Heart attacks, cardiac arrest and strokes are all serious conditions related to the heart, but too often people use the terms interchangeably without understanding the differences between the three. While the disorders are all (usually) related to the heart, they have different causes and symptoms, and it's important to know the characteristics of each so you can better identify and treat problems if they occur in your loved ones, or even yourself.
What is the difference between the three conditions?
Heart attack
It is a circulatory problem that occurs when arteries become blocked and the normal flow of oxygen through the blood to the chambers of the heart is prevented. The attack occurs when the coronary arteries, which are responsible for transporting blood to the heart, become smaller due to the accumulation of fatty substances, calcium and protein in them.
Over time, these deposits form a plaque that hardens on the outside. This can lead to rupture, causing blood clots to form around them. When these blood clots block the coronary arteries completely, blood cannot reach the heart, which ends up starving for oxygen. When this happens, the muscle cells in the heart begin to die and can become damaged, which is what constitutes a heart attack.
Causes of heart attack and stroke
Causes of development of ischemic cerebral infarction:
- increased blood viscosity;
- blood clots;
- decreased cerebral blood flow due to diseases of the heart, vascular system, and blood;
- age;
- physical inactivity;
- bad habits;
- pathology of the vertebral and carotid arteries.
Symptoms of ischemic stroke increase gradually. Over time, a cyst forms at the site of the area affected by ischemic cerebral infarction.
The main causes of hemorrhagic stroke:
- high blood pressure (hypertension);
- microangiopathy (pathological condition of the vessels responsible for metabolism).
Stroke
Stroke, also known as CVA, is actually a brain disorder that is often (but not always) caused by heart problems. This occurs when blood flow to the brain is reduced to the point where cells in the brain begin to die. There are two main types of stroke:
Ischemic: Resulting from blockages in the arteries, resulting in a lack of blood flow to the brain and the death of brain cells. This type of stroke involves the heart and circulatory system and is often confused with a heart attack or cardiac arrest.
Hemorrhagic: Caused by bleeding, usually caused by a rupture of an artery in the brain itself. They can sometimes be associated with traumatic injuries to the head, although the impact may occur long after the initial incident.
What are the symptoms of each condition?
All of these conditions can develop very suddenly, but there are often a number of indicators that people can use to help identify a developing problem. Some of the symptoms may be shared between the two conditions, but there are some differences that can help you tell them apart:
Diagnosis of stroke
Diagnosis of a stroke is quite complex, because to identify the cause and assess brain damage, and therefore the consequences of a stroke, the doctor will need a large amount of data.
To visualize the condition of the brain vessels, CT or MRI can be used, depending on the situation. A fairly informative study on the state of blood flow will be angiography - an X-ray examination using a contrast agent injected into the vessels.
In addition, the doctor may prescribe blood and urine tests; test for glucose and cholesterol levels; conduct an ultrasound examination.
Heart Attack Symptoms
Symptoms that indicate a heart attack may come and go, but the condition may also worsen over time. They are also likely to be more acute during physical activity.
- Chest pain: Also known as angina. Sufferers often describe a feeling of heaviness or tightness in the chest. This feeling often comes and goes and can easily be confused with indigestion.
- Pain and numbness in other areas of the body: Feelings of pain or discomfort in the arms, neck, or jaw are common indicators of cardiovascular disease. The left side of the body is more likely to experience more pain than the right side.
- Unexplained difficulty breathing, hoarseness, and extreme weakness.
- Fast or irregular pulse or heartbeat.
- Dizziness, nausea and vomiting.
- Intense and often unexplained feelings of anxiety.
Symptoms of diseases
Ischemic stroke is characterized by dizziness, dark vision, numbness in the limbs - a feeling of numbness appears in the arm or leg, in some cases symptoms appear on one half of the body. The patient's speech becomes incoherent or he cannot speak at all for some time. The face and lips may become distorted - facial paralysis develops. This occurs due to damage to a part of the brain and its failure to perform its functions. With timely assistance, functionality is restored - healthy areas of the brain begin to be responsible for speech, muscle function and other functions.
