Moxarel®
Suction
After oral administration, moxonidine is rapidly and almost completely absorbed from the upper gastrointestinal tract. Absolute bioavailability is approximately 88%, indicating no significant first-pass effect. The time to reach maximum concentration is about 1 hour. Food intake does not affect the pharmacokinetics of the drug.
Distribution
The connection with blood plasma proteins is 7.2%.
Metabolism
The main metabolite is a dehydrogenated derivative of moxonidine. The pharmacodynamic activity of the main metabolite is about 10% of the activity of moxonidine.
Removal
The half-life (T1/2) of moxonidine and the dehydrogenated metabolite is 2.5 and 5 hours, respectively. Within 24 hours, over 90% of moxonidine is excreted by the kidneys (about 78% unchanged and 13% as dehydromoxonidine, the level of other metabolites in the urine does not exceed 8% of the dose taken). Less than 1% of the dose is excreted through the intestines.
Pharmacokinetics in special groups of patients
Patients with arterial hypertension
Compared with healthy volunteers, patients with arterial hypertension show no changes in the pharmacokinetics of moxonidine.
Elderly patients
Clinically insignificant changes in the pharmacokinetic parameters of moxonidine were noted in elderly patients, probably due to a decrease in the intensity of its metabolism and/or slightly higher bioavailability.
Children
Moxonidine is contraindicated for use in patients under 18 years of age, and therefore pharmacokinetic studies have not been conducted in this group.
Patients with kidney failure
Moxonidine excretion is significantly correlated with creatinine clearance (CC). In patients with moderate renal failure (creatinine clearance in the range of 30-60 ml/min), steady-state plasma concentrations and final T1/2 are approximately 2 and 1.5 times higher than in patients with normal renal function (creatinine clearance more than 90 ml/min). min).
In patients with severe renal failure (creatinine clearance less than 30 ml/min), steady-state plasma concentrations and final T1/2 are 3 times higher than in patients with normal renal function. The administration of multiple doses of moxonidine leads to predictable accumulation in the body of patients with moderate and severe renal failure. In patients with end-stage renal failure (creatinine clearance less than 10 ml/min) on hemodialysis, steady-state plasma concentrations and final T1/2 are 6 and 4 times higher, respectively, than in patients with normal renal function. In patients with moderate renal failure, the maximum concentration of moxonidine in the blood plasma is 1.5-2 times higher. In patients with impaired renal function, the dosage should be adjusted individually.
Moxonidine is excreted to a small extent during hemodialysis.
Moxarel, 0.2 mg, film-coated tablets, 14 pcs.
Suction
After oral administration, moxonidine is rapidly and almost completely absorbed from the upper gastrointestinal tract. Absolute bioavailability is approximately 88%. The time to reach maximum concentration is about 1 hour. Food intake does not affect the pharmacokinetics of the drug.
Distribution
The binding to plasma proteins is 7.2%.
Metabolism
The main metabolite is dehydrogenated moxonidine. The pharmacodynamic activity of dehydrogenated moxonidine is about 10% compared to moxonidine.
Removal
The half-life (T1/2) of moxonidine and metabolite is 2.5 and 5 hours, respectively. Within 24 hours, over 90% of moxonidine is excreted by the kidneys (about 78% unchanged and 13% as dehydromoxonidine, other metabolites in the urine do not exceed 8% of the dose taken). Less than 1% of the dose is excreted through the intestines.
Pharmacokinetics in elderly patients
Clinically insignificant changes in the pharmacokinetic parameters of moxonidine were noted in elderly patients, probably due to a decrease in the intensity of its metabolism and/or slightly higher bioavailability.
Pharmacokinetics in children
Moxonidine is not recommended for use in patients under 18 years of age, and therefore pharmacokinetic studies have not been conducted in this group.
