So-called rheumatism or acute rheumatic fever (according to new terminology) is a systemic inflammatory disease of connective tissue, in which the pathological process has a tropism towards the membranes of the heart and joints.
Even at the beginning of the 20th century, the concept of “rheumatism” meant almost any disease of the joints - doctors did not have the need or opportunity to differentiate these ailments, especially since the range of healing procedures was not diverse. Today, a rheumatologist has a wide range of diagnostic methods in his arsenal, allowing him to distinguish rheumatism from many other rheumatological diseases, each of which has its own treatment strategy.
Rheumatism is a disease predominantly of children aged 6 to 15 years, and only 1 child in 1000 suffers in this age group.
Primary rheumatism in adult patients is observed less frequently. According to statistics, women are 2-3 times more likely to suffer from this disease than men.
Rheumatism usually begins some time after a streptococcal infection of the nasopharynx, and after a few years it can turn into a chronic, incurable disease. Fortunately, only 1-3% of patients who have an infection become victims of rheumatic fever.
1
Consultation with a rheumatologist
2 Consultation with a rheumatologist
3 Consultation with a rheumatologist
General information about rheumatism
Acute rheumatic fever
ー systemic inflammatory disease characterized by damage to joint tissues, heart and blood vessels. Develops in predisposed individuals after suffering a streptococcal infection (pharyngitis, tonsillitis, scarlet fever, erysipelas). Most often it develops in adolescents and young people due to the high reactivity of their immune system.
With this disease, foci of inflammation appear with tissue destruction in large and medium-sized joints, heart tissue, kidneys, and liver. The greatest danger is rheumatic heart disease. This is the most common cause of the formation of acquired heart defects and carries a risk of developing heart failure, thromboembolism (blockage with blood clots) of the pulmonary and cerebral arteries.
Causes of rheumatism
Group A hemolytic streptococcus causes the development of sore throat, scarlet fever, and erysipelas. The human immune system actively reacts to the presence of such a pathogen in the body - it produces specific antibodies that fight the microbe. But the enzymes that streptococcus produces have a toxic effect on the heart muscle. In addition, they have a similar structure to the proteins of the human body, so antibodies begin to attack not only microbes, but also their own tissues, rheumatic carditis, rheumatoid arthritis, and glomerulonephritis develop.
Therefore, rheumatic fever is considered a disease of an infectious-allergic nature - a pathogenic microorganism plays a role in its development, with hyperreactivity of the human immune system.
Many of us have had a sore throat, but only 1-3% of people develop rheumatic fever, due to the following factors:
- incorrect treatment of streptococcal infection;
- genetic predisposition;
- hypothermia;
- deficiency of vitamins and microelements;
- the presence of autoimmune diseases (lupus, scleroderma, etc.).
Clinical picture of rheumatism
The trigger for the development of rheumatism is the entry of streptococcus into the body, as a result of which the immune system begins to produce antibodies to fight the infection. However, in the body itself, namely in connective tissues and heart muscle, there are molecules of the same structure. Due to the presence of this factor, the immune system begins to “fight” its cells. As a result, connective tissue is damaged, and this is fraught with heart defects and joint deformation.
Forms of rheumatism
- cardiac form (cardiac rheumatism), when all the membranes of the heart are affected (pancarditis), myocardium (myocarditis), endocardium (endocarditis);
- articular form (rheumatism of the joints);
- cutaneous form;
- pulmonary form (pleurisy);
- rheumatic chorea (St. Vitus' dance).
Classification of rheumatism
Based on the nature of the flow, the following forms are distinguished:
- acute (up to 3 months);
- subacute (3-6 months);
- prolonged (more than 6 months);
- latent (hidden) - occurs without characteristic symptoms, without laboratory changes, is detected after the formation of heart defects;
- recurrent - wave-like course with rapid development of internal organ failure.
There are active and inactive phases of the disease. In the active, a specific laboratory picture is observed (increased levels of C-reactive protein (CRP) - reflecting acute inflammatory processes, antistreptolysin).
Clinical forms of rheumatism:
- rheumatic carditis - inflammation of the heart tissue;
- polyarthritis ー multiple joint damage;
- ring-shaped erythema - a specific rash on the skin;
- chorea - severe neurological symptoms (hand tremors, muscle weakness, involuntary movements);
- subcutaneous nodules - with the formation of dense nodules under the skin in the joint area.
What happens if you run it?
After the first attack, it can take from several months to several years. Even in the absence of symptoms, the dangerous consequences of rheumatism develop.
The most harmless of them is erythema, a reddening of the skin in the form of a red circle with clear edges. It occurs in most rheumatic diseases. In a quarter of cases, inflammation of the heart tissue leads to the appearance of defects: the heart becomes larger, murmurs appear when listening, and arrhythmia appears. Damage to the mitral valve can lead to heart failure.
