Iron deficiency anemia IDA is a hypochromic microcytic anemia that develops as a result of an absolute deficiency of iron in the body.
In addition to anemic syndrome, it is characterized by dysfunction of the skin, its appendages and mucous membranes - sideropenic syndrome.
IDA is the last stage of iron deficiency; Before the onset of anemia, often with detailed questioning and examination of the patient, manifestations of sideropenia can be detected, which will allow timely identification of the cause of iron deficiency and prevent the development of IDA.
Epidemiology
IDA was first described by the German physician J. Lange in 1554, and drugs for its treatment were first used by T. Sydenham in the 17th century. Anemia that develops as a result of iron deficiency in the body is the most widespread in clinical practice. According to WHO, about 2.5 billion people on Earth have hidden iron deficiency and 1 billion people suffer from IDA.
In women it is observed 2–5 times more often than in men; children are in 2nd place in frequency of occurrence.
The influence of IDA on the increase in the incidence of maternal and child mortality has been reliably proven. IDA occurs in 12–13% of children aged 6 months and older. up to 2 years. In developing countries, this figure is much higher: in India and African countries it reaches 72–76%. In developed countries of Europe and North America, IDA is detected in 7.5–11% of all women of childbearing age, and 20–25% have hidden tissue iron deficiency. The frequency of IDA is significantly higher in the countries of Asia, Africa and Latin America, where it reaches epidemic levels and amounts to 45–60%. Of all anemias encountered in clinical practice, about 80% are iron deficiency. In the Russian Federation, there is no information on the frequency of IDA, however, according to our data, in Moscow its frequency is 30–35% among women of childbearing age, and hidden iron deficiency is up to 60%.
Stages of iron deficiency anemia
Laboratory examination allows you to determine the stage of iron deficiency anemia.
Stage 1 is characterized by decreased iron in the bone marrow; hemoglobin and serum iron remain within normal limits, but ferritin levels fall below 20 ng/ml. A compensatory increase in iron absorption leads to an increase in the iron-binding capacity of the serum.
During stage 2 , erythropoiesis is impaired and serum iron concentrations fall below 9 µmol/L. There is an increase in the concentration of the transferrin receptor.
At stage 3 , anemia is observed with normal erythrocyte indices and no changes on the smear.
At stage 4, microcytosis and hypochromia develop.
At stage 5 , iron deficiency leads to disruption of tissue function, and symptoms and complaints develop.
Development of anemia
Over time, iron deficiency progresses, flows latently for many years, and then, after complete depletion of iron stores in the depot, IDA develops. The main mechanism for the development of anemia is a violation of hemoglobin formation in erythrokaryocytes of the bone marrow. The pathology of erythropoiesis in iron deficiency is based on a violation of heme synthesis, as a result of which the hemoglobinization of erythronormoblasts is delayed compared to the process of reverse development of nuclear structures. Since hemoglobin synthesis suffers to a greater extent due to iron deficiency than the formation of red blood cells, IDA, with a relatively moderate decrease in the number of red blood cells, is characterized by a more pronounced drop in the hemoglobin content in them, which is manifested by hypochromia of red blood cells and the development of hypochromic microcytic anemia.
The second pathological mechanism that occurs under conditions of iron deficiency is a decrease in the formation of other important proteins involved in the accumulation and transport of oxygen. The myoglobin content in striated muscles decreases. Violation of the formation of cytochromes and catalases leads to inhibition of the energy metabolism of all cells of the body, while rapidly dividing tissues (skin and mucous membranes) are mainly affected.
Depending on the causes of iron deficiency, five groups of IDA are distinguished:
1) chronic posthemorrhagic IDA;
2) IDA associated with impaired absorption and intake of iron from food;
3) IDA associated with insufficient initial levels of iron in the body (more often in children);
4) IDA, caused by an increase in the body's need for iron (without blood loss);
5) IDA associated with impaired iron transport.
Symptoms of anemia include:
- muscle weakness not corresponding to the degree of anemia;
- perversion of taste, in the form of a desire to eat inedible substances (chalk, coal, clay), raw foods, cereals, dough, raw minced meat), as well as an addiction to unusual odors (kerosene, fuel oil, gasoline, acetone, shoe polish, naphthalene, exhaust gases) cars);
- hair loss and dry skin with the formation of cracks, especially often in the corners of the mouth (angular stomatitis);
- changes in nails: fragility, appearance of striations, concavity (koilonychia);
- soreness and focal redness of the tongue mucosa with atrophy of the papillae (“geographic tongue”);
- dysphagia, characterized by difficulty swallowing dry food and the development of painful spasms of the esophagus (Plummer-Wilson syndrome);
- dysuric disorders (urinary incontinence, nocturnal enuresis).
