Transient ischemic attack of the brain is a temporary acute disorder of the central nervous system. In medical practice, such a pathology may also be called a microstroke. The only difference is the duration of symptoms. In the case of transient ischemia, the signs disappear within an hour; they do not have irreversible consequences. Most often, this type of disorder is found in older people.
Diagnosis is carried out on the basis of the totality of all information obtained through medical research: computed tomography, magnetic resonance imaging, ultrasound and PET scans of brain regions. Additionally, laboratory procedures may be prescribed. It is advisable to undergo the examination in specialized neurological centers.
Treatment of transient ischemic attack of the brain can be conservative, symptomatic and surgical. It all depends on the patient’s age, the presence of concomitant diseases and general condition. Therapy is necessary to eliminate the risk of stroke. According to statistics, a patient’s risk of stroke after 2 days after an attack is 4%, after 30 days - 8%, within 5 years - 29%.
ICD-10 code
TIA in ICD-10 (International Classification of Diseases, 10th revision) is as follows: Transient transient cerebral ischemic attacks (attacks) and related syndromes (G45). TIA is included in the group of episodic and paroxysmal disorders (G40-G47).
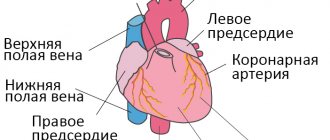
A transient ischemic attack occurs as a result of blockage of a vessel supplying the brain. Atherosclerotic plaques or blood clots may form in the vessel, interfering with normal blood flow. Rarely, TIA occurs as a result of hemorrhage. However, in this case, blood circulation is restored quite quickly.
Make an appointment
What happens in the blood vessels and cells of the brain?
During an ischemic attack, the arteries that carry oxygen and nutrients to different parts of the brain undergo a short-term spasm. This is caused by a disturbed vascular reaction, a failure of the “control” function of the cortical nuclei.
Perhaps their negative role is played by:
- vascular inferiority due to genetic predisposition;
- impaired coagulating properties of blood (hyperprothrombinemia increases thrombus formation);
- the process of autoallergy - the formation of antibody complexes on the inner walls of blood vessels;
- inflammatory reactions in vasculitis.
Even a short-term interruption in the supply of brain cells (neurons) disrupts the internal energy production process, causes oxygen deficiency (hypoxia), and suspends all types of metabolism.
Clinical symptoms depend on the extent of the lesion and its location. They differ from the manifestations of a stroke by returning to normal within 24 hours.
Causes
TIA is not an independent disease; its occurrence is associated with pathologies of the cardiovascular system, blood clotting problems, vascular injury and large blood loss. The causes of thromboembolism are most often associated with:
- atrial fibrillation;
- sick sinus syndrome;
- mitral stenosis;
- atrial fibrillation;
- dilated cardiomyopathy;
- infective endocarditis;
- atrial myxoma;
- acute heart attack;
- thrombosis of the left atrium.
TIA can occur in patients with:
- patent oval valve;
- artificial heart valve;
- mitral valve calcification;
- heart disease;
- heart failure;
- angiopathy;
- coagulopathy;
- abnormalities in the vertebral and carotid arteries.
Carotid artery lesions
The appearance of typical symptoms is observed after a 2-5 minute period. When the circulation of the circulatory system in the area of the carotid artery is dysfunctional, the patient feels weak, suddenly loses vision, and completely or partially stops speaking.
Motor dysfunction of the limbs on one side is often observed, and the patient also loses sensation.
The pulse drops rapidly and a noise is heard in the carotid artery. The disease may be indicated by focal symptoms of damage to the brain structures of the head: the face becomes asymmetrical, the pressure fluctuates, the retina changes.
There is a feeling of heaviness in the sternum area, the heart is working intermittently, there is not enough air to breathe, convulsions appear, and you want to cry.
Risk factors
In most cases, transient ischemic attack is caused by atherosclerotic plaques blocking small blood vessels. The risk group for developing transient ischemic attack includes persons suffering from the following diseases and conditions:
- atherosclerosis of cerebral vessels - this pathology is considered the main cause of ischemic attacks. 90% of strokes in older people are caused by atherosclerosis;
- arterial hypertension – ranks second in the incidence of strokes;
- hereditary predisposition - if any of the family members have similar conditions in the past, the likelihood of developing an ischemic stroke increases;
- age factor - after 60 years, the risk of developing the disease increases significantly.
