Migraine
is a chronic disease that manifests itself in the form of sudden attacks of severe headache, often accompanied by nausea and, in some cases, vomiting. Photophobia and sound intolerance may also occur before and during attacks.
Migraine is a neurological disease. It is associated with disturbances in the activity of brain structures responsible for pain and other sensations. Migraine attacks can last from several hours to 3 days. The frequency of attacks also varies: from once or twice a year to 2-8 times a month, in some cases more often.
Migraine can be considered a widespread disease - one in seven adults suffers from migraine. Migraines occur three times more often in women than in men.
Manifestations of migraine are more typical for young or mature people. Usually the disease appears at the age of 18-33 years, less often - at an older age, after 50 years - extremely rarely. Cases of the disease have been reported in children over 5 years of age. After 60 years, the severity and frequency of attacks disappear, the disease, as they say, “goes away.”
general information
According to statistics, at least every tenth person on the planet suffers from migraine.
Women get sick approximately twice as often as men. This is associated with cyclical hormonal changes during the menstrual cycle. Typically, the disease makes itself felt before the age of 30-35; cases of the pathology occurring in childhood have also been described.
The biomechanism of the development of the disease is not precisely known. There are several theories about the occurrence of pain and accompanying symptoms, the most popular of which is neurovascular. According to this point of view, migraine begins against the background of activation of the trigeminal nucleus, which first causes spasm and then dilation of cerebral vessels. As a result, the tissue around the arteries becomes swollen, which leads to pain. In addition, the pathological process is associated with impaired serotonin metabolism.
Some scientists believe that pain occurs solely against the background of a sharp spasm and subsequent relaxation of blood vessels, resulting in tissue swelling (vascular theory). It has been clearly proven that the risk of developing the disease is significantly higher in women, as well as in people whose parents or close relatives also suffered from migraine.
Make an appointment
Why does migraine occur?
Neurology describes more than two hundred types of headaches of various origins. Broadly speaking, they are divided into two groups. Primary cephalgia is not associated with any diseases, secondary ones are symptomatic.
Migraine is a primary headache. It is considered a neurovascular syndrome and has long been thought to result from irritation or compression of the neurovascular bundle. But now the disease is associated with increased excitability of certain groups of nerve cells in the brain. Research shows that these neurons have unstable biochemical activity and electrical excitability. Therefore, under the influence of several trigger factors, they are activated and transmit excitation to neighboring cells, forming a focus. The mechanism of propagation of an electrical impulse is similar to an epileptic attack, but this is a completely different disease.
The causes of migraine can be:
- genetic predisposition;
- endocrine disorders;
- stress and sleep disorders;
- poor nutrition;
- weather sensitivity.
In women, the manifestation of primary cephalgia is associated with changes in hormonal levels. Thus, when estrogen levels decrease, migraine episodes become more frequent, and when estrogen levels increase, they disappear. The first attacks may coincide with the first menstruation, but often begin after 30 years. Migraine usually disappears after pregnancy, it practically does not occur in the 2nd and 3rd trimesters.
Certain foods can act as triggers. Each person will have an individual list of them, but most often the connection is traced with the consumption of chocolate, cocoa, coffee, alcohol, strong tea, red wine, beer, legumes or cheese. Therefore, if such a connection is established, it is better to exclude the product from the diet.
Sometimes attacks occur after head and neck injuries, which may be due to a disruption in the blood supply to a certain area of the brain. Mandibular joint dysfunction can also lead to chronic migraines.
In children, attacks occur due to mental or physical fatigue; they can appear after a change of team or place of residence, or other stressful situations.
Causes
Migraine occurs against the background of various external and internal causes (triggers), each of which can cause another attack:
- mental and psycho-emotional stress;
- constant severe stress;
- sleep disturbances, insufficient rest at night;
- chronic fatigue (mental and physical);
- smoking;
- previous head injuries (even many years ago);
- excessive physical activity for a particular person;
- hormonal surges: puberty, menstruation (“menstrual migraine”), pregnancy;
- consumption of foods containing tyramine (chocolate, coffee, citrus fruits, nuts, cheese, smoked meats);
- drinking alcohol, especially low-alcohol drinks;
- sharp fluctuations in atmospheric pressure, changes in air temperature;
- overstrain of the senses: sharp sound, bright light, strong unpleasant odor, etc.;
- staying in a hot or stuffy room, etc.