Hemorrhagic stroke is characterized by an acute course of the disease, the appearance of the following symptoms:
- a sharp decrease in visual acuity;
- loss of consciousness;
- photophobia;
- tinnitus;
- headache;
- vomiting, severe nausea;
- redness of the face and body;
- unsteady gait;
- convulsions;
- paralysis of one side of the face;
- paralysis of one side of the body;
- impaired coordination of movements;
- the patient speaks poorly, gets confused in words;
- coma.
It is very important to provide first aid for a brain stroke as early as possible. The patient is admitted to the hospital, diagnostics are carried out, seizures are eliminated, brain swelling is relieved, and the patient’s condition is stabilized. On the basis of the Yusupov Hospital there is a hospital, an intensive care unit, and a rehabilitation unit for patients after serious illnesses. If necessary, resuscitation measures will be carried out at the Yusupov Hospital and the seriously ill patient will be cared for.
Symptoms of cardiac arrest
In more than half of cases, cardiac arrest occurs without symptoms, as a “sudden event.” However, some patients experience a range of symptoms in anticipation of the problem. These include:
- Rapid heartbeat or extreme heartbeat.
- Feelings of dizziness and disorientation.
- Loss of breath and chest pain.
Although these indicators can predict cardiac arrest, most people will be alerted to it by the most severe symptoms, such as sudden weakness or loss of consciousness. In most cases, it is therefore very difficult to distinguish a stroke from a heart attack in advance.
First aid
Both pathologies are extremely serious. If a pain attack behind the sternum of a squeezing or squeezing nature persists or increases, accompanied by weakness, cold sweat, severe shortness of breath, or if speech disturbances or impaired motor function occur, it is necessary to call an ambulance as quickly as possible. In this situation, delay is like death. The sooner specialized qualified care is started, the higher the survival rate.
The gold standard in the treatment of acute coronary pathology is emergency surgery aimed at restoring blood flow in the shortest possible time. Currently, all large hospitals are equipped with appropriate equipment.
To prevent a heart attack or stroke, you must adhere to several rules: do not smoke, walk 10,000 steps per day, adhere to a balanced diet, maintain a drinking regime (1–1.5 liters of clean still water per day), do not abuse alcohol, control your weight and, accordingly, , waist circumference (for men no more than 94 cm, for women no more than 80 cm), monitor blood pressure levels, check blood glucose and cholesterol levels. You are also required to undergo an annual medical examination. If you already have cardiac pathology, take prescribed medications regularly. If your health suddenly deteriorates, you should immediately call an ambulance.
Symptoms of a stroke
Many of the early symptoms of a stroke are neurological and may begin to appear in the weeks and months before the attack. Symptoms to watch out for include:
- Severe headaches that may be accompanied by a feeling of dizziness.
- Confusion, forgetfulness and memory loss. Inability to speak clearly or remember anything from the past.
- Blurred vision in one or both eyes and slurred speech.
- Coordination problems leading to problems walking or lifting objects.
- Nausea, illness and excessive sweating.
- Partial or complete loss of feeling and function in the arms, legs and mouth. It usually affects one side of your body.
What is commonly confused between these disorders?
It should be noted that during a heart attack the heart continues to beat, but during cardiac arrest it stops altogether (or the power of the beating is significantly reduced) due to an electrical malfunction. Those who have previously had a heart attack are at greater risk of cardiac arrest.
Doctor
A heart attack is also more likely to occur as a result of symptoms gradually developing and worsening over time (although sometimes, people can have a heart attack despite having no symptoms at all - a condition known as a "silent" heart attack).
Stroke symptoms, meanwhile, vary and usually affect the sufferer's head or motor skills. Since the causes of stroke can be attributed to the heart's inability to pump enough blood to the brain, it actually occurs as a result of sudden cardiac arrest (which is actually one of the main causes of stroke).
