- Causes of portal hypertension
- Classification
- Symptoms of portal hypertension
- Complications
- Diagnostics
- Treatment of portal hypertension
- Forecast
- Risk group
- Prevention of portal hypertension
Portal hypertension is a condition in which there is increased pressure in the portal (also known as “portal”) vein, which is located in the abdominal cavity and is responsible for transporting blood from the gastrointestinal tract to the liver. After filtration, the blood enters the heart and circulatory system. When the liver functions abnormally, the blood circulation in this organ changes, which increases the pressure in the portal vein. Blood returns to the liver, additional vessels are formed in the esophagus and stomach. They swell and can curl, which can lead to rupture, blood loss and death.
Causes of portal hypertension
The main reason is damage to the liver parenchyma. The disease is also provoked by a number of factors:
- hepatitis in acute and chronic forms;
- cirrhosis and liver tumor;
- parasitic infections;
- common bile duct tumor;
- pancreatic head cancer;
- cholelithiasis;
- intraoperative damage to the bile ducts or their ligation.
Liver damage occurs due to poisoning with hepatoprotective poisons when taking medications, mushrooms and other toxic substances. The disease is also provoked by vascular pathologies of the liver:
- thrombosis, compression as a result of tumor formation, stenosis, atresia;
- Budd-Chiari syndrome, which develops thrombosis of the hepatic veins;
- increased pressure in the right side of the heart.
Portal hypertension can develop against the background of critical conditions due to operations, injuries, burns, sepsis and disseminated intravascular coagulation syndrome. The causes of the disease can be infections and bleeding in the gastrointestinal tract. Long-term use of tranquilizers, diuretics, alcohol, and a diet containing excess animal proteins contributes to increased pressure in the portal vein.
In addition, reasons may be:
- impaired blood flow;
- increased blood flow volume;
- resistance of the vein branches;
- outflow of blood into the central veins.
The clinical picture of the disease includes four stages: initial, moderate, severe, and with complications.
Complications
The main complications: gastrointestinal bleeding, ascites and hepatic encephalopathy (liver failure, a complex of mental, nervous and muscle disorders).
Splenomegaly often causes anemia, low white blood cell counts, and low platelet counts.
Common complications associated with portal hypertension are aspiration pneumonia, sepsis, renal failure, cardiomyopathy, arrhythmias, and hypotension.
Portal hypertension is a dangerous disease because it can cause bleeding. In many cases, bleeding episodes are considered medical emergencies because the mortality rate from variceal bleeding is about 50%. Esophageal varices are very common in people with advanced cirrhosis, and it is estimated that one in three people with varices will develop bleeding.
Classification
According to its form, hypertension is classified as portal or segmental, depending on the extent of the area of increased pressure. With the first, the entire network of the portal system is covered, with the second, the blood flow in the splenic vein is disrupted.
According to localization they distinguish:
- Prehepatic. Occurs as a result of damage or development of pathologies of the portal or splenic vein.
- Intrahepatic. A common form preceded by a postsinusoidal, presinusoidal or sinusoidal block.
- Posthepatic. Occurs due to thrombosis and damage to the portal vein (Budd-Chiari syndrome)
If the cause of the condition is liver cirrhosis or portal vein thrombosis, a mixed form of pathology develops.
Publications in the media
Portal hypertension (PH) is an increase in pressure in the portal vein system (normal pressure is 7 mm Hg), developing as a result of obstruction of blood flow in any part of this vein. Increase over 12–20 mm Hg. leads to expansion of the portal vein anastomoses. The outflow of blood from the portal vein through dilated collaterals increases. Varicose veins rupture easily, leading to bleeding.
Classification • Suprahepatic PH - an obstruction in the extra-organ parts of the hepatic veins or in the inferior vena cava proximal to the point where the hepatic veins enter it • Subhepatic PH - the obstacle is localized in the trunk of the portal vein or its large branches • Intrahepatic PH - an obstruction to blood flow is located in the liver itself.
