffective, surgical treatment methods are used (myocardial revascularization procedures), which include: percutaneous transluminal coronary angioplasty, implantation of coronary stents, coronary artery bypass surgery. In patients with coronary artery disease, it is important to determine individual risk based on clinical and instrumental indicators, which depends on the corresponding clinical stage of the disease and the treatment provided. Thus, the maximum effectiveness of coronary bypass surgery was observed in patients with the highest preoperative risk of developing cardiovascular complications (with severe angina and ischemia, extensive lesions of the coronary arteries, impaired LV function). If the risk of complications of coronary artery disease is low (single artery disease, absence or mild ischemia, normal LV function), surgical revascularization is usually not indicated until the ineffectiveness of drug therapy or coronary angioplasty has been established. When deciding whether to use coronary angioplasty or coronary bypass surgery to treat patients with damage to multiple coronary arteries, the choice of method depends on the anatomical features of the coronary bed, LV function, the need to achieve complete myocardial revascularization and patient preferences [13].
Thus, with the methods of combating cardiovascular diseases that exist today (Table), it is important for the doctor to be aware of the latest advances in medicine and make the right choice of treatment method.
For questions regarding literature, please contact the editor.
D. M. Aronov , Doctor of Medical Sciences, Professor V. P. Lupanov , Doctor of Medical Sciences, State Research Center for Preventive Medicine of the Ministry of Health of the Russian Federation, Institute of Clinical Cardiology named after. A. L. Myasnikov Russian Cardiological Research and Production Complex of the Ministry of Health of the Russian Federation, Moscow
Forecast and prevention of angina pectoris
The basis for preventing angina pectoris is proper nutrition and exercise. The diet should consist of proteins, vegetable fats, and complex carbohydrates. The consumption of alcohol and trans fats (fast food) should be avoided. Give preference to white meat, fish and seafood.
Regular physical activity should be present in the life of every person, this could be swimming, team sports, fitness, running or just walking. Its intensity is determined by the person’s health status; if you have chronic diseases, you should consult your doctor about the types of physical activity acceptable to you.
If you follow all the doctor’s recommendations, angina pectoris can be controlled, but, unfortunately, most patients ignore lifestyle instructions, which can lead to a worsening of the condition.