What should you do?
You do not need to live in fear because of any disorder, but you should always contact your doctor if you have any concerns that you have such symptoms. Heart attacks and strokes in particular do often provide notice of an upcoming event, and treatment can prevent disaster.
The best ways to ensure that you do not have such problems are to live a healthy lifestyle, avoid bad habits, eat well and exercise regularly. Also, see your doctor for regular checkups, especially if you have any symptoms that may be related to these conditions.
Ischemic stroke (cerebral infarction) - symptoms and treatment
General events
When treating ischemic stroke, it is customary not to reduce blood pressure quickly if it is high, especially in the first days of the disease.
Low blood pressure should be increased - this is done by doctors; do not give the patient any medications on your own. Uncontrollable, severe vomiting is a common problem in the period immediately after a stroke, especially when the basilar artery is affected. This creates problems in the patient's nutrition. If vomiting does not stop, or there is dysphagia, then a feeding tube is inserted. The lack of electrolytes is compensated for by infusion therapy. The airway should be closely monitored.
Thrombolytic therapy
Thrombolytic therapy is the only therapy for acute ischemic stroke whose effectiveness has been proven in large studies.
No more than 4.5 hours should pass from the onset of the first symptoms of a stroke to the administration of a thrombolytic, so prompt hospitalization is important.
Vascular occlusion occurs in the arterial or venous bed. Thrombotic medications dissolve the clot, but the drug must be delivered to the thrombotic area.
Thrombolytic agents first appeared in the 1940s. The active development of drugs in this group has led to the fact that there are currently five generations of thrombolytics:
- The first thrombolytics are natural substances that convert plasmagen into plasmin, thereby causing active bleeding. These ingredients are isolated from the blood. This group of drugs is rarely used, as severe bleeding is possible. This generation includes: Fibrinolysin, Streptokinase, Urokinase, Streptodecase, Thromboflux.
- The second generation are substances obtained based on the achievements of genetic engineering using bacteria. This generation of drugs has been well studied and has virtually no side effects. Act directly on blood clots. This generation includes: Alteplase, Actilyse, Prourokinase, Gemaz. Purolase, Metalise.
- Third generation - these drugs are able to quickly find a blood clot and act on it for a longer period of time. Most effective in the first three hours: Reteplase, Tenecteplase, Lanoteplase, Antistreplase, Antistreptolase.
- Fourth generation - these drugs are in development and are characterized by a rapid and intense effect on the blood clot. Insufficiently studied.
- The fifth generation is a combination of natural and recombinant active substances.
In the recovery phase, when the patient’s condition almost always improves to one degree or another, speech therapy assistance, as well as occupational therapy and exercise therapy, are important.
Infusion therapy
Anticoagulants (heparin and indirect anticoagulants) are prescribed only when the doctor’s instructions will be followed and it is possible to monitor blood clotting [8].
Anticoagulants
Anticoagulants prevent the formation of fibrin threads and thrombus formation, help stop the growth of already formed blood clots, as well as the effect of endogenous fibrinolytic enzymes on blood clots [11].
Anticoagulant treatment can be started only after intracerebral bleeding has been ruled out.
Direct coagulants : heparin and its derivatives, direct thrombin inhibitors, as well as selective inhibitors of factor X (Stewart-Prower Factor - one of the blood clotting factors).
Indirect anticoagulants:
- Vitamin K antagonists: phenindione (Phenilin), warfarin (Warfarex), acenocoumarol (Sincumar);
- Heparin and its derivatives: heparin, antithrombin III, dalteparin (Fragmin), enoxaparin (Anfibra, hemapaxan, Clexane, Enixum), nadroparin (Fraxiparin), parnaparin (Fluxum), sulodexide (Angioflux, Vessel Due F), bemiparin (Cibor);
- Direct thrombin inhibitors: bivalirudin (Angiox), dabigatran etexilate (Pradaxa);
- Selective factor X inhibitors: apixaban (Eliquis), fondaparinux (Arixtra), rivaroxaban (Xarelto).