ETIOLOGY
• Intrahepatic causes •• Liver cirrhosis •• Nodular regenerative hyperplasia (with rheumatoid arthritis, Felty's syndrome) •• Acute alcoholic hepatitis •• Reception of cytostatics (methotrexate, azathioprine, 6-mercaptopurine) •• Vitamin A intoxication •• Schistosomiasis •• Sarcoidosis • • Alveococcosis •• Caroli's disease •• Wilson's disease •• Congenital liver fibrosis (hepatoportal sclerosis) •• Gaucher's disease •• Polycystic liver •• Liver tumors •• Partial nodular transformation of the liver •• Non-cirrhotic hepatoportal sclerosis (Banti's disease) •• Hemochromatosis •• Chronic hepatitis •• Myeloproliferative diseases •• Exposure to toxic substances (vinyl chloride, arsenic, copper) •• Idiopathic PG.
• Prehepatic causes (blockade of portal inflow) •• Compression or thrombosis of the portal or splenic vein trunk •• Surgical interventions on the liver, bile ducts; splenectomy •• Damage to the portal vein as a result of trauma or penetrating injury •• Aneurysms of the splenic or hepatic artery •• Severe splenomegaly in myeloproliferative diseases (polycythemia, osteomyelofibrosis, hemorrhagic thrombocythemia) •• Congenital anomalies of the portal vein •• Very rarely, portal vein block is associated with cirrhosis liver, migratory thrombophlebitis, retroperitoneal fibrosis.
• Posthepatic causes (hepatic outflow block) •• Budd-Chiari syndrome •• Constrictive pericarditis (eg, pericardial calcification) causes increased pressure in the inferior vena cava, increasing resistance to venous flow in the liver •• Thrombosis or compression of the inferior vena cava.
Pathogenesis • When outflow through the portal vein is disrupted, portal blood flows into the vena cava through venous collaterals, which significantly expand. The main clinical significance is the expansion of the veins of the lower third of the esophagus and the fundus of the stomach, because varicose veins easily rupture, which leads to bleeding • Due to the development of collateral circulation, the amount of portal blood flowing to the liver decreases and the role of the hepatic artery in the blood supply to the liver increases • With significant portosystemic shunting, hepatic encephalopathy may develop.
Pathomorphology • The spleen is enlarged, full of blood • The vessels of the portal system and spleen are enlarged, tortuous, they may contain aneurysms, hemorrhages, mural thrombi • Changes in the liver depend on the cause of PG • Varicose veins of the esophagus, stomach, rectum.
History • Presence of cirrhosis or chronic hepatitis • Indication of a history of gastrointestinal bleeding • Indications of alcohol abuse, blood transfusions, viral hepatitis B, C, taking oral contraceptives and hepatotoxic drugs, contact with hepatotoxic substances, sepsis and inflammatory diseases of the abdominal organs , myeloproliferative diseases, history of tendency to hypercoagulability • Presence of liver diseases in relatives.
Clinical picture
• Classical signs observed in all types of PG •• Development of collateral circulation - expansion of the saphenous veins of the anterior abdominal wall (head of Medusa), veins of the lower 2/3 of the esophagus, fornix and cardia of the stomach, hemorrhoidal veins •• Bleeding from varicose collaterals - esophagus -gastric bleeding (hemoptysis, melena), hemorrhoidal bleeding • Splenomegaly •• Ascites •• Dyspeptic disorders (pain in the epigastric region, a feeling of heaviness in the hypochondrium, anorexia, nausea, constipation, etc.).