- diabetes mellitus – hypertension and increased blood clotting in patients with diabetes lead to worsening atherosclerotic damage to blood vessels;
- systemic vascular diseases;
- obesity – excess body weight is quite often the cause of ischemic attacks;
- heart diseases;
- osteochondrosis of the cervical spine, especially spasm of the cervical artery;
- alcohol abuse and smoking.
According to statistics, transient ischemic attacks more often affect middle-aged male patients. However, symptoms can also appear in childhood and young adults with cardiovascular disease.
Diagnosis of transient ischemic attack is carried out on the basis of information obtained during medical research:
- computed tomography;
- magnetic resonance imaging;
- Doppler ultrasound;
- positron emission tomography of all parts of the brain.
To make the most accurate diagnosis, additional laboratory procedures may be prescribed.
Paroxysmal systemic dizziness
Paroxysmal systemic dizziness is the most common symptom of focal circulatory disorders, both in the brain stem and in the structures of the inner ear.
A reliable criterion for brainstem vertigo, according to Sarklinik, is the combination of dizziness with cerebral symptoms proper, for example oculomotor, visual, pyramidal, and sensory symptoms. A reliable criterion for peripheral dizziness is the combination of dizziness with cochlear disorders.
The manifestation of paroxysmal dizziness in the form of a monosyndrome in most cases indicates its peripheral origin.
In the differential diagnosis of peripheral or central dizziness, the phenomenon of accelerated growth of vestibular excitability - vestibular recruitment - is of great importance. With central vertigo it is negative, with peripheral vertigo it is positive.
Clinical manifestations
A transient ischemic attack contributes to the occurrence of temporary neurological symptoms. Therefore, at the time of consultation, the neurologist does not have all the signs; the specialist is based only on the patient’s complaints during the interview. Depending on the location of the pathology, the clinical picture will also change.
Disorders in the vertebrobasilar region (VBP) cause unsteadiness of gait, instability, dizziness, dysarthria (fuzzy speech), vision problems, and sensory abnormalities.
Changes in the carotid system lead to a sharp deterioration in vision, temporary blindness of one of the organs, impaired mobility in the limbs, and rarely convulsions. These signs are short-term.
TIA in the retinal area, when the pathology affects the artery of the visual organs, which leads to transient blindness. Patients complain of an obstacle in the form of a “curtain”.
A TIA attack lasts no more than 15–20 minutes, after which all neurological manifestations disappear. It is because of this short-term ailment that people do not pay attention to it and do not visit the clinic. This disorder can occur once in a lifetime or recur regularly (up to three times a day). There are as many manifestations of TIA as there are functions of the brain. Temporary deviations can be observed in speech, memory, and behavior.
Physiology of the disease
TIA develops due to the inability of blood vessels to supply neurons with oxygen. The severity of the condition can vary greatly. Doctors often find it difficult to draw a clear line between a transient attack and an ischemic stroke, since they develop according to a similar scenario.
At the moment, there is only one criterion that allows you to distinguish a TIA from a stroke - TIA lasts less than 24 hours. With a stroke, circulatory disturbances persist for more than a day.
General signs
Common signs of a TIA include:
- severe tinnitus;
- flashes of light in the eyes;
- severe hiccups;
- nausea or vomiting;
- speech problems;
- pain in the back of the head;
- dizziness;
- severe headaches;
- coordination problems;
- convulsive state;
- blood pressure surges;
- transient amnesia.
Patients experience pale skin, absent-mindedness, and inability to concentrate. If the pathology is localized in the cervical region, then situational attacks cause the appearance of severe muscle weakness - the patient may fall, lose the ability to freely move the limbs, most often the victim is fully conscious. In severe cases, a person requires immediate emergency care.
Symptoms of cerebral ischemic attack
The clinical picture of TIA depends on the location of the damaged cerebral vessel.
Manifestations of vertebrobasilar artery obstruction:
- Excessive sweating;
- Intra-ear noise;
- Dizziness;
- Coordination disorders;
- Local amnesia (memory loss);
- Visual disturbances – double vision of objects, loss of areas of the visual image, light flashes;
- Occipital pain.
A common manifestation of vertebrobasilar syndrome is a short-term loss of consciousness, a positive Romberg test (the inability to touch the tip of the nose with a finger).
