Hypertensive crisis (HC) is an extremely severe manifestation of arterial hypertension, which develops due to a violation of the mechanism of blood pressure regulation. The main manifestation of GC is a sharp sudden increase in blood pressure (BP), accompanied by a significant deterioration in renal and cerebral circulation. For this reason, the likelihood of severe cardiovascular complications increases (myocardial infarction, stroke, acute coronary failure, dissecting aortic aneurysm, subarachnoid hemorrhage, acute renal failure, pulmonary edema, acute left ventricular failure accompanied by pulmonary edema, etc.).
General information about hypertensive crisis
A sudden increase in blood pressure above generally accepted values in a short period of time should alert you.
This condition can develop in any person exposed to overexertion, emotional shock, and even as a consequence of an acute infectious disease.
Pathogenesis
Neurohumoral mechanisms of the development of hypertensive crisis are important. Overstimulation of the RAAS initiates a vicious chain reaction that includes vascular damage, tissue ischemia, and further overproduction of renin. The body produces excessive amounts of angiotensin II, catecholamines, vasopressin, aldosterone, endothelin-1, and thromboxane. But there are not enough endogenous vasodilators. Therefore, local regulation of peripheral resistance. If blood pressure gradually increases and reaches an individual limit, endothelial regulation of vascular tone is disrupted.
As a result of hyperperfusion, following endothelial damage, fibrinoid necrosis of arterioles develops, vascular permeability increases, which leads to perivascular edema. An important aspect of clinical manifestations and prognosis is the concomitant activation of platelets and the coagulation system, which, in combination with the loss of fibrinolytic activity by the endothelium, contributes to disseminated intravascular coagulation.
Mechanism of development and causes of hypertensive crisis
It may appear as follows:
- Short-term and unexpected manifestation of the following symptoms: pain in the temporal and other areas of the head, difficulty breathing, high blood pressure.
- Increased pressure, discomfort or pain in the heart and occipital area, extraneous noise in the ears.
The causes of hypertensive crisis are divided into two groups. In the first:
- diseases of the brain and cervical spine of any origin;
- pathologies of the cardiovascular system: coronary disease, atherosclerosis, arterial hypertension, heart failure;
- diseases of the endocrine system (hyperthyroidism, diabetes, etc.);
- respiratory tract diseases (bronchial asthma);
- pathologies of the kidneys and urinary system (pyelonephritis, glomerulonephritis, etc.).
The second group (trigger) risk factors include:
- stress;
- physical fatigue;
- taking tonic medications;
- smoking;
- alcohol consumption;
- acute attack of angina.
Men are more predisposed to hypertensive crisis than women, especially over the age of 50-55 years.
GBUZ NO "Pavlovsk Central District Hospital"
Emergency care for acute life-threatening conditions
In our country, up to 80% of deaths occur outside of medical organizations - at home, at work, in the country, in public and other places. Most of them occur suddenly or by the mechanism of sudden death. Statistics show that many patients (or their relatives) call an emergency doctor late, which reduces the likelihood of rescue.
By mastering the necessary first aid skills in the form of self- or mutual assistance (on the part of people surrounding a person who finds himself in such a critical condition), in most cases the patient’s life can be saved.
Often, up to 30-50%, a life-threatening complication with a dangerous fatal outcome may be the first and last manifestation of these diseases (complications).
FIRST AID for a heart attack
Characteristic signs (symptoms) of a heart attack (myocardial infarction):
• sudden (paroxysmal) pressing, squeezing, burning, aching pain in the chest (behind the sternum) lasting more than 5 minutes;
• similar pains are often observed in the left shoulder (forearm), left shoulder blade, left half of the neck and lower jaw, both shoulders, both arms, the lower part of the sternum along with the upper abdomen;
• lack of air, shortness of breath, severe weakness, cold sweat, nausea often occur together, sometimes follow or precede discomfort/pain in the chest; often these manifestations of the disease develop against the background of physical or psycho-emotional stress, but more often with some interval after them.