Disruption of the nervous system leads to “minor chorea” - involuntary movements of the limbs, muscles of the face, body, impaired coordination, handwriting, and speech defects.
Do not start the disease, consult a doctor (pediatrician or therapist) when the first symptoms appear - both streptococcal infection and signs of rheumatism. To prevent illness, follow the prevention tips.
Symptoms and signs of rheumatism
The disease can be suspected by the following manifestations:
- development of the disease 1-2 weeks after tonsillitis, pharyngitis, scarlet fever, erysipelas;
- a sharp increase in body temperature, general weakness;
- joint pain (knee, ankle, elbow, wrist);
- swelling and redness of the skin over the joints, stiffness of movement;
- pain in the heart area;
- shortness of breath, dizziness, headache;
- muscle weakness, involuntary twitching of the limbs;
- pink rash in the form of a ring on the body, passes quickly;
- rheumatic nodules - painless, dense small formations under the skin in the joint area;
- nagging pain in the lower back, darkening, redness of urine.
If such symptoms appear, you should make an appointment with a physician, cardiologist or rheumatologist.
YOU can call us: 8 (8452) 98-84-68 and +7-967-500-8468 or
Rheumatism is a disease that develops unnoticed and gradually. It occurs after a streptococcal infection and consists of inflammation of the connective tissue, which is found in all organs and systems of the body. The heart, blood vessels and joints are primarily involved.
In modern medical literature, this term has been replaced by the generally accepted throughout the world “ acute rheumatic fever ”, which is due to the contradictory understanding of the term “rheumatism” in Russia.
Causes
The disease is triggered by special bacteria - group A beta-hemolytic streptococci. Once inside our body, they can cause tonsillitis (tonsillitis), pharyngitis, and lymphadenitis. However, rheumatism can be a consequence of this infection only if the person has certain defects in the immune system. According to statistics, only 0.3-3% of people who have had an acute streptococcal infection develop rheumatism.
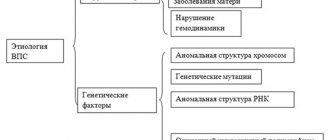
Etiology . Infection with β-hemolytic streptococcus of group A. The presence of foci of infection in the nasopharynx (angina, chronic pharyngitis, chronic tonsillitis). Scarlet fever. Genetic predisposition.
Risk factors for developing rheumatism:
- the presence of rheumatism or systemic connective tissue diseases in first-degree relatives (mother, father, brothers, sisters);
- female;
- age 7 - 15 years;
- previous acute streptococcal infection and frequent nasopharyngeal infections;
- content in the body of a special protein - B-cell marker D8/17
What's happening?
When streptococcus enters the body, the human immune system begins to fight it by producing specific antibodies. They “recognize” streptococcus by special molecules on its surface. However, the connective tissue and heart muscle of people predisposed to rheumatism contain molecules that are similar in structure. And antibodies attack the tissues of their own body. This leads to the development of an inflammatory process in the connective tissue, mainly in the heart and joints. In this case, the tissue can become deformed - this is how heart defects and joint curvatures occur.
How does it manifest itself? Typically, the first signs of rheumatism appear two to three weeks after a sore throat or pharyngitis. The person begins to experience general weakness and pain in the joints, and the temperature may rise sharply. Sometimes the disease develops very secretly: the temperature is low (about 37.0), weakness is moderate, the heart and joints work as if nothing had happened. Usually a person begins to worry only after he develops serious joint problems - arthritis.
Most often, the disease affects large and medium joints: pain appears in the knees, elbows, wrists and feet. Painful sensations can appear suddenly and disappear just as quickly, even without treatment. But make no mistake, rheumatoid arthritis has not gone away.
Another important sign of rheumatism is heart problems: irregular pulse rates (too fast or too slow), irregular heart rhythms, heart pain. A person is worried about shortness of breath, weakness, sweating. This is associated with the development of inflammation of the heart - rheumatic carditis. In 25% of cases, rheumatic carditis leads to the formation of heart disease.
After the first rheumatic attack, repeated ones with similar manifestations may occur months or years later. They can also lead to joint deformities and heart defects.
If the nervous system is affected by rheumatism, the patient experiences involuntary movements of various muscles (face, neck, limbs, torso). This is manifested by grimaces, pretentious movements, impaired handwriting, slurred speech and is called minor chorea (the old name is the dance of St. Vitus). This disorder occurs in 12-17% of patients with rheumatism, more often in girls 6-15 years old.