Antiplatelet agents
The administration of antiplatelet agents improves the passage of fluid in the brain tissue and prevents the development of acute disruption of the blood supply to the brain [6].
Antiplatelet agents prevent platelets from sticking together, thereby preventing the formation of blood clots.
Classification of antiplatelet agents by mechanism of action:
- aspirin, indobufen, trifluse (stop the action of cyclooxygenase-1, COX-1);
- ticlopidine, clopidogrel, prasugrel, ticagrelor, cangrelor (stop the functioning of the ADP receptor P2Y12 on platelet membranes);
- abciximab, monofram, eptifibatide, tirofiban; xymelofiban, orbofiban, sibrafiban, lotrafiban and others (glycoprotein (GP) Iib/IIIa antagonists);
- dipyridamole and triflusal (cAMP phosphodiesterase inhibitors);
- iloprost (adenylate cyclase enhancer);
- ifetroban, sulotroban and others (suppress the TXA2/PGH2 receptor);
- atopaxar, vorapaxar (antagonize the AR receptor (protease activated receptors) of thrombin).
Aspirin is a commonly used drug in this group. If anticoagulants are contraindicated, then antiplatelet agents can be used.
Surgery
Carotid endarterectomy is a prophylactic surgical procedure performed to remove atherosclerotic plaque from the arteria carotis communis (common carotid artery).
When a cerebellar stroke develops with compression of the brain stem, in order to save the patient’s life, a surgical operation is performed to relieve intracranial pressure in the posterior cranial fossa.
Decongestant therapy
There are different and quite opposite opinions regarding the use of corticosteroids for ischemic stroke, but doctors still actively use them to reduce cerebral edema: they prescribe dexamethasone 10 mg intravenously or intramuscularly, then 4 mg intravenously or intramuscularly every 4-6 hours.
Osmotic agents . Mannitol - increases plasma osmolarity, thereby fluid from tissues, including from the brain, moves into the bloodstream, creating a pronounced diuretic effect, and a large amount of fluid is removed from the body. Cancellation can have a rebound effect.
Anticonvulsants
They must be prescribed for the development of ischemic stroke with epileptic seizures.
Rehabilitation after stroke
Rehabilitation measures begin in the early period of the disease and continue after discharge from the hospital. They include not only drug treatment, massage, physical therapy, speech therapy classes, but also require the involvement of other specialists in psychological, social and labor rehabilitation.
Along with the restoration of impaired functions, rehabilitation includes:
- prevention of post-stroke complications;
- prevention of recurrent strokes.
Basic principles of rehabilitation after stroke:
- early start of rehabilitation measures;
- systematicity and duration, which is possible with a well-organized step-by-step construction of rehabilitation;
- inclusion of specialists of various profiles in the rehabilitation process, individualization of rehabilitation programs;
- active participation in the rehabilitation process of the patient himself, his relatives and friends.
The duration of rehabilitation is determined by the timing of restoration of impaired functions. Recovery of motor functions occurs mainly in the first 6 months after a stroke. During this period, intensive motor rehabilitation is most effective. Rehabilitation treatment for patients with aphasia should be longer and carried out during the first 2-3 years after a stroke.
The complexity of rehabilitation consists of using not one, but several methods aimed at overcoming the defect.
For movement disorders, the rehabilitation complex includes:
- methods of kinesiotherapy (passive and active gymnastics, training in walking and self-care skills);
- correction of motor dysfunction using biofeedback and electrical stimulation using feedback;
- methods of overcoming spasticity and treatment of arthropathy.
For speech disorders, the main thing is regular classes with a specialist in the restoration of speech, reading and writing (speech therapist-aphasiologist or neuropsychologist).
