Local therapist
Burnatskaya
Svetlana Nikolaevna
33 years of experience
Local therapist, occupational pathologist. Member of the Russian Scientific Medical Society of Therapists
Make an appointment
Dyspnea is the name given to visible disturbances in the depth and frequency of breathing in a person, accompanied by an obsessive feeling of lack of air. Shortness of breath can be observed after intense physical activity or in a state of absolute rest. In what cases is this the norm, and in what cases is it an alarming signal of a health threat?
Types of shortness of breath
In medicine, this problem has its own name - dyspnea. According to the international classification, the following types of shortness of breath are distinguished:
- bradypnea;
- tachypnea.
Bradypnea is a decrease in breathing with a slowdown in respiratory rate to 12 or less movements per minute. Tachypnea is an increase in shallow breathing with a frequency of more than 20 movements per minute.
Based on intensity and time interval, dyspnea is divided into types:
- chronic – observed for several years;
- acute – lasts from 2 minutes to several hours;
- subacute – from several hours to 2 days.
Most often, shortness of breath is observed in diseases of the respiratory (bronchopulmonary) and cardiovascular systems. These diseases are extremely life-threatening. Therefore, if you suspect shortness of breath, you should immediately consult a doctor to undergo examination and receive timely treatment.
Causes of shortness of breath
There can be quite a few reasons for shortness of breath. Among them:
- strong physical activity (sports, work);
- myocardial infarction, irregular heart rhythms, heart defects, myxomas, other heart problems;
- allergies, bronchial asthma, tuberculosis, emphysema, pneumothorax, pneumonia, pulmonary obstruction, cancer;
- vasculitis, primary type hypertension, aneurysm;
- myasthenia gravis, lateral sclerosis;
- ascites;
- uremia;
- anemia;
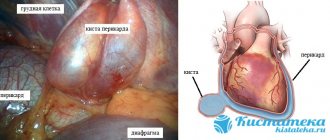
- pericardium;
- hyperventilation syndrome.
Psychogenic asthma
In general, bronchial asthma refers to a pathology of the respiratory system. Its development is associated with changes in the structure of the bronchi against the background of immune failures, that is, it is a very specific disease, the etiology of which is not related to mental factors.
People suffering from this disease may develop a condition called psychogenic asthma. This happens when attacks of suffocation, the main symptom of the disease, are provoked by nervous overstrain, both positive and negative, whereas in normal cases this occurs under the influence of cold, infections or physical exertion.
Under the influence of super-emotions, histamine is released. This is one of the main mediators of inflammation. It causes bronchospasm. The result is a dry cough, shortness of breath and an attack of suffocation.
Psychogenic asthma often develops in women during the menstrual period and in children, whose psyche is still quite unstable and very sensitive.
Symptoms
Symptoms of shortness of breath can be very different, but they are always characterized by changes and disturbances in respiratory activity. A person can breathe very quickly and shallowly, or he can take rare and very deep breaths. In both situations, he experiences an acute lack of air, a feeling of suffocation and chest compression.
With inspiratory dyspnea, it is difficult for the patient to take a breath. At the same time, he hears noise while trying to draw oxygen into his lungs. In the case of expiratory dyspnea, it is difficult to exhale, as the lumens of the bronchioles and bronchi begin to narrow.
In medical practice, there are cases of mixed dyspnea, the condition of which is the most dangerous for the body. It can lead to complete respiratory arrest and death.
Are you experiencing symptoms of shortness of breath?
Only a doctor can accurately diagnose the disease. Don't delay your consultation - call
What is the connection between COVID-19 and shortness of breath?
— Coronavirus has a wide range of negative effects on the entire human body: it is not the same pneumococcus (the main causative agent of community-acquired pneumonia), which primarily affects the respiratory tract and from which the body only indirectly suffers.
The causative agent of COVID-19 can affect not only the lungs, but also all organs; in many patients, blood clotting noticeably increases (therefore, patients are often prescribed drugs from the group of anticoagulants - drugs to improve blood flow that prevent the formation of blood clots in all vessels, including including in the vessels of the lungs). On the one hand, the virus affects the respiratory system
. With coronavirus, the volume of the respiratory surface in the lungs may decrease, and the system of conduction tracts does not remain unchanged. The bronchi also suffer: in this respect, COVID-19 is similar to the influenza virus, which often causes tracheitis.
On the other hand, it can affect the cardiovascular system ,
as well as the central and peripheral nervous systems, which, among other things, may be associated with stress and a changed lifestyle. Coronavirus disrupts the regulation of processes in the nervous system, which may result in a feeling of lack of air, “laziness” of the respiratory center, and impaired patency of those nerves that give a signal for respiratory movements. It has been revealed that this virus is capable of infecting brain tissue such as thrombovasculitis and specific viral encephalitis, the manifestations of which may include a feeling of lack of air.
All these factors can affect the respiratory tract - and not only during the period of time when a person is sick. Doctors around the world are talking about “post-Covid syndrome”
, that is, about the long-term presence of symptoms (including shortness of breath) in people who have suffered the acute phase of coronavirus infection. In December 2021, at the initiative of Russian therapists, additional codes were even added to the International Classification of Diseases, Tenth Revision (ICD-10) to designate post-Covid syndrome.