Each person has his own “dangerous” factors. Most of them can be calculated and, if possible, avoided in the future.
Symptoms
A migraine attack follows a standard scenario, consisting of several successive stages.
- Prodromal (initial) stage. A person’s mood begins to change, yawning and drowsiness appear, or, conversely, insomnia. Some report sensitivity to noise and bright light. Sometimes there is a slight numbness in one of the hands. For most patients, these symptoms are enough to know that a full-blown migraine attack is on the way. The duration of the prodromal stage ranges from several hours to several days; it is not present in all patients.
- Aura. Occurs against the background of cerebral vascular spasms. Most often it manifests itself in the form of visual disturbances (flashes in the form of spots, zigzags or lightning in front of the eyes, distortion of the contours of objects, loss of individual fields of vision). Less common are taste or hearing disorders, problems with coordination of movements, etc. Aura is not observed in all patients.
- Actually a migraine attack. In most cases, it manifests itself as a unilateral headache that is pulsating in nature. It starts with slight discomfort and gradually gains strength, becoming simply unbearable. Movements, changes in body position, bright lights and loud sounds intensify the sensations, which is why patients try to spend this time lying in a darkened room. Against the background of a headache, many patients report nausea, vomiting, soreness in the muscles of the neck and shoulders, nasal congestion, lacrimation, chills and even fever. The duration of the attack is individual and ranges from 2-3 hours to several days.
- Resolution stage. At this time, the headache goes away on its own or after taking medications. Many patients fall asleep at first, but within 24 hours after the attack they may feel weak, lethargic, dizzy, and depressed. Increased sensitivity to light, sounds and smells also does not go away immediately. Less common is the opposite type of resolution stage, in which patients note increased activity.
What is migraine
Migraine is a neurological disorder characterized by unilateral headaches. In some cases, it is accompanied by a set of concomitant vegetative symptoms. Because of them, migraine can be confused with other diseases.
The disease occurs more often in women and can be hereditary. There is a rare type of hemiplegic migraine that is associated with changes in genes on chromosomes 1, 2, and 19. But the role of these pieces of genetic material in the formation of common migraines is still being studied.
Not every headache fits the definition of a migraine. Usually the pathology occurs unilaterally, and the intensity of pain varies. The first signs appear on average at the age of 30 and gradually progress. But there have been rare cases of migraine headaches appearing in children as young as 3 years old. Moreover, boys suffer from migraines more often than girls. And with age, this ratio changes in favor of women.
The exact causes of the pathology are unknown, but it is considered a multifactorial disease. The peculiarity of the course of the pathology is that in women, as menopause approaches, the condition may worsen. But after menopause it stabilizes and the symptoms gradually disappear.
Types of pathology
Migraines are most often classified according to the presence of an aura and its type. The following types of disease are distinguished:
- classic migraine: before an attack of pain, a typical aura occurs with visual, auditory, olfactory and other disturbances;
- migraine without aura: symptoms appear suddenly against a background of relative well-being; the rest of the clinical picture is characteristic of the disease.
Depending on the predominant symptoms, the following types of migraine are distinguished:
- ocular (ophthalmic): accompanied by classic visual impairments: glare, flickering, flare in certain areas of the visual field;
- retinal: the disease manifests itself as complete or partial loss of vision in one eye due to impaired blood circulation in the vessels of the retina;
- ophthalmoplegic: manifested by double vision, visual distortions, drooping of the eyelid;
- basilar: accompanied by dizziness, ringing in the ears, unsteadiness when walking, blurred speech;
- hemiplegic: characterized by loss of sensation and impairment of motor function of one arm or arm and leg on one side;
- cervical: occurs against the background of impaired blood flow in the vertebral arteries and is accompanied by a very severe headache;
- aphasic: pain is accompanied by speech disorders, as with a stroke;
- abdominal: additionally manifests itself as severe pain throughout the abdomen, diarrhea, nausea and vomiting; this form is very common in children;
- “decapitated”: the patient does not feel a headache, as a rule, only visual disturbances are noted, while the prodromal period and aura occur typically.