• Clinical manifestations depending on the form of PH •• Suprahepatic form ••• Early development of ascites ••• The appearance of ascites is accompanied by pain in the right upper quadrant of the abdomen ••• Peripheral edema ••• Significant hepatomegaly with relatively small splenomegaly ••• Moderate jaundice • • Subhepatic form ••• The first sign may be esophagogastric bleeding or asymptomatic splenomegaly ••• Hypersplenism ••• Hepatic encephalopathy develops frequently and can take a chronic course ••• The liver is not enlarged, of normal consistency •• Intrahepatic form ••• Early symptoms - persistent dyspeptic syndrome without changes in the stomach, flatulence, periodic diarrhea, weight loss ••• Late symptoms - significant enlargement of the spleen, varicose veins with possible bleeding, ascites ••• Signs of liver failure ••• Often the first bleeding can be fatal , because liver function sharply deteriorates.
• Indirect signs of liver damage •• Liver failure •• Pancreatic insufficiency •• Spider veins and asterisks on the skin •• Hepatic encephalopathy.
Laboratory tests • In the CBC - signs of hypersplenism (thrombocytopenia, leukopenia, anemia) • In liver function tests - changes characteristic of chronic hepatitis and liver cirrhosis (with intrahepatic PH) • Determination of the etiology of chronic hepatitis/liver cirrhosis •• Determination of markers of viral hepatitis • • Detection of autoantibodies •• Determination of iron concentration in blood serum and in the liver •• Determination of a1-antitrypsin activity in blood serum •• Determination of daily copper excretion in urine and quantification of copper content in liver tissue.
Instrumental studies • Esophagography • FEGDS allows to identify varicose veins of the esophagus and stomach •• I degree - when pressing with an endoscope, the size of the veins decreases •• II degree - when pressing the veins do not decrease •• III degree - the veins merge along the entire circumference of the esophagus •• Usually veins are white •• A change in color to red or bluish indicates a high probability of bleeding • Sigmoidoscopy: varicose veins are clearly visible under the mucous membrane of the rectum and sigmoid colon • Ultrasound allows you to assess the diameter of the portal and splenic veins, determine the presence of collaterals, and diagnose portal thrombosis veins Dopplerography allows you to identify the structure of the portal vein and hepatic artery, portosystemic shunts and blood flow through them, determine the speed of portal blood flow • CT • MRI allows you to very clearly visualize the vessels • Venography is necessary to verify portal vein thrombosis, before operations of portosystemic shunt, resection or liver transplantation • Angiography allows you to detect space-occupying formations in the liver • Radioisotope study allows you to evaluate hepatic blood flow by the clearance of colloidal denatured albumin labeled 131I from peripheral vessels • Determination of pressure in the portal vein •• Measurement by wedge pressure: a catheter with a balloon at the end is inserted through the femoral vein into the hepatic vein, o catheter jamming is indicated by regular fluctuations in the measured pressure ••• The measured pressure corresponds to the pressure in the sinusoids ••• After measuring the wedge pressure, the balloon is deflated and the pressure in the hepatic vein is determined ••• The difference between the wedge pressure and the pressure in the hepatic vein is equal to the portal pressure •• Splenomanometry - puncture of the spleen with a needle connected to a water pressure gauge; normally, the pressure does not exceed 120–150 mm water column, with significant PH - 350–500 mm water column •• Hepatomanometry: intrahepatic pressure is normal - 80–130 mm water column, with cirrhosis - increases by 3– 4 times Note: the last two methods are contraindicated in case of hemocoagulation disorders.
Differential diagnosis • Liver cirrhosis • Budd-Chiari syndrome • Myeloproliferative diseases • Constrictive pericarditis • Sarcoidosis • Vitamin A intoxication.
TREATMENT
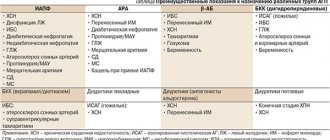
Management tactics • Treatment of the underlying disease • Prevention of the first episode of bleeding or re-bleeding in cirrhosis: •• Non-selective b-blockers, for example propranolol 20-180 mg 2 times / day in combination with sclerotherapy or ligation of varicose vessels •• Alternative drug - long-acting nitrates , such as isosorbide mononitrate. Ineffective in decompensated cirrhosis • If signs of gastrointestinal bleeding appear, immediate hospitalization.