Pharmacokinetics in renal failure
Moxonidine excretion is significantly correlated with creatinine clearance (CC). In patients with moderate renal failure (creatinine clearance in the range of 30-60 ml/min), steady-state plasma concentrations and final T1/2 are approximately 2 and 1.5 times higher than in patients with normal renal function (creatinine clearance more than 90 ml/min). min).
In patients with severe renal failure (creatinine clearance less than 30 ml/min), steady-state plasma concentrations and final T1/2 are 3 times higher than in patients with normal renal function. The administration of multiple doses of moxonidine leads to predictable accumulation in the body of patients with moderate and severe renal failure. In patients with end-stage renal failure (creatinine clearance less than 10 ml/min) on hemodialysis, steady-state plasma concentrations and final T1/2 are 6 and 4 times higher, respectively, than in patients with normal renal function.
In all groups, the maximum concentration of moxonidine in blood plasma was 1.5-2 times higher. In patients with impaired renal function, the dosage should be adjusted individually.
Moxonidine is excreted to a small extent during hemodialysis
Description of the drug XARELTO® (XARELTO)
Concomitant use of rivaroxaban and strong inhibitors of the isoenzyme CYP3A4 and P-glycoprotein may lead to a decrease in renal and hepatic clearance and thus significantly increase the AUC of rivaroxaban.
The combined use of rivaroxaban and the azole antifungal drug ketoconazole (400 mg 1 time / day), which is a strong inhibitor of CYP3A4 and P-glycoprotein, led to a 2.6-fold increase in the average steady-state AUC of rivaroxaban and a 1.7-fold increase in the average Cmax of rivaroxaban, which is accompanied by a significant increase pharmacodynamic effects of the drug.
With simultaneous use of rivaroxaban and the HIV protease inhibitor ritonavir (600 mg 2 times / day), which is a strong inhibitor of CYP3A4 and P-glycoprotein, led to a 2.5-fold increase in the average steady-state AUC of rivaroxaban and a 1.6-fold increase in the average Cmax of rivaroxaban, which is accompanied by a significant enhancing the pharmacodynamic effects of the drug. Therefore, rivaroxaban should be used with caution when treating patients concomitantly receiving systemic azole antifungals or HIV protease inhibitors.
Clarithromycin (500 mg twice daily), a potent CYP3A4 inhibitor and moderate-intensity P-glycoprotein inhibitor, caused a 1.5-fold increase in mean AUC values and a 1.4-fold increase in Cmax of rivaroxaban. This increase in AUC and increase in Cmax are within normal limits and are considered clinically insignificant.
Erythromycin (500 mg 3 times/day), a moderate inhibitor of CYP3A4 isoenzyme and P-glycoprotein, caused a 1.3-fold increase in the mean steady-state AUC and Cmax values of rivaroxaban. This increase in AUC and increase in Cmax are within normal limits and are considered clinically significant.
Co-administration of rivaroxaban and rifampicin, a potent inducer of CYP3A4 and P-glycoprotein, resulted in an approximately 50% decrease in the mean AUC of rivaroxaban and a parallel decrease in its pharmacodynamic effects. Concomitant use of rivaroxaban with other strong CYP3A4 inducers (eg, phenytoin, carbamazepine, phenobarbital or St. John's wort) may also result in decreased plasma concentrations of rivaroxaban. The decrease in plasma concentrations of rivaroxaban is considered clinically insignificant.
After the combined use of enoxaparin (in a single dose of 40 mg) and rivaroxaban (in a single dose of 10 mg), an additive effect was observed regarding the activity of antifactor Xa, which was not accompanied by additional effects regarding blood coagulation parameters (prothrombin time, aPTT). Enoxaparin did not change the pharmacokinetics of rivaroxaban.
There was no pharmacokinetic interaction between rivaroxaban and clopidogrel (loading dose of 300 mg followed by a maintenance dose of 75 mg), but in a subgroup of patients a clinically significant increase in bleeding time was detected, which did not correlate with platelet aggregation and P-selectin or GPIIb/IIIa receptor levels .
