Chemotherapy is widely used to treat cancer. Special drugs prevent the division of cancer cells, but at the same time they also affect other cells in the body. This leads to various side effects, one of which is leukopenia – a decrease in white blood cells.
According to statistics, a decrease in leukocytes in the blood after chemotherapy becomes noticeable approximately 5-8 days after starting to take the drugs. The incidence of this side effect is estimated differently: if, according to some researchers, we can talk about 16% of patients suffering from leukopenia, then according to other scientists, the proportion of people with a reduced level of leukocytes reaches 59% of the total number of those who were prescribed chemotherapy.
Leukocytes or white blood cells protect the body from everything that is genetically foreign to it. They are divided into two groups:
- granulocytes - eosinophils, neutrophils and basophils;
- agranulocytes – monocytes and lymphocytes.
Each cell type has its own clearly defined function.
Eosinophils form antiparasitic immunity. They are also responsible for some hypersensitivity reactions and can be both causative agents of allergic reactions and their inhibitors.
Neutrophils provide the body's defense against fungi and bacteria. Their cytoplasm contains granules that contain proteolytic enzymes that destroy pathogenic microorganisms.
Basophils are involved in allergic reactions and inflammatory processes. Their cytoplasm contains granules with histamine, which, when released, helps to dilate capillaries and lower blood pressure.
Monocytes are the precursors of macrophages. They participate in the phagocytic reaction, capturing and digesting particulate matter.
Lymphocytes are divided into several groups and, depending on their specialization, are capable of producing antibodies, regulating and suppressing the immune response, and fighting viral, tumor and atypical cells.
Why is leukopenia dangerous?
Side effects are common to all types of antitumor treatment, even if it is carried out according to modern standards. Most of the complications, including those associated with suppression of hematopoiesis, such as leuko- and neutropenia, develop delayed, when the patient is no longer in the hospital, but is discharged for outpatient observation.
Leukopenia is a condition characterized by a decrease in the level of leukocytes in the blood.
Leukocytes are white blood cells. One of the varieties of blood cells, along with red blood cells and platelets.
The main function of leukocytes is to protect the body from infections, foreign proteins and foreign bodies that can harm it and upset the balance of biochemical reactions.
The content of leukocytes in the blood is not constant; it changes dynamically throughout the day depending on the time of day and the functional state of the body. For example, the level of leukocytes increases not only during the presence of any inflammation in the body, but also usually increases slightly in the evening, after eating, and also after physical and emotional stress.
But we are talking about those cases when the number of leukocytes decreases.
There is always some reason for this, including this natural complication of antitumor treatment.
Effect of nutritional support on tumor growth
At present, no evidence-based clinical data has been obtained indicating the effect of long-term artificial nutrition on tumor growth.
Recommendations for nutritional support:
A clinically significant effect occurs within 2 weeks.
The duration of the appointment is not limited.
Siping mixtures should be consumed slowly and in small sips through a straw for 20-30 minutes.
Nutrient mixtures can be consumed either chilled or warm, but not above + 40 °C.
Based on specialized nutrition, you can prepare milkshakes, add it to cereals, purees, salads and desserts.
Most patients need to continue nutritional support on an outpatient basis as part of rehabilitation.
Why does this state matter to us?
Leukocytes are responsible for immunity and resistance to various unfavorable factors, therefore, when their level in the blood decreases, the body’s “defense” is primarily affected.
In this case, a person becomes more vulnerable to any infection: bacterial, viral or fungal.
In most cases, with the development of infectious complications, specialized antitumor treatment should be postponed. Consequently, in addition to the main danger for humans, which lies precisely in the infectious process, we are also faced with the fact that we have to postpone the treatment of cancer indefinitely until we deal with the infection.
Do overweight patients need nutritional support?
There is such a thing as sarcopenic obesity. This condition is characterized by the fact that lean body mass decreases, but this is not visually noticeable due to the presence of excess fat mass. Sarcopenic obesity significantly worsens the prognosis of the disease.
The composition of mixtures used for nutrition in patients with excess body weight includes the following components:
- amino acids and their derivatives: arginine, glutamine, ornithine, taurine;
- lipids: omega-3 unsaturated fatty acids (EPA), medium chain triglycerides (MCT), short chain triglycerides;
- antioxidants: alpha-tocopherol, glutathione, etc.;
- dietary fiber – only in enteral formulas.
Why is it important to know about the leukocyte formula?
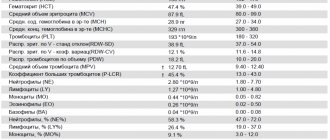
There is a so-called leukocyte formula, which is formed from subtypes of leukocytes: monocytes, eosinophils, basophils, lymphocytes and neutrophils.