Stopping bleeding • Terlipressin 1 mg IV bolus, then 1 mg every 4 hours for 24 hours - acts more stable and longer than vasopressin • Somatostatin 250 mg IV bolus, then 250 mg IV drip for an hour ( infusions can be continued for up to 5 days) reduces the frequency of recurrent bleeding by 2 times. Somatostatin impairs blood circulation in the kidneys and water-salt metabolism, so in case of ascites it should be prescribed with caution • Endoscopic sclerotherapy (“gold standard” of treatment) •• Preliminary tamponade is carried out and somatostatin is administered •• Sclerosant drug (5% ethanolamine solution, 1% sodium tetradecyl sulfate solution, etc.), injected into varicose veins, leads to their thrombosis •• Manipulation is effective in 80% of cases • Esophageal tamponade using a Sengstaken-Blakemore probe •• After inserting the probe into the stomach, air is injected into the cuffs, pressing the veins of the cardial part of the stomach and the lower third of the esophagus. The esophageal balloon should not be kept inflated for more than 24 hours • Endoscopic ligation of varicose veins of the esophagus and stomach with elastic rings •• Efficiency is the same as with sclerotherapy, but the procedure is difficult in conditions of ongoing bleeding •• Prevents recurrent bleeding, but does not affect survival.
Surgical treatment (see also Gastroduodenal bleeding).
• Emergency surgery is indicated when the above treatment methods are ineffective •• Emergency portacaval shunting; effectiveness depends on the initial somatic condition •• Transjugular intrahepatic portosystemic shunting is the method of choice for massive bleeding that recurs after 2 sessions of sclerotherapy •• Emergency mesentericocaval anastomosis •• Transection of the esophagus.
• Planned surgical treatment of varicose veins of the esophagus and stomach is performed to prevent recurrent bleeding if bleeding prevention with propranolol or sclerotherapy is ineffective. Survival is determined by the functional state of the liver. Shunt operations lead to a decrease in pressure in the portal vein system and decompression of varicose veins of the esophagus and stomach. The most serious complication is the development of hepatic encephalopathy •• Portacaval shunting - the portal vein is connected to the inferior vena cava ••• The operation is indicated with a good functional reserve of the liver ••• After the operation, the likelihood of ascites, spontaneous bacterial peritonitis, hepatorenal syndrome is reduced •• Mesentericocaval shunting - sewn in prosthesis between the superior mesenteric and inferior vena cava •• Selective splenorenal shunt - varicose veins are crossed, resulting in blood being directed into the splenic vein, anastomosed with the left renal vein •• Transjugular intrahepatic portosystemic shunt - connection of a branch of the portal vein and the hepatic vein inside the liver with using an expandable metal stent.
• Liver transplantation is indicated for patients with cirrhosis who have suffered at least 2 episodes of bleeding requiring blood transfusions.
Complications • Bleeding from varicose veins of the esophagus and cardia of the stomach (most often); less often - from hemorrhoids of the rectum (see Gastroduodenal bleeding) • Hepatic encephalopathy • Renal failure • Sepsis • Spontaneous bacterial peritonitis • Ascites • Hepatorenal syndrome.
Observation • Patients must be observed in a specialized center • Patients with compensated PG without varicose veins undergo FEGDS once every 2-3 years, with small nodes - once every 1-2 years
Prognosis • Depends on the underlying disease. In cirrhosis, it is determined by the severity of liver failure •• The one-year survival rate of patients in groups A and B according to Child is 70%, in patients in group C - 30% •• The mortality rate for each bleeding is 40%.
Reduction. PG - portal hypertension
ICD-10 • K76.6 Portal hypertension
Note. Hypersplenism in PG occurs frequently. In approximately half of patients who undergo portocaval shunting, hypersplenism resolves. Splenectomy for portal hypertension is rarely performed.