Uncharacteristic signs that are often confused with a heart attack:
• stabbing, cutting, pulsating, boring, constant aching pain for many hours and not changing its intensity in the heart area or in a specific clearly defined area of the chest
Algorithm of emergency actions in case of a heart attack (advice to the patient) - a reminder for the patient
If you or someone else suddenly has the above characteristic signs of a heart attack, even with weak or moderate intensity, which last more than 5 minutes, do not hesitate, immediately call an ambulance team. Do not wait more than 10 minutes - in such a situation it is life-threatening.
Remember that being intoxicated in this life-threatening situation is not a reasonable excuse for delaying calling an ambulance. If you have symptoms of a heart attack and there is no way to call an ambulance, then ask someone to take you to the hospital - this is the only right decision. Never drive yourself unless you have no other choice.
In the most optimal scenario, if a heart attack occurs, you must follow the instructions received from your attending physician; if there are no such instructions, then you must act according to the following algorithm:
• Immediately after an attack occurs, sit down (preferably in a chair with armrests) or lie down in bed with the head of the bed raised, take 0.25 g of acetylsalicylic acid (aspirin) (chew the tablet, swallow) and 0.5 mg of nitroglycerin (spray one inhalation dose into the cavity mouth while holding your breath, place one tablet/capsule under the tongue, first bite the capsule, do not swallow); free your neck and provide fresh air (open the vents or windows).
• If after 5-7 min. After taking acetylsalicylic acid (aspirin) and nitroglycerin, pain persists, it is imperative (life-saving) to call an ambulance and take nitroglycerin a second time.
• If pain persists 10 minutes after taking the second dose of nitroglycerin, it is necessary to take nitroglycerin a third time.
• If after the first or subsequent doses of nitroglycerin there is severe weakness, sweating, shortness of breath, you need to lie down, raise your legs (on a bolster, etc.), drink 1 glass of water and then, as with a severe headache, do not take nitroglycerin.
• If the patient has previously taken medications that lower cholesterol levels in the blood from the statin group (simvastatin, lovastatin, fluvastatin, pravastatin, atorvastatin, rosuvoastatin), give the patient his usual daily dose and take the drug with you to the hospital.
Attention ! A patient with a heart attack is strictly forbidden to get up, walk, smoke or eat until the doctor’s special permission;
You should not take aspirin (acetylsalicylic acid) if you are intolerant to it (allergic reactions), as well as with obvious or worsening peptic ulcers of the stomach and duodenum;
Nitroglycerin should not be taken if there is severe weakness, sweating, or if there is severe headache, dizziness, or acute impairment of vision, speech, or coordination of movements.
FIRST AID for acute cerebrovascular accident
The main signs (symptoms) of acute cerebrovascular accident:
• numbness, weakness, “disobedience” or paralysis (immobilization) of an arm, leg, half of the body, distortion of the face and/or drooling on one side;
• speech disorders (difficulties in choosing the right words, understanding speech and reading, slurred and unclear speech, up to complete loss of speech);
• disturbances or loss of vision, double vision, difficulty focusing;
• imbalance and coordination of movements (feelings of “swaying, sinking, body rotation, dizziness”, unsteady gait up to falling);
• unusual severe headache (often after stress or physical exertion);
• confusion or loss of consciousness, uncontrollable urination or bowel movements.
If any of these signs suddenly appear, call an ambulance immediately, even if these manifestations of the disease were observed for only a few minutes
Patient Reminder
1. Call an ambulance immediately, even if these manifestations of the disease were observed for only a few minutes
2. Before the arrival of the emergency medical team:
• If the patient is unconscious, place him on his side, remove removable dentures (food debris, vomit) from the mouth, make sure that the patient is breathing.
• If the victim is conscious, help him to a comfortable sitting or semi-sitting position in a chair or on a bed, placing pillows under his back. Provide fresh air. Unbutton your shirt collar, belt, waistband, and remove tight clothing.
• Measure your blood pressure if its upper level exceeds 220 mmHg. Art., give the patient a drug that lowers blood pressure, which he took before.
• Measure your body temperature. If the temperature is 38° or more, give the patient 1 g of paracetamol (2 tablets of 0.5 g, chew, swallow), (if paracetamol is not available, do not give other antipyretic drugs!).
• Put ice on your forehead and head, you can take food from the freezer, put in waterproof bags and wrapped in a towel.