Publications in the media
Iron deficiency anemia (IDA) is a hypochromic microcytic hyporegenerative (in children hyperregenerative) anemia that occurs as a result of an absolute decrease in iron resources in the body (usually due to chronic blood loss or insufficient supply of iron from the outside). When formulating a diagnosis, it is necessary to indicate the etiology of IDA.
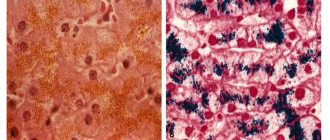
Iron metabolism • The total amount of iron in the body of an adult (male weighing 70 kg) is 4–5 g • The main amount of iron in the body is part of heme (Hb, myoglobin, cytochromes). Some iron is stored in the form of ferritin (in hepatocytes, bone marrow and spleen macrophages) and hemosiderin (in von Kupffer cells and bone marrow macrophages). A certain amount is in a labile state due to transferrin. Most of the iron required for heme synthesis is released from destroyed red blood cells, and only 5% of the iron for erythropoiesis comes from outside • Sources of iron •• Dietary iron accumulates in the epithelial cells of the small intestinal mucosa. From here, transferrin transports iron to the red bone marrow and liver. Iron enters the erythroblasts, and free transferrin is returned to the plasma •• When red blood cells are destroyed in the spleen, liver and bone marrow, the iron released from heme is transported by transferrin to the bone marrow; part of the iron is included in the composition of ferritin and hemosiderin (the so-called reserve iron) • Iron is excreted during desquamation of the epithelium of the skin and mucous membranes; with feces.
Frequency. IDA is observed in 10–30% of the adult population. The most common form of anemia (80–95%). IDA occurs much more often in women than in men. According to various estimates, up to 20% of women suffer from IDA.
Etiology • Acute and chronic blood loss (for example, during gastrointestinal or uterine bleeding) • Nutritional factors - insufficient intake of iron into the body • Impaired absorption of iron in the gastrointestinal tract •• Resection of the stomach and/or intestines •• Hypoacid (anacidic) gastritis, gastroduodenitis •• Malabsorption syndrome • Increased body need for iron (for example, in infants, adolescence, pregnancy, helminthic infestations) • Tumors (for example, hypernephroma, bladder cancer) • Other causes (paroxysmal nocturnal hemoglobinuria, pulmonary hemosiderosis) .
Clinical picture • General symptoms (fatigue, weakness, irritability, apathy, pallor of the skin and mucous membranes). Shortness of breath, tachycardia, arterial hypotension, headache, dizziness occur in severe form • Specific symptoms •• Angular stomatitis •• Koilonychia •• Atrophic glossitis •• Dysphagia •• Perversion of appetite (addiction to chalk, lime, clay, coal, tooth powder or ice).
Concomitant pathology • Peptic ulcer of the stomach and duodenum • Neoplasms • Hemorrhoids • Pulmonary hemosiderosis • Helminthic infestation • Juvenile uterine bleeding in girls.
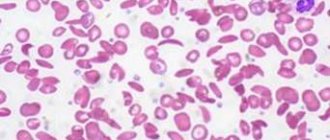
Laboratory tests • The gold standard is staining of bone marrow aspirate to determine iron content, but bone marrow puncture is used only when differential diagnosis is difficult • Determination of decreased serum ferritin concentrations. When using this research method, it is necessary to take into account that ferritin is an acute-phase blood indicator, and therefore diagnostic errors are possible • When examining a peripheral blood smear, hypochromic microcytic anemia, anisocytosis, and poikilocytosis are usually detected in patients. The smear may be normal •• With minor anemia or acute blood loss, the average erythrocyte volume and the average Hb content in erythrocytes may be normal • Hb concentration - less than 120 g/l, but in patients with increased Hb concentration before the disease (smokers, persons with chronic hypoxemia), anemia can develop in the presence of higher Hb levels. Thus, when using standard criteria for anemia, it is necessary to conduct studies aimed at detecting hidden anemia • Drugs that affect test results. Iron-containing foods or multivitamins with added minerals, including iron • Medical conditions that may affect results. Serum ferritin concentrations may increase in acute liver diseases, cirrhosis, lymphogranulomatosis, acute leukemia, fever, acute inflammatory diseases, and hemodialysis.