Migraine status stands apart. This is a severe condition in which two or more attacks occur in a row with less than 4 hours between them. This type also includes pain that lasts for more than 3 days. Against the background of migraine status, the patient experiences repeated vomiting, which does not allow him to eat, drink, or take medications normally.
Do I have migraines?
A neurologist can determine this with accuracy. Therefore, we recommend consulting with a specialist if you are experiencing a similar problem. To get your bearings, you can use the IHS – International Headache Society questionnaire. You only need to answer 5 simple questions:
- Does nausea or vomiting occur along with the headache?
- Does the headache last from 4 to 72 hours?
- Does the pain throb?
- Does only one side of your head hurt?
- Does pain interfere with the usual flow of life?
If you answered “yes” to 3 questions, then the probability that it is a migraine is 90%. If the answer to 4 questions is positive, the probability is 100%.
Diagnostics
The patient's headache has characteristic features that immediately suggest a migraine. For diagnosis, the doctor uses the following methods:
- collecting complaints and medical history to determine the nature of the pain; special attention is paid to: the time of onset and end of the attack;
- provoking factors;
- nature of pain;
- the absence or presence of an aura, its symptoms;
- well-being after an attack;
If necessary, additional examinations and consultations with specialists are prescribed. The diagnosis of migraine is made by exclusion when no other causes of headache have been identified.
Make an appointment
Educational video “Headache and migraine”
1 - Frick et al. Efficacy and safety of naproxen sodium and ibuprofen for pain relief after oral surgery. Current Therapeutic Research. 1993;54(6):619-27. 2 — https://www.ncbi.nlm.nih.gov/pubmed 3 — Karateev AE. Naproxen: a versatile analgesic with minimal risk of cardiovascular complications. Modern rheumatology. 2016;10(2):70–77. 4 - in oral form. Based on these instructions for use and clinical studies of over-the-counter painkillers registered in the Russian Federation.
Treatment
Migraine treatment is divided into two areas:
- relief of the patient’s condition during an attack;
- preventing the occurrence of new attacks.
Help during a seizure
At the first signs of an impending migraine attack, it is necessary to eliminate as quickly as possible all factors that can increase the pain:
- turn off the lights and TV, close the curtains;
- eliminate sources of extraneous sounds as much as possible;
- provide access to fresh, cool air;
- go to bed.
To prevent and relieve immediate pain attacks, painkillers of various groups are used:
- analgesics and non-steroidal anti-inflammatory drugs (analgin, ibuprofen, indomethacin and their analogs): used for mild attacks that do not affect a person’s daily life;
- combination drugs (codeine, tempalgin, solpadeine): prescribed for moderate attacks that have little effect on life activity;
- triptan drugs (amigrenin, sumamigren, zomig and others) are used if attacks interfere with normal life;
- hormonal drugs (dexamethasone): used for severe and prolonged migraines in combination with other medications.
Additionally, antiemetics (metoclopramide, cerucal) can be used.
Home remedies to prevent a migraine attack are used as an addition to the main therapy. Many patients benefit from:
- cold compress on forehead;
- rubbing essential oils into the temple area;
- infusion of chamomile, mint, lemon balm, lavender and other herbs that promote relaxation;
- acupressure on acupuncture points: at the base of the skull, between the eyebrows in the hollow above the bridge of the nose, on the back of the foot (the hollow between the first and second toes).
It is important to remember that these remedies do not replace primary therapy.
Treatment between attacks
Preventing the occurrence of attacks is no less important than relieving pain and nausea. Currently, various groups of drugs are used:
- beta-blockers (propranolol and drugs based on it);
- antidepressants (venlafaxine, milnacipran, etc.): have a good effect in the treatment of chronic pain, and also reduce the manifestations of depression characteristic of patients with frequent attacks;
- anticonvulsants (Depakine, topiramate): well tolerated and significantly reduce the frequency of exacerbations.
Medicines are used:
- if exacerbations occur more than 2 times a month;
- if attacks last more than 48 hours;
- with severe headache or complications.
In other cases, general preventive measures are sufficient.