The following model of staged rehabilitation after a stroke is most optimal:
Stage 1 - rehabilitation begins in the angioneurological department (or in the regular neurological department of a clinical hospital), where the patient is delivered by ambulance;
Stage 2 - at the end of the acute period (the first 3-4 weeks), the following options for referring patients are possible:
- 1st option - the patient with complete restoration of impaired functions is discharged for outpatient follow-up treatment or transferred to a sanatorium;
- 2nd option - a patient with a pronounced motor deficit, who by the end of the acute period is still unable to move independently or moves with great difficulty, and needs outside help with self-care, is transferred to the rehabilitation department of the hospital where he was taken by ambulance;
- Option 3 - patients with moderate and mild motor defects, who can move independently within the hospital and provide basic self-care, are transferred to a rehabilitation center. Patients who, during their stay in the rehabilitation department of the hospital (2nd option) have learned to walk independently and simply take care of themselves in everyday life, are also transferred to the rehabilitation center.
Stage 3 - outpatient rehabilitation: rehabilitation in special rehabilitation sanatoriums and at home.
Outpatient rehabilitation is carried out on the basis of rehabilitation departments of clinics or recovery rooms or in the form of a “day hospital” at rehabilitation departments of hospitals and rehabilitation centers. In rehabilitation sanatoriums there can be patients who can fully care for themselves and move independently not only indoors, but also outside. For those patients who cannot independently get to a clinic or day hospital, rehabilitation assistance (classes with a physical therapy methodologist and classes on speech restoration) is provided at home, with the obligatory training of relatives.
Contraindications and limitations to active rehabilitation
The following concomitant diseases limit or prevent active motor rehabilitation:
- frequent attacks of angina pectoris;
- heart failure;
- high and poorly controlled blood pressure;
- chronic pulmonary diseases: bronchial asthma with frequent attacks, obstructive bronchitis;
- severe forms of diabetes mellitus;
- cancer;
- acute inflammatory diseases;
- some diseases and pathologies of the musculoskeletal system: severe arthritis and arthrosis, amputated limbs.
Psychoses and severe cognitive impairment (dementia) are limitations for carrying out not only motor, but also speech rehabilitation.
There are limitations for rehabilitation treatment in conventional rehabilitation centers: extremely limited mobility of patients (lack of independent movement and self-care), impaired control of the functions of the pelvic organs, and impaired swallowing. Rehabilitation of such patients, as well as patients with severe cardiac and pulmonary pathologies, is carried out in rehabilitation departments located on the basis of large clinical multidisciplinary hospitals, according to special rehabilitation programs.
First aid for stroke
Having discovered signs of a stroke in a woman, it is necessary to call emergency doctors and provide the patient with first aid:
- lay the victim on the bed, create an elevated position for the head by placing a pillow or blanket;
- increase the flow of fresh air by opening a door or window to the street and turning on ventilation;
- Unfasten the tight collar and belt.
Before the ambulance arrives, blood pressure should be measured and if it increases significantly, give an antihypertensive drug, which the patient takes as planned. You can put a heating pad under your feet. When vomiting occurs, you must turn your head to the side to prevent vomit from entering the upper respiratory tract.
Ambulance doctors will provide first aid. Call by phone, and the neurology clinic will prepare everything necessary for emergency specialized care before the patient arrives at the Yusupov Hospital. Patients with stroke are treated by doctors of the highest category and professors who are leading experts in the field of cerebrovascular disorders. Stroke therapy is carried out according to individual regimens using the most effective drugs.
Characteristics of diseases
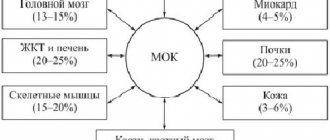
If blood circulation is disrupted in any organ, local or widespread tissue necrosis (necrosis) occurs due to the absence or insufficient supply of nutrients and oxygen.