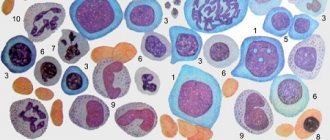
Laboratory signs depend on the stage of iron deficiency • Characteristic signs of iron deficiency - hypochromia and microcytosis - indicate the duration of iron deficiency •• In any form, pale red blood cells of small sizes are found in blood smears (low average erythrocyte volume and average Hb content in erythrocytes), which is reflected on a decrease in the color index •• The number of reticulocytes in adults is reduced (hyporegenerative anemia). In children, reticulocytosis (hyperregenerative anemia) is noted • Specific signs of IDA: •• In the prelatent stage of iron deficiency: low serum ferritin concentration •• In the latent stage: low Fe2+ content in the blood serum, increased TLC, decreased saturation of transferrin with iron • Red bone hyperplasia brain, the presence of micro- and normoblasts, a decrease in the number of sideroblasts (erythrokaryocytes containing iron granules).
Special studies • To establish the cause of iron loss by the body - guaiac test for occult blood in the feces, endoscopic examination of the gastrointestinal tract (fibroesophagogastroduodenoscopy (FEGDS), sigmoidoscopy, colonoscopy), blood coagulation test • If thalassemia is suspected, it is necessary to review previous general blood tests (determining long-term and minor anemia in combination with elliptocytosis), examine the content of HbA2, HbF, family history data • To confirm the violation of iron utilization, it is necessary to conduct a trial course of treatment with iron preparations (orally or parenterally). Trial therapy with iron preparations in a daily dose of 3 mg/kg (calculated for elemental iron) is the best way to diagnose IDA in infants and older children • Determination of the content of free erythrocyte protoporphyrins and iron reserves in the bone marrow is carried out during differential diagnosis.
TREATMENT
Diet • Milk consumption should be limited to 0.5 l/day (for adults). Milk and other dairy products should be avoided completely 2 hours before taking iron-containing medications • Close attention should be paid to the amount of protein and iron-containing foods consumed (meats, legumes, leafy greens, figs, dates) • To reduce the likelihood of constipation in patients receiving replacement therapy with iron preparations; it is recommended to increase the content of plant fiber in the diet.
Drug therapy • Iron sulfate 300 mg 3 times a day orally between meals (provides 180 mg of pure iron per day into the body; taking the drug with meals reduces iron absorption by 50%). With adequate therapy, reticulocytosis is observed in the blood after 7 days; after 2 weeks, the Hb level increases (usually by 0.7–1 g/week). Lack of therapeutic effect (or weak effect) indicates ongoing bleeding, concomitant infection or malignancy, insufficient dose of the drug, or (very rarely) iron malabsorption. Hb concentration reaches normal levels within 2 months of treatment. The drug should be taken for 6 months (but no more) •• If you are intolerant to iron sulfate, you can prescribe either iron gluconate or iron fumarate •• If symptoms of gastrointestinal damage appear, the dose of the drugs should be reduced • Children are advised to take liquid forms of iron-containing drugs in the recommended dose 3 mg/kg/day (calculation for elemental iron) • In severe cases (for example, with malabsorption syndrome), iron preparations (for example, iron [III] hydroxide polyisomaltose, fercoven) are prescribed parenterally. For hypermenorrhea, iron-containing drugs are prescribed 7–10 days before the expected period of menstruation, continued during it and for 7–10 days after its end.
Observation. Monitoring the Hb content in the blood monthly after normalization of its concentration and serum iron concentration.
The course and prognosis are favorable with timely diagnosis of IDA and adequate therapy with iron-containing drugs.
Pregnancy. IDA often develops during pregnancy without dietary correction with iron supplements.