Modern approaches to the treatment of migraine
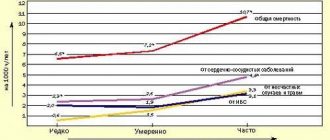
Migraine is a common disorder, occurring in 6% of men and 18% of women (Rasmussen BK et al., 1991). Despite the fact that migraine therapy is well developed (according to the American Headache Association, the effectiveness of correct treatment can reach 95%), more than 70% of patients are not satisfied with the result of treatment (Lipton RB, Stewart WF, Simon D., 1998). This is partly the fault of the patients themselves, who do not see a doctor, self-medicate, and ignore the recommendations they receive. However, in many cases, the low effectiveness of therapy is the result of inadequate medical care. Some doctors continue to manage patients with migraine based on outdated information, without considering the possibilities of modern migraine treatments. However, the difficulty of treating headaches is not only due to the “correct” choice of medication. Migraine is a complex neurobiological disorder with a multifactorial pathogenesis, and the problem of its treatment cannot be solved with the help of any one drug, even a new and effective one. To achieve success, it is necessary to take into account a number of aspects, both purely medical and psychological.
In the treatment of migraine, three tasks can be distinguished - prevention of attacks, their treatment and prevention.
- Preventing migraine attacks . By teaching the patient to identify warning signs, identify migraine triggers, and avoid situations that provoke migraine, it is possible to prevent or significantly reduce the number of attacks without the use of drugs.
- Treatment of seizures . Many patients suffering from migraine are maladjusted by the fear associated with anticipating an attack. In this regard, it is very important to work together with the patient on treatment tactics for various scenarios of migraine development.
- Preventive treatment of migraine . If migraine attacks are frequent (more than 2 times a week) and/or if behavioral and pharmacological measures are ineffective, it is necessary to consider preventive treatment. Some specific forms of migraine are also indicated for preventive treatment: hemiplegic migraine or migraine with aura with persistent neurological deficit.
Preventing migraine attacks
The success of treatment largely depends on the doctor’s ability to teach the patient to recognize triggers and avoid situations that provoke migraines. According to our study, when first told, the connection between the onset of a headache and some factors is noted by about 30% of patients visiting a doctor (Danilov A. B., 2007). With careful questioning using a special questionnaire that lists all possible headache triggers, the frequency of identifying such factors increases to 85%.
The difficulty of detecting provoking factors may be explained by the fact that some of them never cause a migraine attack in some patients, while in others they do, but not always. For example, many patients sensitive to alcohol notice that if they are in a good mood, relaxed, and following a low-carb diet, then a moderate amount of white wine does not lead to negative consequences. If these patients are tense and eat a lot of sweets, then the same wine can cause them a severe migraine attack. When the presence of migraine triggers is not obvious, it is useful to use a headache diary, which helps to recognize the factors that provoke the development of migraines.
In a study conducted at our department, it was shown that in some patients a migraine attack did not occur at the height of emotional stress, but at the end of a stressful situation: after an important speech, after signing a complex contract, at the beginning of a vacation (“weekend migraine”), after receiving a promotion, etc. Chronic stress (family conflicts, work overload) contributed to an increase not only in the frequency of attacks, but also in the intensity of headaches. At the same time, the strength of the provoking factor depended on the significance that the patient attached to the events in accordance with his attitudes and coping strategies - the situation became/did not become “stressful” depending on the patient’s individual reaction to it. It was noted that men were more likely to attach importance to problems related to professional activities, and women were more concerned about their social relationships at work and at home (Danilov, 2007).
In susceptible individuals, foods may cause headaches. Most often, such triggers are meat (pork, game), as well as animal organs (liver, kidneys, goiter, brains), sausages and frankfurters, herring, caviar and smoked fish, vinegar, salted and pickled foods, some types of cheese (cheddar, "brie"), products containing yeast (especially fresh bread), chocolate, sugar and products containing it, citrus fruits (if consumed in large quantities), cream, yoghurt, sour cream, legumes, flavor enhancers such as monosodium glutamate, caffeine ( black tea, coffee), alcohol, especially red wine. It should also be taken into account that the development of a migraine attack can also be triggered by skipping meals.
Other migraine triggers are strong odors (even pleasant ones, such as perfumes, cigar smoke), vestibular stress, bright light, noise, and smoking. In women, in addition, the development of headaches can be triggered by certain days of the menstrual cycle or the start of taking oral contraceptives.