• If the patient has previously taken medications that lower cholesterol levels in the blood from the statin group (simvastatin, lovastatin, fluvastatin, pravastatin, atorvastatin, rosuvastatin), give the patient the usual daily dose.
• If the victim has difficulty swallowing and saliva drips from his mouth, tilt his head towards the weaker side of the body and blot the dripping saliva with clean tissues.
• If the victim is unable to speak or has slurred speech, reassure and reassure him that the condition is temporary. Hold his hand on the non-paralyzed side, stop him from trying to talk, and don't ask questions that require an answer. Remember that although the victim cannot speak, he is aware of what is happening and hears everything that is said around him.
FIRST AID for hypertensive crisis
Hypertensive crisis is a condition manifested by high blood pressure (BP) (systolic or “upper” blood pressure, usually more than 180 mm Hg; diastolic or “lower” blood pressure - more than 100 mm Hg) and the following main symptoms:
• headache, often in the occipital region, or heaviness and noise in the head;
• flashing “flies”, a veil or a net before the eyes;
• nausea, feeling of exhaustion, overwork, internal tension;
• shortness of breath, weakness, constant monotonous aching pain/discomfort in the heart area, sometimes the appearance or increase of pastiness/swelling of the skin of the face, arms, legs.
Algorithm for emergency actions in case of hypertensive crisis
(advice to the patient) – a reminder for the patient
If symptoms of a hypertensive crisis appear, you must:
• remove bright light, ensure peace, access to fresh air (unbutton your shirt collar, ventilate the room, etc.);
• measure blood pressure (see the method for measuring blood pressure at the end of this section) and if its “upper” level is higher than or equal to 160 mm Hg, you must take an antihypertensive drug previously recommended by your doctor. In the absence of an antihypertensive drug recommended by a doctor or when a blood pressure level is registered above 200 mm Hg. urgently need to call an ambulance.
• before the arrival of emergency medical services, it is necessary, if possible, to sit in a chair with armrests and take a hot foot bath (put your feet in a container of hot water).
Attention! A patient with a hypertensive crisis is prohibited from any sudden movements (suddenly standing up, sitting down, lying down, bending over), pushing hard or any physical activity.
• 40-60 minutes after taking the medicine recommended by the doctor, it is necessary to re-measure blood pressure and if its level has not decreased by 20-30 mm Hg. from the initial state and/or the condition has not improved - urgently call an ambulance.
• If you feel better and your blood pressure decreases, you need to rest (lie in bed with the head of the bed raised) and then contact your local (family) doctor.
When talking with your doctor, you need to clarify which medications you need to take if a hypertensive crisis develops, clearly write down their names, dosage and time sequence (algorithm) for taking them, and also check with your doctor for what manifestations of the disease you need to urgently call an ambulance.
All patients with hypertension need to create an individual mini-first aid kit for a hypertensive crisis and carry it with them at all times, since a hypertensive crisis can develop at any time and anywhere.
FIRST AID for acute heart failure
Acute heart failure (AHF) is a severe pathological condition that develops in patients with various heart diseases and hypertension. This is one of the most common reasons for calling an ambulance and hospitalization of patients, as well as mortality in our country and around the world.
The main manifestations (symptoms) of acute heart failure are:
• heavy, frequent (more than 24 per minute) noisy breathing - shortness of breath, sometimes reaching the level of suffocation, with predominant difficulty in inhaling and a clear increase in shortness of breath and cough in a horizontal position. A sitting position or a lying position with the head of the head raised up alleviates the patient's condition;
• often when breathing, wet, squelching wheezing/sounds, interrupted by coughing, become audible; in the terminal stage, breathing takes on a bubbling character with the appearance of foam at the patient’s mouth;
• characteristic sitting posture of the patient, resting his straight arms on his knees or on the seat (to facilitate breathing)
Acute heart failure can develop very quickly and lead to the death of the patient within 30-60 minutes. In most cases, 6-12 or more hours pass from the first clinical signs to severe manifestations of AHF, but without medical care, the vast majority of patients with AHF die.