Features in children • Main causes •• Nutritional errors •• Increased need for iron during growth •• In girls of puberty - polymenorrhea • Risk factors for the development of iron deficiency in the first year of life •• Prenatal ••• Prematurity ••• Multiple pregnancy • •• Gestosis in a pregnant woman ••• Anemia in a pregnant woman •• Intranatal ••• Early umbilical cord ligation ••• Premature placental abruption •• Postnatal ••• Hemolytic disease of the newborn ••• Intestinal dysbiosis • Prevention of IDA in the first year of life •• Reception pregnant women taking iron supplements from the 20th week of pregnancy •• Prophylactic administration of iron supplements to children at risk.
Features in the elderly • Approximately 60% of all cases of IDA are observed in patients over 65 years of age • In older people, IDA can lead to exacerbation of coronary artery disease with subsequent development of left ventricular failure.
Prevention • A balanced diet with adequate iron content • Treatment of diseases leading to chronic blood loss • Treatment of anemia in pregnant women • Breastfeeding of children.
ICD-10 • D50 Iron deficiency anemia
Stages of iron deficiency
Currently, there are several stages of iron deficiency:
1. Predisposition to the development of iron deficiency (vegetarianism, adolescence in combination with menstrual irregularities in girls, frequent childbirth, the presence of chronic diseases of the gastrointestinal tract or female reproductive system associated with blood loss).
2. Pre-latent iron deficiency. At this stage there are no laboratory criteria for iron deficiency, however, an increase in the absorption of 59Fe3+ in the gastrointestinal tract can be determined, which can exceed 50% (normally 10-15%).
3. Latent iron deficiency. It is characterized by the development of sideropenic syndrome, a decrease in iron reserves in the body according to laboratory tests.
4. WAITING. The diagnosis is established when the hemoglobin concentration decreases to less than 120 g/l in women and 130 g/l in men.
Forecast
In most cases of iron deficiency anemia, the therapy provided has excellent results. However, the situation is significantly complicated by the frequent presence of a severe primary disease that causes anemia (most often oncological pathology). In addition, the prognosis of patients with iron deficiency anemia is significantly worsened by diseases of the cardiovascular system.
Iron deficiency anemia is rarely fatal, but severe and moderate cases can cause sufficient hypoxia to aggravate chronic lung and heart disease.
In children, iron deficiency can cause reduced growth rate, reduced IQ and reduced learning ability.
Diagnosis of hypochromic anemia
To make a diagnosis, the doctor examines the patient and listens to his complaints. Without fail, the doctor clarifies whether immediate blood relatives suffered from anemia. The next stage of diagnosis is laboratory tests. Be sure to donate blood for analysis to calculate the level of red blood cells and hemoglobin in it.
| Age and gender | Normal hemoglobin level in g/l | Deviations from the norm in g/l | |
| Male | 130-160 | Less than 130 | |
| Female | 120-150 | Less than 120 | |
| Pregnant women | 110-150 | Less than 10 | |
| Children under five years old | Newborns | 145 | Less than 145 |
| 1-14 days | 130 | Less than 130 | |
| 15-28 days | 120 | Less than 120 | |
| 1-5 years | 110 | Less than 110 | |
One red blood cell should contain 0.85-1.15 hemoglobin. Hypochromic anemia is characterized by a decrease in this indicator to less than 0.85.
To clarify the diagnosis, you will need to go through a number of additional diagnostic procedures, which also allow you to find out the cause of anemia:
- Submission of stool to detect hidden blood in it.
- Passing FGDS to examine the mucous membrane of the stomach and duodenum.
- A colonoscopy involves examining the intestines.
- Submission of urine for analysis.
- Ultrasound examination of the kidneys.
- X-ray examination of the lungs.
- All women must see a gynecologist.
- A bone marrow puncture is performed.
- A blood test is performed to determine serum iron levels.
How to treat?
Treatment of hypochromic anemia is based on the causes that caused it. To eliminate clinical anemia, iron supplements and vitamin B12 are used. It should be taken into account that vitamins are not retained in the body and are quickly excreted by the kidneys, so it will not be possible to achieve a lightning-fast effect.
Basic principles of therapy:
- Iron source medications are prescribed for a period of 1 to 1.5 months. This allows you to increase the level of hemoglobin in the blood. Such medicines are: Ferrum Lek, Hemofer, Fenyuls. If drugs for parenteral administration are indicated for the patient, treatment should be carried out in a hospital setting, since injections are associated with a high risk of developing an allergic reaction.
