The disease, or Budd-Chiari syndrome, is a condition that is based on a violation of the outflow of blood through the hepatic veins. The problem may arise in the hepatic veins themselves or in the inferior vena cava, the largest vessel that collects blood from all organs of the abdominal cavity. In any case, disruption of normal hepatic blood flow adversely affects the condition of the organ.
This is a fairly rare pathology that occurs with a frequency of approximately 1 in 100 thousand people1, mainly in women.
The portal vein collects blood from the liver
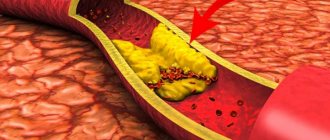
In approximately half of the cases, the cause of Budd-Chiari syndrome is a congenital or acquired increased tendency of the blood to form blood clots2. Congenital or acquired anomalies in the structure of the inferior vena cava (membranes, deformations), its compression or occlusion (blockage) by tumor masses or cysts (including echinococcosis) are also possible. In approximately 30% of cases, the cause of the disease cannot be determined3.
The following risk factors are identified that increase the likelihood of thrombosis:
- operations on the abdominal organs;
- infections and inflammations in the abdominal cavity;
- hereditary predisposition - mutations of some genes that regulate the synthesis of proteins-coagulation factors and proteins that suppress the blood coagulation system;
- myeloproliferative diseases (tumors of the hematopoietic system);
- taking hormonal contraceptives.
Violation of the outflow of blood from the liver through the hepatic vein system causes congestion, hypoxia and, as a consequence, cell death. Individual areas of liver tissue atrophy are combined with hypertrophic nodes that arise as a result of compensatory regeneration. The result is a picture similar to that of liver cirrhosis, when fibrous layers and regenerative nodes further disrupt blood flow, leading to increased pressure in the portal vein system.
The consequence of this is varicose veins of the anterior wall of the abdomen, esophagus and stomach, hemorrhoidal veins in combination with progressive liver failure.
4.Treatment
Conservative therapy includes the prescription of hepatoprotectors, anticoagulants, diuretics, and hormonal anti-inflammatory drugs. However, all these measures are usually ineffective; The mortality rate with drug treatment alone reaches 90%. Thus, the method of choice is vascular surgery (bypass surgery, angioplasty), but in this case the prognosis and surgical plan vary widely depending on the etiopathogenetic and clinical features of a particular case.
Varicose veins of the abdomen or “head of the jellyfish” in Budd-Chiari disease
The clinical manifestations of Budd-Chiari disease depend on whether this condition developed acutely or whether the process was initially chronic and part of the blood flow managed to be redistributed into the system of venous collaterals (bypass tracts of the blood flow).
Fulminant (hyperacute) course occurs with sudden massive thrombosis. There is a sharp pain in the abdomen, nausea, vomiting, and the liver enlarges. Jaundice develops quickly, followed by hepatic encephalopathy (lethargy, loss of consciousness, coma).
In the acute course of the disease, the above symptoms develop somewhat more slowly and before the appearance of hepatic encephalopathy, diuretic-resistant ascites - an accumulation of fluid in the abdominal cavity - has time to form. In both acute and hyperacute cases, the prognosis is unfavorable, since liver cells do not have time to adapt to the disruption of blood flow and die en masse.
In subacute and chronic forms of Budd-Chiari syndrome, thrombosis gradually invades the renal vein system. Bypass blood flow pathways have time to form, partially relieving the load on the liver. Necrosis of hepatocytes in this situation is not so pronounced, and symptoms develop slowly. Patients also complain of abdominal pain, but it is moderate. The first objective sign is usually ascites, resistant to diuretics. During the examination, an enlarged liver, varicose veins of the abdomen, esophagus, and hemorrhoidal plexus are detected.
3. Symptoms and diagnosis
The clinical picture is dominated by symptoms of liver dysfunction and portal hypertension. Acute forms manifest (usually after the age of 40-45 years) with severe pain in the liver, nausea, vomiting, and swelling of the legs. Due to gross violations of blood drainage and fluid removal from the body, ascites (dropsy) quickly develops. A characteristic feature is the ineffectiveness of diuretics. Jaundice is observed. As the congested vessels stretch, bleeding from the veins of the esophagus may begin. The acute form of Budd-Chiari disease/syndrome accounts for no more than 5-15% of all cases, but has a very high mortality rate within a few days from the onset of the first symptoms.
The symptoms of the chronic form are generally similar, but are much less pronounced and “stretched” over time over several years. The initial stages, sometimes very long, are often asymptomatic. Then characteristic pain appears in the right hypochondrium, external jaundice, vomiting, etc. The progression of varicose veins of the esophageal veins can lead to hemorrhages. Ascites is also one of the typical symptoms in late stages.
In diagnostic terms, clinical and biochemical blood tests and coagulograms are important. The pressure in the veins of the liver and spleen is measured (hepatomanometry, splenomanometry). Certain instrumental methods for studying the vascular systems (Doppler ultrasound, angiography) are prescribed. The size and structure of internal organs are examined tomographically, and if this is not possible, x-ray. According to indications, a histological examination (biopsy) is performed, the material for which is taken percutaneously.