Algorithm of emergency actions for acute heart failure
(advice to the patient) – a reminder for the patient
When the above symptoms of AHF appear in patients with hypertension or heart disease (but not the lungs or bronchi), it is necessary:
• call an ambulance
• give the patient a sitting position, preferably in a chair with armrests on which he can lean and engage the intercostal muscles in the act of breathing
• provide physical and psycho-emotional peace and fresh air by ventilating the room
• place your feet in a large container (basin, tank, bucket, etc.) with hot water
• in extremely severe cases, tourniquets are applied to the legs in the groin area, compressing the superficial veins, but not the deep arteries, which reduces blood flow to the heart and thereby facilitates its work
If the patient or the person providing first aid has experience in the use of nitroglycerin, it is prescribed in a dose of 0.4 (0.5) mg (inhalation into the oral cavity is carried out under the root of the tongue, the tablet/capsule is placed under the tongue, the capsule must first be bitten, do not swallow). If the patient’s well-being improves after using nitroglycerin, it is reapplied every 10-15 minutes until the arrival of the emergency medical team. If there is no improvement in the patient’s well-being after the next dose of nitroglycerin, it is no longer used.
Attention! A patient with AHF must exclude all physical activity; it is strictly forbidden to walk, smoke, drink water and take liquid food until special permission from the doctor; Nitroglycerin should not be taken if blood pressure is less than 100 mm Hg. with severe headache, dizziness, acute impairment of vision, speech or coordination of movements.
All patients with hypertension or heart disease with shortness of breath and swelling in the legs should discuss with their doctor what medications should be taken if AHF develops, clearly write down their names, dosage and time sequence (algorithm) for taking them, and also check with the doctor for which manifestations of the disease, it is necessary to urgently call an ambulance.
Each such patient needs to create an individual first aid kit for AHF and constantly have it with him.
FIRST AID for sudden death (advice to eyewitnesses)
Most often, sudden death occurs due to cardiac arrest.
activities.
The main signs (symptoms) of sudden death:
• Sudden loss of consciousness, often accompanied by agonal movements (a standing or sitting person falls, convulsive muscle tension, involuntary urination and defecation are often observed; a lying person sometimes makes a convulsive attempt to sit up or turn on his side)
• Sudden complete cessation of breathing, often after a short period (5-10 seconds) of agonal pseudobreathing: the patient makes wheezing and/or gurgling sounds, sometimes similar to a convulsive attempt to say something.
Algorithm for urgent actions of eyewitnesses to the sudden death of a person
• If a person suddenly loses consciousness, immediately call an ambulance team (if there are other people nearby, they call an ambulance). Next, shake the patient by the shoulder and ask loudly, “What’s wrong with you?” If there is no response, active patting is performed on the patient’s cheeks; if there is no reaction, immediately begin closed cardiac massage.
• The patient is placed on a hard, flat surface (floor, ground, flat hard area and similar places, but not on a sofa, bed, mattress and other soft surfaces), and the front part of the chest is freed from clothing. Determine the location of the hands on the patient’s chest as indicated in the figure. One palm is placed in the place indicated in the figure, and the palm of the second hand is placed on top of the first in exact accordance with the image of the hands in the figure.
Rice. Illustration of the technique of closed cardiac massage
• With straight arms (not bent at the elbows), vigorous rhythmic compression of the victim’s chest is performed to a depth of 5 cm with a frequency of 100 compressions on the chest per minute
• When signs of life appear (any reactions, facial expressions, movements or sounds made by the patient), cardiac massage must be stopped. If these signs of life disappear, heart massage must be resumed. Stops of cardiac massage should be minimal - no more than 5-10 seconds. When signs of life resume, the heart massage stops, and the patient is provided with warmth and peace. If there are no signs of life, cardiac massage continues until the arrival of an emergency medical team.
If the first aid provider has special training and experience in performing cardiopulmonary resuscitation, he can perform artificial ventilation in parallel with closed cardiac massage. In the absence of special training, artificial ventilation of the lungs and determination of the pulse in the carotid artery should not be performed on the patient, since special scientific studies have shown that such procedures in inexperienced hands lead to an unacceptable loss of time and sharply reduce the frequency of revival of patients with sudden cardiac arrest.
remember, that
- emergency medical care only called in the first 10 minutes from the onset of a heart attack or stroke allows full use of modern highly effective methods of inpatient treatment and many times reducing mortality from these diseases
- acetylsalicylic acid (aspirin) and nitroglycerin taken in the first minutes can prevent the development of myocardial infarction and significantly reduce the risk of death from it
- state of alcohol intoxication is not a reasonable basis for delaying calling an ambulance in the event of a heart attack and acute cerebrovascular accident - about 30% of people who suddenly (within an hour from the onset of symptoms) died at home were intoxicated.