Physical activity can also be a migraine trigger. According to our study, 7% of women and 21% of men associate headaches with physical activity. Migraine attacks can be provoked by exhausting physical exercise (for women - fitness, dancing, for men - running, football, fitness). Playing sports without physical exhaustion does not lead to headaches (Danilov, 2007).
In 10% of cases, migraine attacks occur during sexual intercourse (Evans RW, 2001). The cause of headaches that develop during sexual activity may not be migraine, but secondary dangerous disorders - aortic aneurysm and others, so in this case it is advisable to undergo a thorough examination. Fortunately, secondary headaches are rare. However, sexual activity may also help reduce or even stop a migraine attack. In a study by Couch JR and Bearss C. (1990), which involved 82 women suffering from migraine, having sex at the onset of a migraine reduced the severity of headaches and other symptoms in every third patient, and in 12% of women, sex completely stopped the attack. The effect was more pronounced in those women who experienced orgasm. The authors explain the observed phenomenon by the influence of antinociceptive opiate systems, which are activated during sex and help reduce or stop headaches.
A number of migraine triggers, such as weather changes and certain days of the menstrual cycle, cannot be avoided. In these cases, it is important to simply be aware of the possible threat of migraine development and be prepared for the onset of an attack. Most other triggers can be controlled and should be disclosed to the patient. Thus, for many patients it may be an unexpected discovery that a migraine attack can be provoked not only by insufficient sleep and overwork, but also by excess sleep, a situation of recovery from a period of stress, overload.
Currently, many devices are offered to reduce or avoid the influence of migraine triggers, for example, special sunglasses, fluorescent lamps instead of “yellow” ones, earplugs, eye masks, and special pillows. It is also important to be able to relax. There are special techniques that help you relax and prevent the development of headaches in cases where you could not avoid a stressful situation.
Treatment of attacks
Behavioral interventions
Preparing for a possible attack. An important factor contributing to the success of treatment is achieving a sense of control over the headache: the pain can be exacerbated by the anxiety that grips the patient in anticipation of a new attack, and the feeling of helplessness that arises if the patient does not know how to cope with the attack. When the trigger or precipitating situation cannot be prevented, or when the patient fails to follow the doctor's instructions, it is important to teach the patient what to do if the development of a headache is unavoidable.
First of all, it is necessary to help the patient learn to recognize the onset of a migraine. Many patients (usually with many years of migraine experience) accurately distinguish migraine from other types of headaches. For others, the doctor’s explanations about the characteristics of migraine attacks (presence of precursors, aura, impaired concentration, nausea, etc.) will be very valuable. The education of the patient in this case is of direct importance in the choice of medications to relieve the attack. If a migraine of moderate or severe intensity is expected, then the best treatment in this situation will most likely be a drug from the triptan group. If the development of a mild headache is expected or the patient feels that in this case he is developing an episode of tension-type headache, then in this situation it is advisable to use a conventional analgesic or a drug from the group of non-steroidal anti-inflammatory drugs (NSAIDs).
It is important to select a drug in advance to relieve an attack, taking into account previous experience with the use of drugs (efficacy, presence of adverse reactions), the patient’s preferences and expectations, and the severity of the expected attack. The tactic of “waiting” is now recognized as incorrect. Migraine attacks can last up to 72 hours, and the longer it takes for migraine symptoms to appear, the worse the response to treatment. If you take the medicine as early as possible after the first signs of migraine appear, you can often completely prevent or significantly reduce the intensity and duration of the headache and quickly return to social or work activity.
Providing conditions for a comfortable experience of an attack . A number of behavioral interventions can enhance the effectiveness of medications. If a migraine attack begins, it is advisable to stop exposure to irritating stimuli (bright lights, loud speech, working at a computer monitor, activities requiring physical or mental stress). Understanding others is very important here. It makes sense for the patient to warn his family or colleagues and superiors in advance that he has migraine attacks, which can prevent him from working for 24 hours or more. They should be told that if the patient is given the opportunity to stop working, take medication and sit in silence, this will greatly increase the likelihood that after 2 hours he will be able to return to normal activities, successfully coping with the attack.
Drug therapy
To date, many methods have been developed for the treatment of migraines, ranging from tea from wild rosemary branches to triptan drugs. What is the best treatment? The best treatment will be one that is tailored to the individual needs of a particular patient.