Each species performs its own specific function, although it is based on immune processes.
When we receive the results of a clinical blood test, the level of leukocytes in it may be normal, but it is impossible to say offhand what part of this total indicator is this or that subtype. At the same time, this is very important for planning systemic treatment. That is why oncologists require that blood tests indicate the absolute number of all subtypes of leukocytes. The patient should also pay attention to this when receiving test results.
Neutrophils are of greatest interest to chemotherapists. This subtype of leukocytes plays a very important role in protecting the body from bacterial and fungal infections and a relatively lesser role in protecting against viral infections. Neutrophils play virtually no role in antitumor or anthelmintic defense; other cells participate in these processes.
During chemotherapy, the level of neutrophils is a critically important indicator. If the number of neutrophils falls below 0.5x10*9/l, then normal microflora, which is present, for example, in the mouth or intestines, can cause infections. If the count is reduced to <0.2 x 10*9/L, the inflammatory response may be suppressed and the usual signs of inflammation - leukocytosis or white blood cells in the urine or at the site of infection - may not be observed. Acute severe neutropenia, especially in the presence of another factor (for example, cancer and the fact of anticancer treatment), significantly impairs the function of the immune system and can lead to the development of fulminant fatal infections. The integrity of the skin and mucous membranes, blood supply to tissues, and the patient's nutrition also influence the risk of developing infections.
If chemotherapy is carried out, despite the low level of leukocytes in general and neutrophils in particular, this will lead to complete inhibition of the functioning of the bone marrow, in which our blood cells are formed and mature. This guarantees the development of all sorts of complications, which will have to be fought long and hard with a 50/50 chance of success. Therefore, it is better to postpone treatment for a week to allow the body to recover on its own, than to carry out a cycle and then return to therapy in a month at best.
In the treatment of breast cancer, gastrointestinal tract, oncogynecological diseases, lung cancer and other tumors, various combinations of drugs are used that have varying degrees of toxicity.
Therefore, in each individual case, the attending physician makes a decision on the safety of carrying out the next cycle of chemotherapy individually based on the current situation.
You should not demand or persuade the attending physician to carry out treatment, despite poor blood test results. In this case, the doctor does not want to make you worse, but he realistically assesses the risks and tries to protect you from them.
Is it possible to increase the level of leukocytes and neutrophils?
Chemotherapy drugs are toxic substances. There are indications and contraindications for their use, because they can both help the patient and cause great harm if used thoughtlessly. The only appropriate and reasonable method to increase the level of white blood cells and neutrophils is to wait.
Yes this is true.
Firstly, because each organism has its own characteristics and is not always able to recover by the time specified by the recommendations.
The intervals between cycles are optimal, but a deviation from the timing by 1-2 weeks (sometimes more, if necessary) is acceptable if there are contraindications to chemotherapy.
Secondly, any drugs that stimulate an increase in the level of leukocytes and neutrophils are dangerous because after several such stimulations, the bone marrow reserve can be depleted, and after this, recovery will take much longer and will be associated with possible complications.
If leuko- and neutropenia is constant, and the body does not recover properly even with increasing intervals between cycles, then specialized drugs are prescribed, which should be used only under the supervision of a doctor in strictly indicated situations.
Any so-called immunomodulators, immune stimulants will not bring any benefit, there will be no effect from them, because leukocytes will still decrease during chemotherapy, as it should be, but at the same time such drugs can provoke the development of undesirable reactions.
Febrile neutropenia
The combination of an increase in body temperature with a decrease in the number of neutrophils is called febrile neutropenia. This is a life-threatening condition that suddenly and acutely develops in patients against the background of a decrease in the number of neutrophils circulating in the blood below 0.5x10*9/l.
Criteria:
- number of neutrophils in peripheral blood <0.5x109/l;
- a two-fold increase in body temperature >38.00C per day or a single increase in temperature >38.30C when measuring temperature in the mouth. This means that when measuring the temperature in the armpit, you and your doctor should start to worry about a temperature above 37.50C.
The main problem is that it is very difficult for oncologists to control this complication and take the necessary measures in a timely manner, since most patients develop febrile neutropenia during the period when they are no longer in the hospital.
Therefore, the patient must also be attentive to his condition and take timely measures: contact the doctor, donate blood as soon as possible and strictly follow what the attending physician recommends.
If your body temperature rises above 38.00C, you must take a clinical blood test as soon as possible. It is important! Without its result, it is impossible to say for sure whether the patient has febrile neutropenia or whether any urgent measures are needed.
Remember that this complication can turn into a big disaster if it is not recognized and treated in time.
If a combination of both criteria occurs (the number of neutrophils in the peripheral blood <0.5x10*9/l in combination with an increase in body temperature to 380-38.30C), you must contact your doctor as soon as possible or go to the oncological institution at your place of residence.