- closed cardiac massage performed in the first 60-120 seconds after sudden cardiac arrest allows up to 50% of patients to be brought back to life.
Print Email
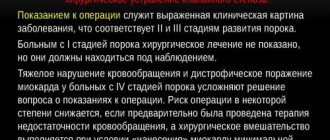
Classification of hypertensive crisis
Depending on the speed of development of the attack, there are:
- Type 1 crisis
- a sharp rise in systolic pressure and a decrease in the indicator with medical help (rapid course), throbbing headache, agitation, irritability, fever, sweating, tachycardia. - Type 2 attack
- a simultaneous increase in upper and lower blood pressure, slow development (from two days or more), decreased vision, hearing, drowsiness, lethargy, symptoms are difficult to eliminate even in a hospital setting. One of the causes of hemodynamic disturbances with subsequent complications.
The presence of complications after a hypertensive crisis allows us to determine whether the process is complicated or uncomplicated. In the first case, manifestations are observed either from the heart (cardiac crisis) and can result in myocardial infarction, or from the brain (cerebral), provoking a stroke.
The forms are:
- Hypokinetic
(decreased cardiac output). Lasts up to several days. It is characterized by drowsiness, loss of strength, decreased vision, and compressive pain in the heart area. - Hyperkinetic
(opposite to the hypokinetic form - increased release). It is characterized by an acute onset, sharp pain in the temporal region, dizziness, decreased vision, agitation, and trembling in the body. Duration - from a couple of minutes to three hours. - Eukinetic
(with normal release dynamics, peripheral blood circulation increases).
Determining the form of the attack is necessary to select further therapy and prognosis.
Consequences
A hypertensive crisis cannot be called a simple sudden sharp increase in blood pressure, accompanied by a headache. GC has a risk of developing many complications from most organs and even systems.
- Disorders of the central nervous system, manifested in confusion or coma (encephalopathy).
- Acute heart failure.
- Brain hemorrhage.
- Pulmonary edema (which results from sudden left ventricular failure).
- Aneurysm.
- Angina pectoris.
- Myocardial infarction.
- Eclampsia, which occurs during pregnancy.
Symptoms of hypertensive crisis
This condition can be assumed based on the following symptoms;
- a sharp increase in blood pressure (depending on the person’s condition, the presence of complications and concomitant diseases);
- tachycardia;
- shooting pain in the occipital region of a pressing, squeezing or bursting nature; often accompanied by a sensation of pulsation;
- dizziness;
- unsteady gait;
- nausea, vomiting;
- dyspnea.
In case of complications or lack of first aid, fainting and even coma are possible.
In children
In children, crises develop with secondary arterial hypertension against the background of glomerulonephritis , coarctation of the aorta , pheochromocytoma , intracranial hypertension , Itsenko-Cushing's disease , adrenal cortex dysfunction, meningitis , polyarteritis nodosa , traumatic brain injury .
During a crisis in children, systolic pressure rises above 150 mmHg. Art., and diastolic is more than 95. In most cases, children experience severe headache lasting several hours or days, nausea , sweating , vomiting . Symptoms such as dizziness , hand tremors , ringing, darkening in the eyes indicate damage to the central nervous system.
To stop the crisis it is important:
- create a calm environment for the child;
- give a sedative;
- use antihypertensive drugs.
Antihypertensive drugs are used in children when repeated vomiting, cardiac dysfunction, disorientation and convulsions occur. Also, as in adults, groups of antihypertensive drugs are used: beta-blockers ( atenolol , esmolol , propranolol ), vasodilators ( sodium nitroprusside ), diuretics ( furosemide ), calcium channel blockers ( nifedipine ), α-blockers ( prazosin ). In case of a crisis that occurs with cardiac symptoms and damage to the central nervous system, the use of nifedipine ( Corinfar ) at a rate of 0.25 mg/kg is effective. The effect appears at the 6th minute and reaches its maximum after an hour.