Until recently, a stepwise approach was adopted in the treatment of migraine, according to which it was initially proposed to use simple analgesics or drugs from the NSAID group to relieve an attack. If the effect was insufficient, we switched to combination drugs. If the tried remedies turned out to be ineffective, it was proposed to use “upper step” drugs—triptans. Thus, triptans were used only in resistant cases.
This approach has often frustrated patients who would have preferred a doctor to immediately prescribe an effective drug. With a stepwise approach, the average patient tried about 6 drugs before finding the optimal one (Lipton RB, 2000). It should be taken into account that another failure when taking a new drug seriously undermines the patient’s faith in the possibility of success of therapy, increases anxiety, contributes to the development of depression and maladjustment, which worsens the prognosis of therapy.
The stratified approach to migraine treatment has proven to be extremely convenient for clinical use. It is based on assessing the impact of migraine on the patient’s daily activities using the MIDAS (Migraine Disability Assessment Scale). Depending on the answers to five simple questions about time lost due to headaches in three main areas of life (study and work, housework and family life, sports or social activity), the severity of migraine is determined. The MIDAS scale divides patients into 4 groups, where group I corresponds to minimal disruption of daily activities and mild headache intensity, and group IV is characterized by a severe degree of maladjustment and severe headache (Lipton RB, Stewart WF, 1998). Each group offers its own medications.
Treatment of attacks of mild intensity, which practically do not worsen the quality of life of patients. Patients in this group rarely go to the doctor, since they are helped by physical methods of dealing with pain (heat, cold), numerous “folk” methods (cabbage leaves, lemon peel, peeled, etc.). Of the pharmacological agents for rare attacks of unexpressed headache, simple analgesics (Analgin), paracetamol or drugs from the NSAID group are usually effective: ibuprofen (Ibuprofen, MIG 400, Nurofen), naproxen (Naproxen), indomethacin (Indomethacin), diclofenac (Voltaren ) etc. The choice of drug should be made depending on the patient’s preferences, taking into account past experience with drugs and the risk of gastrointestinal complications
Treatment of attacks of moderate intensity. For pain of moderate intensity, NSAIDs are indicated. More effective are combined analgesics containing codeine or caffeine (Caffetin, Solpadeine, Tetralgin, Pentalgin). These drugs can be purchased without a prescription. Many patients, unfortunately, get too carried away with them, believing that it is necessary to be careful only when using medications prescribed by a doctor. It should be remembered that over-the-counter medications, when used in excess, can lose their effectiveness and sometimes even cause an overuse headache, that is, a headache caused by excessive use of the drug.
In cases of severe maladjustment in patients with moderate headache intensity, it may be advisable to start therapy with a triptan drug. The use of triptans can reduce the number of drugs that patients take for the symptomatic treatment of migraine and prevent chronic headaches.
Treatment of high intensity attacks. If the headache intensity is high, it is recommended to immediately prescribe a drug from the triptan group. In some cases, it is advisable to use opioid analgesics. Clinical studies have demonstrated the high effectiveness of the combination drug Zaldiar, which includes the weak opioid analgesic tramadol and the analgesic and antiperetic paracetamol, for relieving migraine attacks. Thanks to this combination, it is possible to achieve high efficiency with a low number of side effects (Ekusheva E. V., Filatova E. G., 2007). Zaldiar does not belong to the group of narcotic analgesics, and any doctor can prescribe it on prescription form No. 147.
Severe headaches are often accompanied by severe nausea and vomiting. In this case, it is advisable to use antiemetics: metoclopramide (Metoclopramide, Cerucal, Ceruglan), domperidone (Domperidone, Motilak, Motilium), chlorpromazine (Chlorpromazine, Aminazine). Some experts recommend using an antiemetic 20 minutes before taking an NSAID or triptan drug. If the attack is accompanied by nausea, it is advisable to use a triptan nasal spray (Imigran) (.).
For very severe persistent migraine attacks, the use of corticosteroids (dexamethasone 8–12 mg intravenously or intramuscularly) is necessary.