About our clinic Chistye Prudy metro station Medintercom page!
Diagnosis of Budd-Chiari disease
Diagnosis of Budd-Chiari syndrome is based on ultrasound data, revealing the characteristic nodular structure of the liver and congestion. A Doppler study (ultrasound examination of blood flow velocity) is also necessary to confirm disturbances in venous outflow from the liver.
Since nodules in the liver can be a manifestation of a malignant neoplasm, additional studies are carried out to exclude oncological pathology (analysis for the level of alpha-fetoprotein, liver biopsy). To accurately determine the anatomy of the lesion in the venous system, venography may be recommended - an examination in which contrast is injected directly into the hepatic vein system. Next, a series of x-rays are taken or a computed tomography scan is performed.
Diagnostics
Diagnosis of the syndrome is made based on a thorough clinical assessment, detailed medical history, and various medical tests. Signs of liver enlargement may be detected during a physical examination.
Diagnostic tests used for this purpose include:
- Blood tests to determine if the organ is working properly.
- Ultrasound of the liver.
- MRI and CT scan of the abdominal cavity, which are performed to identify any abnormalities in the body.
Liver biopsy is another useful diagnostic procedure. During this process, the doctor takes a small sample of liver tissue for examination. Any tissue damage can be easily recognized by this test.
Hepatic vein catheterization is also performed to determine the presence of abnormalities. In this test, a catheter is inserted into the body to examine the liver veins. A small instrument attached to the tip of the catheter helps doctors measure blood pressure in the hepatic veins.
How is it diagnosed?
Budd-Chiari syndrome is indicated by a triad of signs - abdominal pain, abdominal hydrops, liver enlargement. To make an accurate diagnosis, a number of additional studies are prescribed:
- Blood chemistry. The pathological syndrome is indicated by increased activity of liver enzymes - AST and ALT.
- Clinical blood test. Stagnation of venous blood is indicated by an increased ESR, and inflammation of the liver is indicated by an excess of leukocytes.
- Coagulogram. Against the background of changes in the rheological properties of blood, an increase in prothrombin time is noted.
- Ultrasound of the liver. Using echo signs, the degree of damage to the liver parenchyma, the size of the organ and the severity of vascular disorders are assessed.
To identify stenosis of the liver veins, MRI and portography are performed. Based on the data obtained, the doctor distinguishes Budd-Chiari syndrome from myocardial insufficiency and veno-occlusive pathology.
Emergency conditions
At any stage and in any form of Budd-Chiari syndrome, the patient's condition may be aggravated by an emergency. In such cases, emergency professional medical care is necessary. This condition is characterized by:
- sudden onset of the most uncomfortable and painful symptoms;
- brown nausea and vomiting;
- difficulty urinating, small amount of urine;
- stool that resembles tar in consistency and color.
Prevention
Budd-Chiari syndrome is an extremely rare and potentially fatal disease. Early diagnosis along with timely treatment is important to ensure a relatively long and normal life for patients. There is no way to ensure prevention of this disease. However, screening and genetic testing of family members of patients with the disease will help understand the risk of developing the syndrome. This process is necessary for those diagnosed with thrombophilic disorder and a family history of Bud Chiari disease.
Proper nutrition is important to manage symptoms and prevent further liver damage. Eating a low-salt diet to maintain a negative sodium balance helps control ascites. The disease can only be prevented conditionally. Patients prone to the syndrome due to a pre-existing condition such as thrombosis, cancer or hepatitis should undergo regular screening. It is important not to put stress on the liver, for example through excessive alcohol consumption or medications.
Causes of the disease
Budd-Chiari syndrome or disease is a pathological condition characterized by venous stagnation due to a decrease in the lumen of the hepatic vessels. The pathology is diagnosed in 1 person per 100 thousand population. Women aged 40-50 years are more susceptible to it than others. In 18% of cases, the syndrome is provoked by pathologies of the hepatobiliary system - liver, gallbladder and ducts. In 1/3 of patients, the cause of thrombosis of the mesenteric (mesenteric) vessels cannot be identified.
The portal system of the liver collects blood from the unpaired organs of the peritoneum:
- pancreas;
- stomach;
- spleen.
Congenital and acquired vascular diseases lead to a slowdown in venous blood flow, which affects the functioning of many internal organs.
Depending on the origin, the syndrome is:
- Primary – a consequence of congenital pathologies of the cardiovascular system. Occurs when there is stenosis or damage to the hepatic vessels. Most often found in people living in Japan and African countries.
- Secondary is the result of structural changes in the vessels of the portal system of the liver against the background of acquired pathologies. Budd-Chiari syndrome complicates the course of pericarditis, cancer of the peritoneal organs, peritonitis, and cirrhosis of the liver.
Disruption of venous blood flow is the main cause of the clinical syndrome.