No clinically relevant prolongation of bleeding time was observed after coadministration of rivaroxaban and 500 mg naproxen. However, a more pronounced pharmacodynamic response is possible in some individuals.
Moxarel
Moxarel tablet film 0.2 mg x30 Vertex, ATX code: C02AC05 (Moxonidine) Active substance: moxonidine Rec.INN registered by WHO
Dosage forms
MOXAREL®
tab., cover film-coated, 200 mcg: 14 or 30 pcs.reg. No.: LP-002550 dated 07/31/14 - Valid
tab., cover film-coated, 400 mcg: 14 or 30 pcs.reg. No.: LP-002550 dated 07/31/14 - Valid
Release form, composition and packaging
Tablets, film-coated, white or almost white, round, biconvex, with a cross-section showing a white or almost white core.
1 tab.
moxonidine 200 mcg
Excipients: lactose monohydrate - 64 mg, microcrystalline cellulose - 29.8 mg, colloidal silicon dioxide - 1 mg, povidone K30 - 2 mg, croscarmellose sodium - 2 mg, magnesium stearate - 1 mg.
Film coating composition: (hypromellose - 1.8 mg, talc - 0.6 mg, titanium dioxide - 0.33 mg, macrogol 4000 (polyethylene glycol 4000) - 0.27 mg) or (dry mixture for film coating containing hypromellose 60%, talc 20%, titanium dioxide 11%, macrogol 4000 (polyethylene glycol 4000) 9%) - 3 mg.
Tablets, film-coated, yellow, round, biconvex, with a cross-section showing a white or almost white core.
1 tab.
moxonidine 400 mcg
Excipients: lactose monohydrate - 64 mg, microcrystalline cellulose - 29.6 mg, colloidal silicon dioxide - 1 mg, povidone K30 - 2 mg, croscarmellose sodium - 2 mg, magnesium stearate - 1 mg.
Film coating composition: (hypromellose - 1.8 mg, talc - 0.6 mg, titanium dioxide - 0.31 mg, macrogol 4000 (polyethylene glycol 4000) - 0.27 mg, iron oxide yellow (iron oxide) - 0.02 mg) or (dry mixture for film coating, containing hypromellose 60%, talc 20%, titanium dioxide 10.33%, macrogol 4000 (polyethylene glycol 4000) 9%, iron oxide yellow (iron oxide) 0.67%) - 3 mg.
Clinical and pharmacological group: Selective agonist of imidazoline receptors. Antihypertensive drug Pharmacotherapeutic group: Central alpha2-adrenergic agonist
pharmachologic effect
Moxonidine is an antihypertensive agent with a central mechanism of action. In the brain stem structures (rostral layer of the lateral ventricles), moxonidine selectively stimulates imidazoline-sensitive receptors that take part in the tonic and reflex regulation of the sympathetic nervous system. Stimulation of imidazoline receptors reduces peripheral sympathetic activity and blood pressure.
Moxonidine differs from other sympatholytic antihypertensive drugs in its lower affinity for α2-adrenergic receptors, which explains the lower likelihood of developing sedation and dryness of the oral mucosa.
Taking moxonidine leads to a decrease in systemic vascular resistance and blood pressure.
Moxonidine improves the insulin sensitivity index in patients with obesity, insulin resistance and moderate arterial hypertension.
Pharmacokinetics
Suction
After oral administration, moxonidine is rapidly and almost completely absorbed from the upper gastrointestinal tract. Absolute bioavailability is approximately 88%. The time to reach Cmax is about 1 hour. Food intake does not affect the pharmacokinetics of the drug.
Distribution
Plasma protein binding is 7.2%.
Metabolism
The main metabolite is dehydrogenated moxonidine. The pharmacodynamic activity of dehydrogenated moxonidine is about 10% compared to moxonidine.