Symptoms of portal hypertension
The disease manifests itself:
- bloating;
- unstable stool;
- feeling of a full stomach;
- lack of appetite;
- nausea;
- pain in the right hypochondrium;
- rapid fatigue;
- weight loss;
- jaundice.
An increased size of the spleen is also a sign of pathology. The size of the organ decreases after bleeding from the gastrointestinal tract, as a result of decreased pressure in the portal vein.
Sometimes the pathology is accompanied by the formation of abdominal dropsy with a persistent course. The volume of the abdomen increases, the ankles swell, and branching veins are noticeable on the anterior abdominal wall, visually resembling a jellyfish.
Portal hypertension does not have its own symptoms, but is manifested by complications. When fluid accumulates, the volume of the abdominal cavity increases, which is accompanied by pain. With an enlarged spleen, discomfort is felt in the left side of the abdomen. As a result of varicose veins, bleeding occurs, vomiting with blood, and dark-colored clots are possible.
With varicose veins in the rectum, the stool contains blood, and severe bleeding increases the risk of death.
When toxins from the liver enter the bloodstream and reach the brain, this can lead to mental confusion.
Course of the disease
The course of the disease can be divided into 4 stages:
Stage I - initial
The disease has already appeared, but cannot yet be diagnosed. It is asymptomatic, or patients feel heaviness in the right hypochondrium and mild malaise.
Stage II - moderate
Pronounced clinical symptoms of the disease appear. Pain in the upper abdomen, flatulence, digestive disorders (belching, heartburn, heaviness in the abdomen, etc.), splenomegaly and hepatomegaly (enlarged liver).
Stage III - pronounced
All the signs and symptoms of portal hypertension are present in a pronounced form.
Stage IV - stage of complications
Intense ascites develops, difficult to treat, repeated bleeding, as well as possible complications.
Diagnostics
Portal hypertension is diagnosed by carefully studying the patient’s medical history, after assessing the condition and based on the results of instrumental studies. During the examination, the doctor evaluates signs of collateral circulation, especially for dilated veins in the abdomen, the appearance of tortuous vessels in the navel area, the occurrence of a periumbilical hernia, and hemorrhoids.
Laboratory tests include clinical analysis of blood and urine. A study of biochemical parameters, antibodies to the hepatitis virus, and coagulogram is required. The level of portal blood flow blockage and the possibility of using vascular anastomoses can be assessed using radiographic and other studies. Ultrasound is required to determine pathologies of the abdominal organs. Laparoscopy and liver biopsy are required to confirm the disease causing portal hypertension.
Treatment of portal hypertension
Treatment is required for functional changes in intrahepatic hemodynamics. Therapy includes taking β-blockers, ACE inhibitors, glycosaminoglycans and nitrates. In case of acute development of the disease, with varicose veins of the stomach and esophagus, they resort to ligation and sclerosis. If conservative methods are ineffective, suturing of veins through the mucosa is indicated.
Indications for surgical intervention are bleeding, hypersplenism, and ascites. The patient is fitted with a vascular portacaval anastomosis, which provides a bypass for the anastomosis. In accordance with the form of the disease, shunting, splenectomy, and reduction are performed. In case of complicated or decompensated pathology, drainage of the abdominal cavity is performed.
Prevention of portal hypertension
A number of liver diseases caused by metabolic disorders cannot be prevented.
The same applies to congenital anatomical features. However, portal hypertension also develops against the background of uncontrolled use of medications, stimulants and alcohol. To prevent the development of the disease, it is necessary to take medications strictly as prescribed by the doctor, and if side effects occur, consult a medical specialist to adjust the therapy. Prevention of the disease is to avoid alcohol or reduce its consumption to a minimum. You should not take narcotic drugs, as they often cause the development of hepatitis B and C, which contributes to the development of liver cirrhosis and, accordingly, portal hypertension.