Some studies have demonstrated a good effect (“on the needle” effect) of Cormagnesin for relieving migraines of moderate or severe intensity (Danilov A. B. et al., 2004). There are other medical methods for relieving migraines, for example, treatment with leeches, injections of novocaine into trigger points, etc. These methods are very effective in the hands of those specialists who have developed them or have extensive experience in their use. Unconventional approaches to the treatment of headaches can be welcomed if they are effective, but they cannot be recommended for mass use without evidence-based research.
Features of triptan drugs . The gold standard for migraine therapy is sumatriptan. The effectiveness and safety of sumatriptan was studied in 300,000 attacks (more than 60,000 patients) in clinical trials and in 200 million attacks in clinical practice over 15 years of its use. Patient satisfaction with this drug is 63% and significantly exceeds satisfaction with drugs of other classes that are used to relieve migraines (Pascual J., 2007). Sumatriptan is more effective in patients with slow onset headaches. In our country, sumatriptan is produced in the form of tablets under the trade names Amigrenin, Imigran, Sumamigren, in the form of a spray - “Imigran” and in the form of suppositories “Trimigren”. Studies of generic sumatriptan (Amigrenin, Sumamigren) conducted in our country confirmed its high effectiveness (Vein A.M., Artemenko A.R., 2002; Tabeeva G.R., Azimova Yu.E., 2007).
Naratriptan (Naramig), zolmitriptan (Zomig), eletriptan (Relpax) belong to the second generation of triptans and have greater selectivity of action compared to sumatriptan, which leads to fewer side effects and greater effectiveness in some respects. The use of these drugs is advisable when taking sumatriptan is ineffective.
The following recommendations have been developed for the use of drugs from the group of triptans to relieve a migraine attack. After the patient feels that he is developing a migraine attack of severe or moderate intensity, he should take 1 tablet of the drug (minimum dose). If the pain goes away after 2 hours, the patient can return to normal activities. If after 2 hours the pain has decreased, but has not gone away completely, it is recommended to take another dose (tablet) of the drug. Next time you can immediately take a double dose of the drug (2 tablets).
If there is no effect 2 hours after administration, the drug is considered ineffective. In this case, the question of replacing it should be raised. Some headache specialists suggest trying the drug 3 times before giving it up. Other doctors believe that a new drug should be used for the next attack. We adhere to the second point of view, i.e. if the drug was taken in a timely manner during a correctly recognized migraine attack and after 2 hours the intensity of the headache has not changed at all, then at the next attack you should take another drug (a triptan from a different group or from a different manufacturer). Note that there is marked variability in the effectiveness of the drug, including within the triptan series, depending on individual sensitivity. It is important to patiently select from the available arsenal the remedy that will be effective for a given patient.
Once an effective drug has been found, you should not experiment with others. Recommend that the patient always carry the medicine with him. There should be no fear of addiction if the drug is used no more than 2 times a week. Taking triptans more frequently can lead to side effects, including triptan overuse headache (headache caused by drug abuse). Also, do not exceed the maximum daily dose. There are contraindications to the use of triptans, such as the presence of hypertension and other cardiovascular disorders (for a complete list of contraindications, see the instructions for use). The choice of drug should be made jointly by the doctor and the patient, taking into account pharmacochemical characteristics, the presence of contraindications and individual sensitivity.
Preventive treatment of migraine
Prescribing preventive treatment is a responsible task that requires careful preliminary discussion with the patient. Preventative treatment is associated with side effects due to long-term use of medications and requires patience from the doctor and the patient. However, the lack of preventive treatment can lead to abuse of analgesics and the development of abusive headaches. Frequent migraine attacks are the basis for the occurrence of chronic migraine, as well as risk factors for vascular brain damage.
To prevent migraine, various pharmacological agents are used, including those for which the recommendations do not yet include this indication. Monotherapy is preferable; in complex cases, combination treatment is allowed, taking into account concomitant diseases. The drugs of choice are beta-blockers - propranolol (Anaprilin, Obzidan). Antidepressants and anticonvulsants, which occupy a leading position in the effectiveness of preventive treatment, still do not have this indication in the instructions for use. Of the anticonvulsants, the most effective are valproate and the new anticonvulsant topiramate. Clinical studies have shown that topiramate is effective in preventing migraine attacks, significantly reducing their frequency. Its effect develops quite quickly - during the first month of therapy there is a stable, long-term decrease in the number of attacks without the development of resistance. Compared to other anticonvulsants, topiramate has a favorable tolerability profile (Brandes JL, 2004).