Pathogenesis Pathogenesis is associated with two factors: Toxic effects of a number of streptococcal enzymes that have a cardiotoxic effect. The presence of some strains of streptococcus in common antigenic substances with cardiac tissue.
Diagnosis Only a rheumatologist . To avoid mistakes, he must conduct a comprehensive examination.
First, order a general clinical blood test in order to identify signs of inflammation.
Secondly, conduct an immunological blood test to identify specific substances characteristic of rheumatism. These substances appear in the blood no earlier than a week after the onset of the disease and reach a maximum by 3-6 weeks.
To clarify the extent of heart damage, electrocardiography (ECG) and echocardiography of the heart are necessary. An x-ray will help assess the condition of the joints. If necessary, arthroscopy, joint biopsy, and diagnostic puncture of the joint with examination of joint fluid are also performed.
In case of rheumatic damage to other organs, consultation with specialized specialists may be necessary.
Clinic Symptoms appear 1-3 weeks after acute streptococcal infection. Rheumatism manifests itself in 5 syndromes:
Rheumatic carditis (cardiac form) is an inflammatory lesion of the heart involving all the linings of the heart (rheumopancarditis), but primarily the myocardium (rheumomyocarditis).
Manifestations:
Symptoms of intoxication (weakness, fatigue, sweating, loss of appetite); Pain in the heart area of a pulling, stabbing nature; Increased body temperature to febrile levels (more than 38 degrees); Moderate hypotension; Tachycardia (palpitations); Changing the boundaries of the heart; Addition of symptoms of left ventricular and right ventricular heart failure; Weakening of tones, most often muting of the first tone; With severe myocardial damage, a gallop rhythm may be auscultated; A diastolic murmur may be auscultated, characterized by blood turbulence during the transition from the atria of the heart to the ventricles due to the operation of a valve affected by rheumatic endocarditis with thrombotic masses superimposed on it; In the early stages of the disease, rheumatic endocarditis is indicated by a rough systolic murmur, the sonority of which increases after physical activity; sometimes it becomes musical.
Rheumatic polyarthritis (articular form) is an inflammatory lesion of the joints, with changes characteristic of rheumatism.
Manifestations:
Predominant damage to large joints (knees, elbows, ankles); A remitting fever (38-39 degrees) appears, accompanied by sweating, weakness, and nosebleeds; Pain in the joints: feet, ankles, knees, shoulders, elbows and hands; Symmetry of the lesion; Rapid positive effect after using non-steroidal anti-inflammatory drugs; Benign course of arthritis, joint deformation does not remain.
Rheumochorea (St. Vitus's Dance) is a pathological process characterized by the manifestation of vasculitis of small cerebral vessels. Mostly occurs in children, more often in girls.
Manifestations:
Motor restlessness, activity; Grimacing, impaired handwriting, inability to hold small objects (cutlery), uncoordinated movements. Symptoms disappear during sleep; Muscle weakness, as a result of which the patient cannot sit, walk, swallowing and physiological functions are impaired; Changes in the patient’s mental state - aggressiveness, selfishness, emotional instability appear, or, on the contrary, passivity, absent-mindedness, increased fatigue.
Cutaneous form of rheumatism.
Manifestations:
Ring erythema - rashes in the form of pale pink ring-shaped rims, painless and not raised above the skin; Erythema nodosum is a limited thickening of dark red skin areas ranging in size from a pea to a plum, which are usually located on the lower extremities. Sometimes, with significant capillary permeability, small skin hemorrhages appear; Rheumatic nodules are dense, inactive, painless formations located in the subcutaneous tissue, joint capsules, fascia, aponeuroses; Pale skin, sweating;
Rheumopleurisy.
Manifestations:
Pain in the chest when breathing, worsening with inspiration; Temperature increase; Nonproductive cough; Dyspnea; On auscultation, a pleural friction noise is heard; Lack of breathing on the affected side. The digestive organs are relatively rarely affected by rheumatism. Sometimes there are acute abdominal pains (abdominal syndrome) associated with rheumatic peritonitis, which are more common in children. In some cases, the liver is affected (rheumatic hepatitis). Quite often, changes in the kidneys are detected: protein, red blood cells, etc. are found in the urine, which is explained by damage to the vessels of the kidneys, and less often - the development of nephritis.
Laboratory diagnostics
- The acute phase of rheumatism is characterized by moderate leukocytosis with a shift in the leukocyte formula to the left; subsequently, eosinophilia, mono- and lymphocytosis may be observed.
- ESR is always increased, in severe cases up to 50-70 mm/h.