Severity criteria
There are 3 degrees of severity of TIA. They indicate the positive or negative dynamics of the disease:
- mild degree - lasts approximately 10 minutes, focal symptoms that disappear without consequences;
- moderate degree - lasts from 10 minutes or more, the attack occurs without consequences for the patient’s health;
- severe - transient cerebral ischemic attack is prolonged, and neurological signs worsen.
According to ICD-10, transient ischemic attack has a standard classification:
- TIA in the VBB (vertebrobasilar area);
- TIA in the carotid region;
- TIAs are multiple or bilateral;
- transitional blindness syndrome;
- TGA (transient global amnesia);
- unspecified TIA.
The type and severity of local decrease in blood circulation in the head can only be determined by a qualified medical professional.
Diagnostics
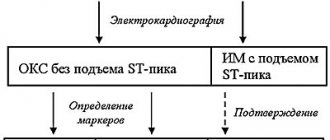
If you follow the recommendations of the World Health Organization, then all patients with suspected TIA should be taken to a regional vascular center. The speed of the examination (within 24 hours) will significantly increase the chances of finding out the picture of general changes. The list of procedures includes:
- conducting MRI using diffusion-weighted images and gradient T2-weighted images;
- A CT scan is performed if it is not possible to do an MRI;
- ultrasound examination of the vessels of the head and neck if there is a suspicion of a stroke;
- clinical examination of physiological parameters with blood tests;
- conducting an ECG.
Additional procedures include:
- echocardiography;
- checking blood for clotting;
- biochemical blood tests.
The diagnostic criteria for transient ischemic attack are based on the ABCD2 scale, which is widely used in Western Europe and the USA. It can be used to predict the risk of stroke in patients who have suffered a TIA.
The assessment school looks like this:
- A - blood pressure indicators;
- B — patient’s age (over 60 years);
- C — symptoms of the disease (general list of ailments);
- D—duration of symptoms and history of diabetes.
This approach allows for an objective assessment of both mild and more severe manifestations of ischemia.
A complete examination of the patient will allow differentiation of TIA from other diseases, such as:
- Neurological disorders: migraines, focal seizures, brain tumor, subdural hematoma, hemorrhage, multiple sclerosis, myasthenia gravis, paralysis and narcolepsy.
- Somatic and mental disorders: hypoglycemia, Meniere's disease, vestibular neuritis, syncope, orthostatic hypotension, hysteria, psychosomatic abnormalities.
There is a range of significant signs with the help of which we can more likely speak about the correct differentiation of acute VBD from other diseases. These include:
- rotational dizziness;
- degree of feeling of unsteadiness or stability in an upright position;
- balance problems;
- the presence of cystic-glial changes in the head;
- the presence of atherosclerosis of the brachiocephalic arteries with stenosis exceeding 50%.
TIA is characterized by the presence of several signs, so the patient’s condition requires a qualitative analysis.
Treatment
The most important thing is to provide the victim with appropriate assistance in a timely manner, since it is difficult to make a diagnosis at first glance. You should know that emergency care is available. This is a series of specific actions aimed at stabilizing the patient’s condition and hospitalization:
- calling an ambulance;
- control of breathing, heart rate and blood pressure;
- relief of convulsive syndrome.
The victim should be given the opportunity to breathe freely: loosen his tie or unbutton the top buttons of his clothes, open the window. Be sure to take a horizontal or half-sitting position. If vomiting occurs, clear the airways. The patient can be given a small amount of water.
The goal of TIA therapy is to prevent subsequent attacks with the development of complications. First of all, the decrease in blood supply is stopped, followed by restoration. Doctors select treatment based on the underlying disease: diabetes mellitus, arterial hypertension, thromboembolism or other pathologies.
The duration of treatment depends on the specific case. The patient can undergo the recovery period on an outpatient basis or in a clinic. He may be prescribed:
- infusion therapy, when Reopoliglucin or Pentoxifylline is injected drip into a vein;
- antiplatelet agents: acetylsalicylic acid, Clopidogrel, which prevent the formation of blood clots;
- anticoagulants: Clexane, Fraxiparine. They require monitoring of blood counts;
- neuroprotectors: Magnesium sulfate, Ceraxon, Actovegin. With their help, nerve cells receive appropriate protection from oxygen starvation;
- nootropics: Cerebrolysin, Piracetam;
- statins: Atoris, Vaseline - help lower the concentration of cholesterol in the blood;
- antiarrhythmic drugs are prescribed for heart rhythm disturbances;
- antihypertensive agents: Lopril.