Due to the increase in hydrostatic pressure in the portal vein basin, portal hypertension is diagnosed. Depending on the rate of progression, there are 2 forms of Budd-Chiari syndrome:
- Acute – accompanied by vivid symptoms. The liver increases in volume and acquires a bluish tint. Due to stagnation of blood, the central lobes of the organ are affected, which leads to thrombosis of the central vein, congestive cirrhosis.
- Chronic – the clinical picture is erased. The walls of the liver vessels thicken. Gradually they become clogged with blood clots. If left untreated, the vessels become overgrown, transforming into fibrous cords.
Phlebologists and hepatologists identify a number of factors that provoke the syndrome:
- injuries of the peritoneal organs;
- malignant tumors;
- chronic inflammation of the liver;
- infectious diseases;
- pregnancy;
- cardiovascular pathologies;
- abuse of certain drugs.
Concomitant pathologies provoke obstruction (blockage) of the liver veins, which leads to damage to its tissue (parenchyma). Due to venous stagnation, intrahepatic pressure increases, which causes necrosis (death) of hepatocytes.
When the vessels in the portal vein are blocked, the outflow of blood is provided by the paravertebral and intercostal veins. But they cannot cope with excessive loads, resulting in serious complications.
In the last stages of the syndrome, the parenchyma in the peripheral areas of the liver becomes thinner, and in the central area it thickens. Due to the increase in its volume, the inferior vena cava is compressed, which aggravates the course of the disease.
Treatment
Treatment of Budd-Chiari syndrome is complex and depends on clinical findings and the underlying disease. Drug therapy with a blood thinning drug may be sufficient for timely diagnosed Budd-Chiari syndrome. Additionally, this form of therapy can be combined with vascular catheter studies. Hollow tubes are used to open the hepatic veins or create short circuits using special lattice vessel prostheses.
Dilation of the affected veins can relieve pressure on the vessel walls. In some cases, Budd Chiari syndrome can be treated surgically by redirecting blood flow from one vein to another (bypass). In other cases, the blocked vein is cleared and then a thin rod is inserted into it to maintain blood flow. In severe cases, a liver transplant may be required. If left untreated, worsening liver failure due to fibrosis and possible death may occur.
Note! Full recovery from Budd-Chiari syndrome is impossible. Drug therapy and surgical methods in combination prolong the life of a patient with a chronic form up to 10 years, but they are ineffective in acute diseases.
Conservative treatment
The goal of treating the disease is to maintain liver function. Doctors first determine the exact area where blood flow is obstructed. The severity of the syndrome depends on where the clot is located and the number of veins affected. Anti-clotting drugs such as urokinase are sometimes used to treat people who experience sudden onset of clotting in the hepatic veins. Patients should be treated first with heparin and then with warfarin to correct coagulation. These drugs are only used to treat the disease in its early stages, as they do not work once blood clots form.
The use of high doses of prednisolone may also be prescribed. Medicines that prevent blood clotting, such as heparin, may be useful in treating patients with the disease. Doctors may recommend topical thrombolysis, which is useful in dissolving blood clots. Systemic thrombolysis is not generally recommended as it is considered a high-risk treatment.
Radiologists will use X-ray techniques to directly examine the arteries and veins to determine the location of the clot. These procedures involve inserting a catheter into a blood vessel through an easily accessible vein in the arm, neck, or groin. Dye is then injected through the catheter to illuminate the blood vessels so they are easier to see under X-rays. In some cases, the scan shows that only the end of the vein is blocked and that most of the vein remains clear.
In other cases, when the vein is more blocked, doctors will need to access it through a tube inserted into the liver from the abdomen. Once the tube hits the blockage, doctors can remove the clot and open the vein. This is called venoplasty or angioplasty. If the clot in the hepatic veins is recent and difficult to remove, the catheter tube may be left in place for a day or two. This will give the drugs that cause the clot a chance to get rid of it. When venoplasty is successful, it results in an improvement in the patient's general condition.
Surgery
People suffering from this disease often require surgery to restore normal liver function. The specific method to be used is determined depending on the location of the blood clots and various other factors. Many other surgical techniques are also used for this treatment. Liver transplantation is performed to prolong the lives of patients who would otherwise not live beyond six months.
Other radiological interventions performed to treat patients with this type of liver disease include:
- Portosystemic shunts.
- Balloon angioplasty.
- Transjugular, portosystemic shunt.
- Surgical shunts.
However, the success rate of these surgeries differs from one patient to another. These surgical procedures can be effective, but there is a risk that they may create additional problems. Shunts mean that less blood passes through the liver to clear toxins. As a result, there is a risk that these toxins will accumulate and this can cause a condition called hepatic encephalopathy.
A liver transplant is recommended only if other treatments have failed and end-stage disease is life-threatening.
An organ transplant may be required when:
- the liver ceases to perform all its functions adequately;
- Bypass procedures cannot prevent further deterioration of health.
Note! Once a shunt is installed, there is an increased risk of infection.
Regular washing is important, especially in the affected area. Moderate outdoor exercise and a healthy diet can promote recovery.