- Dysproteinemia is characteristic: a decrease in the amount of albumin (less than 50%) and an increase in globulins, a decrease in the albumin-globulin ratio below one. The proteinogram shows an increase in α2-globulin and γ-globulin fractions;
- The fibrinogen content increases to 0.6-1% (normally not higher than 0.4%). C-reactive protein appears in the blood, which is absent in healthy people;
- The level of mucoproteins increases, which is detected by the diphenylamine (DPA) test. The titers of antistreptolysin, antihyaluronidase, and antistreptokinase increase significantly.
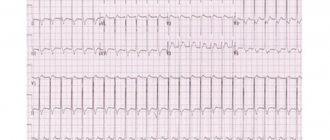
- Conduction disturbances are often found on the ECG, especially atrioventricular block of the I-II degree, extrasystole and other rhythm disturbances, and a decrease in the voltage of the ECG waves. Violation of the trophism of the heart muscle due to its inflammatory damage can lead to changes in the T wave and a decrease in the S-T segment.
- FCG reflects changes in tones characteristic of rheumatic carditis and registers the appearance of noise.
The duration of the active rheumatic process is 3-6 months, sometimes much longer. Depending on the severity of clinical symptoms and the nature of the course of the disease, there are 3 degrees of activity of the rheumatic process:
- Maximum active (acute), continuously relapsing;
- Moderately active, or subacute;
- Rheumatism with minimal activity, sluggish current, or latent. In cases where there are neither clinical nor laboratory signs of activity of the inflammatory process, they speak of the inactive phase of rheumatism.
Rheumatism is characterized by relapses of the disease (repeated attacks), which occur under the influence of infections, hypothermia, and physical stress. The clinical manifestations of relapses resemble the primary attack, but the signs of damage to blood vessels and serous membranes are less pronounced; symptoms of heart damage predominate.
Prevention Includes hardening the body, improving living conditions, working hours at work, and fighting streptococcal infections. To prevent relapses in the spring and autumn, drug prophylaxis is carried out with bicillin in combination with salicylates or ortofen (Voltaren), indomethacin, hingamine, or year-round prophylaxis is carried out with monthly administration of bicillin-5.
Features of the course of rheumatism in children
Rheumatic fever is more severe in children than in adults. The leading clinical form is carditis; heart defects form more often and faster in children.
Articular syndrome in children is less pronounced, and other extracardiac manifestations (annular rash, subcutaneous nodules, chorea) are more common with more pronounced manifestations.
But, despite its more severe course, the disease in children responds better to drug treatment, and relapses can be avoided. If symptoms of rheumatism appear, hurry up and show your child to the pediatrician. Do not deny your child medical care, follow all recommendations, all the appointments of the pediatrician, this can be vital.
Diagnosis of rheumatism
The diagnosis is made by clinical and laboratory signs. Main criteria: polyarthritis, carditis, chorea, annular rash, subcutaneous nodules.
Laboratory tests are required to confirm the diagnosis:
- general blood analysis;
- C-reactive protein level;
- level of antibodies to streptococcus and its toxins (antistreptolysin, antistreptokinase).
To assess the level of heart damage, you need to do:
- chest x-ray;
- ECG;
- echocardiography (ultrasound of the heart with Doppler sonography).
Rheumatic fever is often “missed” due to a blurred clinical picture and diagnostic errors. To prevent this from happening, get tested in trusted laboratories.
The Paracelsus Medical Center uses certified expert-class diagnostic equipment, which undergoes standardization and calibration.
All doctors work according to the principles of evidence-based medicine (international protocols drawn up on the basis of clinical trials). This minimizes the likelihood of a false diagnosis.
Prevention of rheumatism
Basic preventive measures:
- timely treatment of streptococcal infections;
- completing the full course of antibiotic therapy, if one was prescribed (you cannot stop taking antibiotics earlier than prescribed by the doctor);
- avoiding hypothermia and contact with people with tonsillitis;
- general measures to strengthen the immune system (balanced diet, physical activity, walks in the fresh air).
Effective treatment of rheumatism
Effective treatment of rheumatism should be aimed not only at suppressing streptococcal infection, but also at preventing relapse and suppressing inflammation, especially in the heart and joints. You need to know that getting rid of this serious disease must necessarily be accompanied by limiting the patient’s physical activity, which negatively affects the condition of tissues damaged by inflammation. In order to recover, it is necessary to adhere to bed rest.
If streptococcal tonsillitis is detected, the patient is prescribed internal penicillin, which is prescribed for ten days. Residual infection in a sick child is eliminated by injections of penicillin. To eliminate pain and inflammation, non-steroidal drugs, including aspirin, are prescribed.
A child who suffered from rheumatism in childhood should receive penicillin internally or intramuscularly until the age of eighteen. This is necessary in order to prevent relapse of the disease. If a person has suffered heart damage during the course of his illness, then throughout his life the patient must take an antibiotic before any operation (even tooth extraction).