According to indications, symptomatic treatment can be carried out, which is prescribed individually. The attending physician may prescribe physiotherapeutic procedures, including:
- Oxygen barotherapy is a treatment with an air environment with a high oxygen content, which promotes cell regeneration.
- Electrosleep is therapeutic; it allows subcortical connections to be restored through exposure to a safe pulsed current.
- Electrophoresis - the effect of current pulses in combination with the administration of drugs.
- DDT (diadynamic therapy) is one of the methods of electrotherapy, when the patient’s body is exposed to Bernard currents. They have low frequency and voltage.
- SMT is the effect of sinusoidal currents on biological tissues. They have a beneficial effect on the entire body.
- Microwaves - human tissues and organs are affected by a specially created electromagnetic field, its wavelength is 12.6 cm, and its frequency is 2375 MHz.
- A circular shower is a useful hydroprocedure; its principle is the needle-like effect of streams of water on the human body over the entire surface. The water from such a shower envelops the entire body. The procedure takes place in a special box, which is equipped with a large number of tubes, from which water is supplied.
- Therapeutic baths (pine, radon, pearl).
According to indications, massage procedures aimed at improving blood circulation can be used. Surgical intervention is prescribed for atherosclerotic lesions of extracranial vessels. This procedure has 3 varieties:
- carotid endarterectomy - removal of atherosclerotic plaque located inside the vessel;
- arterial stenting - the procedure is performed on narrowed arteries;
- prosthetics - the affected area of the artery is removed and replaced with a graft.
A patient suffering from a TIA requires professional advice from appropriate specialists. Treatment after a transient ischemic attack will depend on the cause of the attack, frequency and age of the patient. If the symptoms are mild and attacks are sporadic, then recovery is quick.
Neurological rehabilitation after transient ischemic attack at the Yusupov Hospital
The rehabilitation clinic of the Yusupov Hospital is a unique medical institution, whose specialists direct all their efforts to restore patients’ body functions lost due to illness.
Our rehabilitation doctors include unique rehabilitation programs, innovative medical technologies and techniques in the scheme of rehabilitation measures.
Exercise after transient ischemic attack and stroke
Physical therapy (physical therapy) is a mandatory and very powerful tool for recovery after a transient ischemic attack. Neurologists at the Yusupov Hospital prescribe it in the first days after an attack. Exercise therapy should be performed at all stages of treatment, and ideally throughout the rest of life.
In terms of the strength of its positive effects, regular physical exercise after a transient ischemic attack and stroke can compete with even the most modern medications.
Physical exercises after transient ischemic attack and strokes have the following objectives:
- prevent complications of long-term immobilization (bedsores, congestive pneumonia, progression of congestive heart failure, thromboembolic complications, muscle atrophy);
- improve muscle tone and strength in muscles that are in a state of paresis or paralysis with reduced tone;
- pathological muscle tone in muscle groups in a state of spastic paresis or paralysis with increased muscle tone;
- improve microcirculation and metabolic processes in all tissues of the body;
- prevent muscle contractures;
- resume physical activity;
- restore the body’s speech functions;
- normalize the activity of internal organs;
- restore fine movements of the hands.
Therapeutic exercise is effective, but not the only method of rehabilitation after transient ischemic attack and stroke. The highest effectiveness is achieved if exercise therapy is combined with massage, manual therapy, occupational therapy, social and psychological adaptation.
Rehabilitation after a transient ischemic attack at the Yusupov Hospital is a full-fledged recovery program that allows you to avoid the development of severe consequences of cerebrovascular accident.
Prevention
To prevent the development of transient ischemic attacks, you should follow the recommendations of specialists:
- take prescribed medications in accordance with the prescribed prescription;
- control blood pressure levels;
- monitor blood cholesterol levels;
- give up bad habits: alcohol and nicotine addiction;
- regularly take medications that prevent the formation of blood clots;
- be regularly checked by your doctor.
To prevent a transient ischemic attack from having consequences, you should lead an active and healthy lifestyle:
- eat on time and often;
- eliminate or reduce the consumption of fatty, smoked and salty foods;
- play sports: swimming, therapeutic exercises;
- spend more time outdoors.
If you adhere to all of the above, the prognosis for full recovery will be positive.
Yusupov Hospital is located near the center of Moscow. Patients are accepted here around the clock. You can make an appointment and get advice from specialists by calling the clinic.