Removal
T1/2 of moxonidine and metabolite is 2.5 and 5 hours, respectively. Within 24 hours, over 90% of moxonidine is excreted by the kidneys (about 78% unchanged and 13% as dehydromoxonidine, other metabolites in the urine do not exceed 8% of the dose taken). Less than 1% of the dose is excreted through the intestines.
Pharmacokinetics in special groups of patients
Clinically insignificant changes in the pharmacokinetic parameters of moxonidine were noted in elderly patients, probably due to a decrease in the intensity of its metabolism and/or slightly higher bioavailability.
Moxonidine is not recommended for use in patients under 18 years of age, and therefore pharmacokinetic studies have not been conducted in this group.
Moxonidine excretion is significantly correlated with CC. In patients with moderate renal failure (creatinine clearance in the range of 30-60 ml/min), steady-state plasma concentrations and final T1/2 are approximately 2 and 1.5 times higher than in patients with normal renal function (creatinine clearance more than 90 ml/min). min). In patients with severe renal failure (creatinine clearance less than 30 ml/min), steady-state plasma concentrations and final T1/2 are 3 times higher than in patients with normal renal function. The administration of multiple doses of moxonidine leads to predictable accumulation in the body of patients with moderate and severe renal failure. In patients with end-stage renal failure (creatinine clearance less than 10 ml/min) on hemodialysis, steady-state plasma concentrations and final T1/2 are 6 and 4 times higher, respectively, than in patients with normal renal function. In all groups, the Cmax of moxonidine in blood plasma is 1.5-2 times higher. In patients with impaired renal function, the dosage should be adjusted individually. Moxonidine is excreted to a small extent during hemodialysis.
Indications: arterial hypertension. ICD-10 codes
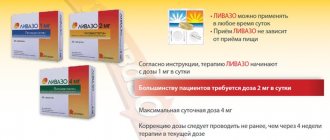
Dosage regimen
Inside, regardless of food intake.
In most cases, the initial dose of Moxarel® is 200 mcg/day. The maximum single dose is 400 mcg. The maximum daily dose, which should be divided into 2 doses, is 600 mcg.
The starting dose for patients with moderate or severe renal impairment, as well as for patients on hemodialysis, is 200 mcg/day. If necessary and if well tolerated, the daily dose can be increased to 400 mcg.
Side effect
The incidence of side effects listed below was determined according to the following: very often (≥10%), often (≥1%, but <.10%), infrequently (≥0.1%, but <.1%), rarely (≥ 0.01 %, but <.0.1%), very rare (<.0.01%, including isolated cases).
From the side of the central nervous system: often - headache, dizziness (vertigo), drowsiness, infrequently - fainting.
Mental disorders: often - insomnia, infrequently - nervousness.
From the organ of hearing and labyrinthine disorders: infrequently - ringing in the ears.
From the cardiovascular system: infrequently - marked decrease in blood pressure, orthostatic hypotension, bradycardia.
From the gastrointestinal tract: very often - dryness of the oral mucosa, often - nausea, diarrhea, vomiting, dyspepsia.
From the skin and subcutaneous tissues: often - skin rash, itching, infrequently - angioedema.
From the musculoskeletal system and connective tissue: often - back pain, infrequently - pain in the neck.
General disorders and disorders at the injection site: often - asthenia, infrequently - peripheral edema.
Contraindications for use
- severe heart rhythm disturbances,
- SSSU,
- AV block II and III degrees,
— severe bradycardia (heart rate less than 50 beats/min),
— acute and chronic heart failure (III-IV functional class according to the NYHA classification),
- simultaneous use with tricyclic antidepressants,
- severe renal failure (creatinine clearance less than 30 ml/min), including patients on hemodialysis,
- age over 75 years,
- age under 18 years (the effectiveness and safety of moxonidine have not been established),
- lactation period (breastfeeding),
- lactose intolerance, lactase deficiency, glucose-galactose malabsorption,
- hypersensitivity to the active substance or other components of the drug.