- Cyanocobalamin is prescribed when the patient is diagnosed with vitamin B12 deficiency. The duration of the therapeutic course can range from 30 days to 2 months.
- If folic acid deficiency is detected, oral supplementation will be required. The duration of therapy is a month.
Depending on individual indications, the doctor may prescribe drugs to the patient in different forms of release: tablets, capsules, solution, syrup, etc. Injection of drugs is indicated only if the person has an acute disease of the digestive system, or the condition is extremely serious. In this case, the patient must be hospitalized.
Diet
Treatment of anemia involves following a diet.
Basic rules to follow:
- Every day a person should receive about 130-150 g of animal protein. Moreover, the emphasis should be on beef and veal. Protein is the basis for the synthesis of hemoglobin and red blood cells.
- Fatty foods on the menu should be limited, as they have a negative effect on the process of hematopoiesis.
- To increase the patient's appetite, a variety of dishes should be introduced into his diet. It could be fish, meat, mushrooms.
- The diet should contain foods that are a source of B vitamins - eggs, cottage cheese, yeast, fish. Every day you need to eat at least 100 g of liver.
Products that must be on the menu:
- Liver, meat and fish with a low fat content. Beef is especially beneficial as it is a source of heme iron and vitamins.
- Cottage cheese.
- Mushrooms.
- Eggs.
- Bread.
- Brewer's yeast.
- Pomegranate juice. It can also be diluted in equal proportions with beet juice.
- Peas, lentils and beans.
- Various berries are eaten as a source of vitamin C.
There are also foods that prevent iron from being absorbed in the body. These include: cereals (millet and oatmeal), tea, herbs, whole milk, coffee, fatty foods. They should be excluded from the menu.
Indicative menu for 1 day for a person with hypochromic anemia:
- First meal: soft-boiled egg, millet porridge with apple, pomegranate juice.
- Snack: cottage cheese and rosehip decoction.
- Lunch: vegetable soup, potato zrazy and boiled vegetables, fried liver, berry salad and compote.
- Snack: yeast-based drink, baked beets.
- Dinner: stewed beef ribs, salad with green peas, beans and vegetable oil, rowan juice.
Cooking recipes:
- To prepare millet porridge you will need 0.25 kg of flakes and 0.5 liters of apple juice. The flakes are poured with juice and left to infuse overnight. In the morning, boil the porridge in a saucepan for 10 minutes.
- To prepare baked beets, you need to wash them, grease them with vegetable oil, sprinkle them with salt and bake them in the oven. Baking time is 45 minutes at 175 °C.
- Drink with yeast. Dissolve 10 g of live yeast in 100 ml of water and leave for an hour. After this time, the drink can be drunk.
- Salad with berries: mix raspberries, strawberries and blackberries, add chopped banana and apple, add lemon juice and a teaspoon of honey.
- Rowan juice. Berries in the amount of 100 g are crushed, rowan flowers and mint (10 g) are added to them. Take 0.2 liters of boiling water for 2 tablespoons of the mixture, pour it over the rowan, and let it brew.
Hypochromic anemia - what is it?
Hypochromic anemia is not one disease. This term combines several types of anemia. However, each of them is characterized by a decrease in the level of hemoglobin in the blood. Hemoglobin is a protein that contains iron. Hemoglobin is transported by red blood cells and is responsible for gas exchange in the body. If the level of hemoglobin in the blood falls, this leads to the development of hypoxia of organs and tissues. As a result, they are unable to function normally, which seriously affects human health.
If you turn to the Greek language, you can find out that anemia is translated as anemia. This concept perfectly reflects the essence of this violation. Anemia can accompany a wide variety of diseases that are in one way or another related to the hematopoietic system.
In addition to the fact that with hyperchromia, the level of hemoglobin in the blood decreases, the number of red blood cells in it decreases. People suffering from anemia are more susceptible to attacks from various viruses and bacteria. It has been established that patients with anemia are 2 times more likely to consult doctors about intestinal and respiratory viral infections.
Hyperchromic anemia is characterized by a decrease in the color index of the blood. The red blood cells change from their normal biconcave disc shape to a ring shape. In the middle of these red blood cells, a light circle appears, which is bordered by a dark ring.
Anemia is a common disorder not only among adults, but also among children. Immediately after birth, the child has a certain supply of iron, which he received from the mother. If these reserves are not replenished, the baby will develop anemia.