This process is called a heart attack. Not everyone knows that this pathology affects not only the heart muscle, but also other organs (brain, lung, kidney, intestines). But only changes in the myocardium occur quickly and require urgent hospitalization. Stroke is an acute process of cerebral circulation disorder, which is accompanied by typical neurological symptoms. He can be:
- Ischemic. Occurs in a certain area due to blockage of the lumen of the vessel. Based on its origin, it is divided into thromboembolic, hemodynamic and lacunar. Its second name is cerebral infarction.
- Hemorrhagic. Appears as a result of a violation of the integrity of the vessel wall with subsequent release of blood into the tissue.
A heart attack is a broad concept and can affect many organs. Stroke has several types and causes, but only the brain is affected.
What is more dangerous for humans?
The likelihood of complications and death is high in both cases. But the incidence and survival rate depend on gender. Infarction with damage to the heart muscle in middle age is more common in men; after 50 years, this difference smooths out.
The fact is that in a young woman, a high level of estrogen protects her from the development of atherosclerosis, and during menopause, hormonal levels change. The mortality rate due to myocardial necrosis remains higher in the stronger sex. Stroke occurs less frequently in women, but in them it is more likely to be fatal.
It makes no sense to talk about what is more dangerous: a stroke or a heart attack. The prognosis and outcome of each of these diseases depends on many factors:
- age and gender;
- degree of irreversible damage to organ tissue;
- presence of concomitant diseases;
- speed and accuracy of emergency care.
The probability of death of the patient in the first hours of acute vascular pathology is the same in both cases. But in this sense, my colleagues and I consider a heart attack to be more dangerous. Myocardial necrosis develops very quickly, and doctors simply do not have time to get to the patient. However, after a stroke, it takes much longer to recover and more often leads to severe disability: the prognosis for quality of life is less favorable.
Case from practice
A patient was admitted to the hospital with complaints of weakness, severe chest pain and heaviness in the head.
At the same time, dizziness, shortness of breath, blue discoloration of the nasolabial triangle, high blood pressure, and increased pulse rate were noted. The ECG revealed signs of acute myocardial ischemia in the posterior basal parts of the heart. When taking an EEG, no abnormalities were found; there were no pathological symptoms from the nervous system. A blood test showed an increase in myoglobin, troponin, ALS and AST, and low-density cholesterol levels. Diagnosis: Acute macrofocal myocardial infarction. Hypertension II degree.
Treatment was carried out (oxygen therapy, intravenous nitrates in a dropper, Heparin, beta blockers, diuretics, sedatives). After 3 weeks of intensive therapy, the condition improved, the cardiogram showed positive dynamics, and scar formation was noted. He was discharged under the supervision of a cardiologist at his place of residence. Secondary prevention of the disease is recommended, constant intake of Aspirin, Nitroglycerin when pain occurs, Bisoprolol, Atorvastatin for life, a diet with limited fatty foods.
First signs and symptoms
Before a stroke, drowsiness, headache, numbness of the limbs, fatigue, spots before the eyes, nausea, dizziness, temperature fluctuations, and blood pressure jumps appear. These are the harbingers or first signs of a stroke that appear several hours or days before the disaster. Most often, these symptoms are ignored, or they are attributed to fatigue and overwork.
Symptoms of a stroke themselves are divided into general cerebral and focal. They can be of varying degrees of severity depending on the prevalence of the pathological process.
- General cerebral symptoms: headache, impaired consciousness up to loss of consciousness, stupor, agitation or weakness, disorientation in space and time, sweating, feeling hot, convulsions. Makes you feel sleepy and sometimes chills.
- The focal abnormalities of a stroke depend on which area of the brain is affected. They can be unilateral or bilateral. This group includes disturbances in speech, vision (visual hallucinations), gait, movements up to paralysis, and sensitivity.
Symptoms of ischemic cerebral stroke develop gradually, with focal symptoms predominant.
With a hemorrhagic stroke, the onset is rapid, with a predominance of cerebral symptoms.
There are several stages in the development of a stroke: the acute period (from the moment of the stroke to 3 weeks on average), the recovery period - from 2 weeks to 24 months.