Carefully
- renal dysfunction (creatinine clearance more than 30 ml/min),
- severe liver failure (more than 9 points according to the Child-Pugh classification),
— AV block of the first degree,
- severe diseases of the coronary vessels,
- severe ischemic heart disease or unstable angina (insufficient experience with use),
- chronic heart failure.
Use during pregnancy and breastfeeding
There are no clinical data on the treatment of pregnant women with Moxarel®.
Moxarel® should be prescribed with caution during pregnancy only after a careful assessment of the risk-benefit ratio, when the benefit to the mother outweighs the potential risk to the fetus.
Moxonidine passes into breast milk. Breastfeeding women are advised to stop breastfeeding or discontinue the drug during treatment.
Use for liver dysfunction
With caution in severe liver failure (more than 9 points according to the Child-Pugh classification).
Use for renal impairment
Contraindicated in severe renal failure (creatinine clearance less than 30 ml/min), including patients on hemodialysis.
With caution in case of impaired renal function (creatinine clearance more than 30 ml/min).
Use in children Contraindicated in patients under 18 years of age, since the effectiveness and safety of moxonidine have not been established.
Use in elderly patients Contraindicated in patients over 75 years of age
special instructions
There is currently no evidence that stopping Moxarel® leads to an increase in blood pressure. However, it is not recommended to stop taking Moxarel® suddenly; instead, you should gradually reduce the dose of the drug over two weeks.
If it is necessary to cancel concomitantly taken beta-blockers and the drug Moxarel®, first cancel the beta-blockers, and only after a few days moxonidine.
During treatment, regular monitoring of blood pressure, heart rate and ECG registration is necessary. You should stop taking Moxarel® gradually.
During treatment with Moxarel®, alcohol consumption should be avoided.
Impact on the ability to drive vehicles and operate machinery
The effect of Moxarel® on the ability to drive vehicles or operate machinery has not been studied. However, given the possible occurrence of dizziness and drowsiness, patients should be careful when engaging in potentially hazardous activities that require increased attention, such as driving a vehicle or operating equipment that requires increased concentration.
Overdose
Symptoms: headache, sedation, drowsiness, marked decrease in blood pressure, dizziness, increased fatigue, asthenia, bradycardia, dry oral mucosa, vomiting and pain in the epigastric region, respiratory depression, impaired consciousness. A short-term increase in blood pressure, tachycardia, and hyperglycemia are also potentially possible.
Treatment: There is no specific antidote. In case of a pronounced decrease in blood pressure, it is recommended to administer fluid to restore blood volume and dopamine. Bradycardia can be relieved with atropine. α-Adrenergic antagonists may reduce or eliminate the paradoxical hypertensive effects of moxonidine overdose. In severe cases of overdose, it is recommended to carefully monitor disturbances of consciousness and avoid respiratory depression. Moxonidine is excreted to a small extent during hemodialysis.
Drug interactions
The combined use of moxonidine with other antihypertensive drugs leads to an additive effect.
Tricyclic antidepressants may reduce the effectiveness of centrally acting antihypertensive drugs, and therefore their use together with moxonidine is not recommended.
Moxonidine may enhance the effect of tricyclic antidepressants, tranquilizers, ethanol, sedatives and hypnotics.
Moxonidine may moderately improve impaired cognitive function in patients receiving lorazepam.
Prescribing moxonidine together with benzodiazepine derivatives may be accompanied by an increase in the sedative effect of the latter.
The simultaneous use of moxonidine with beta-blockers leads to increased bradycardia, the severity of ino- and dromotropic effects.
When moxonidine is prescribed together with moclobemide, there is no pharmacodynamic interaction.
Moxonidine is released by tubular secretion, so its interaction with other drugs released by tubular secretion is possible.
Storage conditions and periods
The drug should be stored in a place protected from light, out of reach of children, at a temperature not exceeding 25°C. Shelf life: 3 years.
Conditions for dispensing from pharmacies The drug is dispensed with a prescription.