In the absence of timely treatment within 48 hours after the development of febrile neutropenia, death occurs in 50% of cases! Even with antibacterial therapy, the risk of death remains in 10% of cases.
This suggests that this is a very dangerous complication and should not be taken lightly.
About 80% of febrile episodes against the background of a reduced level of neutrophils in the blood are associated with the development of infection, which occurs in the absence of classical symptoms (pain, flushing, swelling, fever), and the main criterion of the infectious process is high body temperature.
Until recently, fever occurring in a patient with neutropenia was the basis for mandatory hospitalization and treatment in a hospital. However, as a result of clinical studies, a system for assessing complications in patients with febrile neutropenia was created. The doctor counts the points according to this scale and can assess whether there are risks when carrying out treatment on an outpatient basis.
Clinical manifestations
Developing leukopenia can cause unpleasant symptoms:
- weakness and fatigue;
- dizziness;
- signs of intoxication;
- feeling of lack of air;
- fever, increased body temperature;
- bloating;
- frequent and painful urination;
- joint and muscle pain, cramps.
In the absence of specific medical care, bacterial complications and exacerbation of chronic infections develop. Which necessitates the abolition of chemotherapy, and this, in turn, leads to a relapse of the tumor process.
What is recommended for patients who have developed this complication?
1) If your body temperature rises, immediately take a blood test. Inform your doctor about the results of the test.
If there is a critically low level of leukocytes and neutrophils, the next administration of chemotherapy will be postponed until complete recovery.
2) Try to stick to a complete diet, exclude raw foods (that is, meat, fish, eggs, fruits and vegetables) - all foods, without exception, must be thermally processed.
3) Follow a work and rest schedule, do not overload yourself, give your body the opportunity to replenish its strength and energy for a speedy recovery.
4) Maintain personal hygiene carefully, because any infection can cause the condition to worsen.
5) Do not visit crowded places unless necessary. Maintain self-isolation. This is relevant not only during the current pandemic, because the risks of infections during febrile neutropenia are enormous - even your household can pose a danger, let alone a large number of strangers, for example, in stores.
6) If you are forced to visit a place with a large number of people, for example, to take a blood test, then be sure to wear a protective mask. Try to keep your distance from others.
The main drugs used in the treatment of febrile netropenia include antibiotics; specialized drugs are also used to stimulate an increase in the level of leukocytes and neutrophils - these are colony-stimulating factors (G-CSF).
These drugs are used to accelerate the formation, maturation and release of neutrophils from the bone marrow into the peripheral blood, where they begin to perform their functions and protect the body.
Methods for normalizing indicators based on frequent deviations
Blood restoration after chemotherapy is based on the administration of agents that increase the number of platelets and stimulate the formation of mature red blood cells. This helps to raise hemoglobin levels, improve the functioning of the heart and blood vessels, and improve blood supply to tissues.
If the patient has swelling, infiltrates, necrotic destruction of the epithelial layer, this indicates the possible death of erythrocyte sprouts of the bone marrow. In this case, a transfusion of blood, platelets or red blood cells can help. In more severe situations, you will have to resort to a bone marrow transplant.
To quickly restore your blood count, your doctor will prescribe:
- Sorbifer Durules is an antianemic drug. Active substances are iron sulfate and ascorbic acid. Thanks to this composition, oxidative processes and protein recovery from blood cells occur in the body. The tablets are taken orally (by mouth) 1-2 times a day for three months or until a normal hemoglobin level is achieved;
- Ferrum LEK is also an antianemic agent with the main component of iron hydroxide polymaltosate. Available in ampoules for intramuscular administration, chewable tablets and syrup form. The dosage is set individually according to age, clinical situation and indications;
- Totema is a combined antianemic solution for oral administration containing trace elements: iron, copper, manganese. It is necessary to strictly follow the dosage regimen prescribed by the doctor. It is possible that tooth enamel and stool may darken to black, which is considered normal;
- Filgrastim-Nanolek is a stimulator of leukopoiesis, an immunomodulator for intravenous and subcutaneous injections. Represents a non-glycosylated, highly purified protein. Causes a slight increase in the number of monocytes and a significant increase in neutrophils. Injections are given at a rate of 5-12 mcg per kilogram of body weight. The duration of the course lasts until the norm of neutrophil granulocytes is established, but no more than two weeks;
- Neupogen is an analogue of the previous one with the same effect for subcutaneous administration.
- We recommend taking VIALIFE capsules or VIALIFE solution, because they contain the highest possible concentration of chlorophyll, which: strengthens the immune system;
- enhances cell regeneration;
- saturates tissues with oxygen;
- has antioxidant, anti-inflammatory, detoxifying effects.