In children, a crisis often occurs as a sympathoadrenal paroxysm (accompanied by autonomic symptoms). In case of sympathoadrenal crisis, tranquilizers ( Seduxen , Relanium , Diazepam ), an antipsychotic ( Sonapax ) or a combination of a tranquilizer and an antipsychotic ( Seduxen + Sonapax ), as well as Pirroxan ( an alpha-blocker ) and propronalol ( a beta-blocker ) are prescribed.
A rapid increase in diastolic pressure is accompanied by a risk of developing encephalopathy . In this case, it is important to eliminate increased peripheral resistance and brain symptoms (convulsions, agitation). In this situation, vasodilators ( nitroprusside ), beta blockers ( labetalol ), and sometimes ganglion blockers ( pentamine ) are prescribed. For cerebral edema, Lasix . For convulsive forms, emergency care includes intravenous administration of Diazepam and intravenous drip administration of magnesium sulfate .
Diagnosis of hypertensive crisis
After providing first aid for a hypertensive crisis, the heart rate is checked, a medical history is taken, tests are prescribed, hormones are determined, Holter monitoring is performed (a study of blood pressure fluctuations over the course of a day), an ECG, etc.
Concomitant diseases can complicate the diagnosis (additional examination by endocrinological, nephrological, and neurological specialists is possible).
Based on the results obtained, a patient management regimen is prescribed.
First aid
Understanding what a hypertensive crisis is, you need to know how to properly provide first aid to a person with the development of a severe, life-threatening condition. First of all, if there is a sharp jump in blood pressure, you need to urgently call an ambulance team. But before the arrival of specialists, it is necessary to try to stabilize the patient’s condition in order to minimize the risks of dangerous consequences.
It is necessary to reduce blood pressure using medications. It should be remembered that it is necessary to lower blood pressure gradually when a hypertensive crisis develops. You should also take a sedative (valerian or corvalol) to relieve anxiety.
It is important that the patient is in a sitting position that is as comfortable as possible. It is imperative to ensure the supply of fresh air. A cold compress should be applied to the patient's forehead. Additionally, you can make hot foot baths with a water temperature of 40°C or apply mustard plasters to your calves.
With the development of a complicated hypertensive crisis, treatment is possible only in intensive care conditions. Patients are kept in the intensive care ward until their condition is completely stabilized. After this treatment, a certain period of time continues in the hospital therapeutic department.
Treatment of hypertensive crisis
Therapy for a hypertensive crisis includes non-drug treatment methods and drug assistance.
First aid
When recording blood pressure readings that are different from the norm and accompanying signs, it is necessary to provide first aid: lay the person horizontally, turn the head to the side, unbutton the top buttons on the clothes and free the neck, ensure a flow of fresh air, call an ambulance.
You can reduce blood pressure with medications prescribed by your doctor in an individual case.
Non-drug treatment
Therapy begins with changing the patient's lifestyle. Rehabilitation consists of eliminating the causes of hypertensive crisis. The patient is advised to take a vacation, visit a psychologist, change his diet, eliminate bad habits, reduce or add gentle physical activity, etc.
In a hospital, a patient may be prescribed a course of physiotherapy, massage and exercise therapy, or sanatorium-resort treatment.
Drug treatment
Drug treatment, selected individually by a doctor, is aimed at restoring heart rhythm and functions of the cardiovascular system.
The following are used as symptomatic therapy:
- diuretics;
- angiotensin-converting enzyme inhibitors;
- β-blockers;
- calcium channel blockers;
- sedatives.
It is necessary to take medications gradually under the supervision of a doctor to avoid a sharp increase or decrease in blood pressure.
Other treatments
The patient can undergo rehabilitation after a hypertensive crisis in the absence of contraindications: sessions of vitamin therapy, acupuncture, balneotherapy, a course of relaxation, air and sun baths, electrosleep, swimming pool, etc.
Causes
The cause may be various factors. GK usually develops if the patient has arterial hypertension of any origin (hypertension or symptomatic manifestations of hypertension). In addition, HA can often occur with abrupt withdrawal of drugs that lower blood pressure (hypotensive medications). This condition is also called “withdrawal syndrome.”