Diagnostics
Diagnosis of shortness of breath comes down primarily to assessing the general condition of the patient and collecting an anamnesis. Based on the current clinical picture, additional studies are prescribed:
- chest x-ray;
- MRI;
- urine and blood tests;
- Ultrasound of the heart;
- ECG;
- spirometry;
- Ultrasound of the neck.
The exact list of necessary diagnostic measures is prescribed by the doctor after consultation with the patient.
Treatment of shortness of breath
Treatment for shortness of breath is selected depending on what root of the problem is discovered after diagnosis.
- If a foreign body is detected in the respiratory organs, surgical intervention is performed.
- For bronchial asthma, selective beta-agonists are used.
- For heart failure, diuretics, narcotic analgesics, and vasodilators are prescribed.
- If the cause is neurology, then the emphasis is on special breathing exercises.
- For obstructions, anxiolytics, respiratory support, oxygen administration and other measures are prescribed.
How to treat shortness of breath after coronavirus
When helping people who have difficulty taking deep breaths, doctors use:
- drug therapy;
- oxygenation;
- inhalation;
- physiotherapy;
- breathing exercises.
Let's look at each method in more detail.
Medicines for shortness of breath
To improve pulmonary function, doctors prescribe drugs belonging to such pharmacological groups as:
- antiviral;
- immunomodulators;
- bronchodilators;
- expectorants;
- thinning phlegm;
- antibiotics.
Drugs and their dosages are always selected individually, taking into account the severity of the symptoms of the disease and the patient’s health status.
Oxygenation
It is inhaled oxygen therapy. Used if a person is unable to breathe on their own. Then oxygen is introduced directly into the respiratory tract through a special catheter.
Oxygenation is required only for seriously ill patients. If a person controls his condition and follows all medical prescriptions, the risk of sudden suffocation will be minimal.
Inhalations
During inhalation, a nebulizer is used, breaking the medicinal solution into tiny particles that easily penetrate into the deep tissues of the lungs. A good effect can be achieved by:
- agents that thin viscous sputum;
- antiseptics;
- sea water;
- saline solution;
- bronchodilators;
- coughing
Inhalations should not be carried out unless prescribed by a doctor, since if the inhaled drug is selected incorrectly, lung function may deteriorate.
Physiotherapeutic procedures
To speed up the resorption of inflammatory foci and abnormal compactions, during and after coronavirus, you need to do the following:
- massage of the chest area;
- UHF therapy;
- electrophoresis with enzyme solutions;
- SMT.
It is important to follow the physiotherapy course to the very end. If you abandon the procedures immediately after you feel better, the negative symptoms will most likely return again.
Breathing exercises
You should do breathing exercises during illness and for at least one month after receiving a negative test for COVID-19. They activate the muscles of the chest and increase blood flow to the lung tissues.
If a patient suffers from severe shortness of breath, the doctor may recommend using a respirometer, a device that measures the intensity in cells and tissues.
Preventing shortness of breath
Since shortness of breath is not an independent disease, but only a symptom, you must first take care of your heart and lungs. For this purpose, the following are recommended as preventive measures:
- stop smoking and drinking alcohol;
- monitor the daily routine (ensure a balance of work and rest, sound, standardized sleep);
- exclude heavy, fatty foods, fast food, carbonated and alcoholic drinks;
- reduce excessive physical activity;
- protect your nervous system from stress and anxiety.
FAQ
Which doctor should you contact if you notice signs of shortness of breath?
First of all, you need to make an appointment with a therapist. He will issue directions for primary tests and diagnostic studies. Based on the results obtained, it will become clear which specialist to refer the patient to. Most often, further treatment is carried out by cardiologists, pulmonologists and neurologists.
Can pregnant women experience shortness of breath? Is it dangerous for the fetus and mother?
Shortness of breath during pregnancy is observed quite often. This is due to constriction of the lungs by the diaphragm. The fetus is constantly growing, the load on the heart and lungs increases. Therefore, shortness of breath should not be considered a danger in this case. The normal respiratory rate in pregnant women is 22-24.
How to deal with systematic shortness of breath?
Of course, you need to understand the reasons for its appearance in the first place. If shortness of breath is not associated with serious illnesses, but is only a consequence of physical weakness of the body (perhaps after an injury or a long-term serious illness), then evening walks in the fresh air will help. You can get a dog, which will become an additional incentive for physical activity and walks.
Is shortness of breath at rest the most dangerous?
— When assessing the degree of respiratory failure, pulmonologists really pay attention to shortness of breath at rest. It ranks last in many scales of dyspnea severity. the mMRC dyspnea severity scale is popular in world practice .
this is what it looks like:
| Degree | Heaviness | Description |
| 0 | No | Shortness of breath occurs only during heavy physical activity. |
| 1 | Lightweight | Shortness of breath occurs when walking quickly on level ground or when climbing a small hill. |
| 3 | Average | Due to shortness of breath, patients walk slower than their peers, or when walking at their own pace on level ground, they must stop to catch their breath. |
| 4 | Heavy | After walking about 100 m or several minutes on level ground, the patient must stop to catch his breath. |
| 5 | Very heavy | Shortness of breath does not allow the patient to leave the house and appears when dressing or undressing. |
This scale is associated with a decrease in exercise intolerance and it shows that shortness of breath, which deprives a person of the ability to perform usual activities, is indeed the most severe.