External reasons include:
- stress;
- weather changes;
- excessive consumption of table salt;
- excessive physical activity;
- excessive alcohol consumption;
- hypokalemia.
Prevention of hypertensive crisis
This is a dangerous condition that can be fatal. It is important to start treatment in a timely manner, to strive to prevent further progression of the disease that caused a sharp increase in blood pressure, following simple recommendations:
- control blood pressure;
- normalize nutrition (follow a regimen, diet);
- maintain normal weight;
- eliminate heavy physical and emotional stress;
- eliminate harmful addictions;
- be examined by a doctor.
During pregnancy
Hypertension during pregnancy is a cause of premature birth, eclampsia , fetal death, and is also associated with maternal deaths. Prevention of preeclampsia (hypertension in combination with proteinuria) is the addition of calcium salts to the diet, resting the pregnant woman lying on her left side, since in this position the pressure decreases and the uteroplacental blood flow increases. Pregnant women with preeclampsia are at risk of thromboembolic complications, and therefore mobility is recommended rather than staying in bed and wearing elastic stockings.
Pregnant women with blood pressure above 140/90 mm Hg. Art. are hospitalized to monitor the woman and fetus. Indications for urgent hospitalization are a state of hypertensive crisis , the addition of preeclampsia , impaired cerebral circulation and renal function, heart failure , and progression of changes in the fundus. If the pressure is above 160/110, the issue of emergency delivery is decided. Emergency delivery is undertaken when the pressure is above 180/110, which does not decrease even in the presence of eclamptic coma .
To reduce blood pressure, Nifedipine (5-10 mg sublingually or orally, if necessary, the drug is taken again after 30 minutes). Nitroglycerin intravenous drip and intravenous administration of labetolol . In severe cases, Pentamin (ganglionic blocker) is used intravenously, which is administered very carefully. It must be remembered that a sharp decrease in pressure leads to a deterioration in uteroplacental circulation and acute kidney damage. To prevent seizures, magnesium sulfate intravenously as a bolus, then slow infusions are continued until the magnesium level is 4.8-9.6 mg. Angiotensin II receptor blockers (ARBs) and ACE inhibitors, which inhibit fetal renal function and cause polyhydramnios in the 2nd and 3rd trimester, are contraindicated for pregnant women. After childbirth, while breastfeeding, it is allowed to take Nifedipine , Propranolol , Spironolactone , Verapamil , Diltiazem , Captopril , Hydrochlorothiazide and Enalapril .
Diet
Diet 10th table
- Efficacy: therapeutic effect after 1 month
- Timing: constantly
- Cost of products: 1700-1850 rubles. in Week
Diet for hypertension
- Efficacy: therapeutic effect after 21 days
- Timing: constantly
- Cost of products: 1600-1700 rubles. in Week
Proper nutrition for hypertension, along with drug treatment, can serve as a preventive measure for the development of crises. Patients are advised to eat a nutritious diet with limited salt, refractory fats and foods rich in cholesterol .
- Salt can be consumed no more than 5 g per day.
- Alcohol, strong tea and coffee, which stimulate the central nervous system, are limited/excluded.
- Otherwise, pickles, spicy snacks, fatty foods, fatty meats, and rich broths are strictly limited.
- If you are overweight, limit flour products, sugar, cereal products, honey, grapes, raisins, and jam.
- Low fat dairy products.
- Whole grain products.
- Lean meat and poultry (boiled or baked).
- Vegetable side dishes, vegetable salads, vinaigrettes, seaweed.
Great importance is attached to the content of potassium and magnesium in products. Consumption of potassium and magnesium has a beneficial effect on the course of hypertension, the condition of blood vessels and the heart. Potassium is rich in baked potatoes, bananas, currants, tomatoes, pumpkin, carrots, cabbage, zucchini, cucumbers, beets, melons, beans, oranges, figs, raisins, dried apricots, and nuts. Magnesium is found in seaweed, rice, buckwheat, bran, bananas, rolled oats and nuts. The diet must contain foods containing polyunsaturated fatty acids: fatty sea fish, fish oil, seeds, nuts and vegetable oils (linseed/rapeseed/olive).