Antidepressants have long been used to treat migraines. The basis for their use is the information accumulated in the treatment of chronic pain. Antidepressants reduce the accompanying symptoms of depression, which is either present in the patient initially or develops in connection with frequent migraine attacks. Antidepressants potentiate the effect of analgesics and triptans, and some of them have independent antinociceptive or analgesic activity. The most favorable efficacy/safety ratio is observed in the new generation of antidepressants - venlafaxine (Velafax, Velaxin), duloxetine (Cymbalta), milnacipran (Ixel).
Prospects for migraine treatment
Currently, a phase 2 study is underway in Europe of the CGRP receptor antagonist olcegepant, which, when administered intravenously, prevents intracranial vascular dilatation that occurs during a migraine attack. Research is also being conducted on the first tablet form of the CGRP receptor antagonist, MK-0974, to relieve migraine attacks (Doods H. et al., 2007).
A group of American scientists from the Ohio University Medical Center conducted a study on the use of transcranial magnetic stimulation to interrupt migraine attacks with aura. According to current theory, the development of migraine begins with an increase in electrical activity in the occipital lobe, after which the electrical impulse spreads throughout the brain, causing the symptoms of a migraine aura. The essence of the technique is to interrupt this electrical activity using an electromagnetic pulse. More than two-thirds of patients treated with transcranial magnetic stimulation reported either no or moderate pain two hours after the procedure. Less than half of the patients reported the same effect in the placebo group (Clarke BM et al., 2006).
Clinical trials of a new drug, an aerosol for migraines, are currently underway. To supply the active substance, the patented technology for the manufacture of Stokatto inhalers is used, which has a number of features. The device has a built-in battery, which, when pressed on the piston, heats up one dose of a solid medicinal substance, turning it into an aerosol. The aerosol particle size—1–3 micrometers—is optimal for deep irrigation of the lungs, where the drug is quickly absorbed and enters the circulatory system at a speed comparable to intravenous injections. The new drug, codenamed AZ-001, is the Staccato system of prochlorperazine, a drug used to treat symptoms such as nausea and vomiting. Recently, research results were released that showed that when administered intravenously, this substance is effective for migraines. Thus, if the clinical trials are successful, Staccato Prochlorperazine will have undeniable advantages over tablets and intravenous injections, since it will combine the effectiveness of an intravenous drug with convenience and ease of use, which will allow the use of the inhaler at home (Alexza news release, 2007).
Non-pharmacological aspects of migraine treatment
Despite the fact that advances in the field of pharmacology play a huge role in the treatment of migraine, the skill of the doctor is no less important, and first of all his ability to build a dialogue with the patient. Here are the factors that doctors consider most important when achieving success in treating migraines.
- Collaboration with the patient. Particularly important is the sincere attitude of the doctor towards the patient, which is manifested through non-verbal communication (intonation, facial expressions, gestures). The patient will immediately feel if the doctor tries to hide his irritation behind encouraging remarks due to the fact that the patient is taking up his time with his questions, when the diagnosis is clear and the patient has long been given a leaflet with prescriptions.
- Involving the patient in the treatment process. The essence of the problem, treatment options should be explained to the patient and he should be involved in the choice of therapeutic agents, taking into account past experience, preferences and expectations. The time spent explaining the essence of the problem pays off with high patient adherence to treatment and, as a result, higher rates of effectiveness of the therapy.
- Patient education and training. Many patients are frustrated by the fact that various doctors and numerous tests do not find a physical cause for their headaches. In this situation, it is advisable to spend time explaining the pathogenesis of migraine. In addition, it is important to educate the patient to identify triggers and avoid migraine-provoking situations.
- Assessment of migraine severity. The severity of migraine is determined not only by clinical manifestations, but also by how much the disease interferes with the patient's life.
Critically evaluate the patient's past experiences, attitudes and expectations. Often patients turn to the doctor who have already tried all known medications and have not received the desired effect. In these cases, it is important to carefully question the patient about previous experience with the medication in order to understand what may be causing the lack of effectiveness.
Conclusion
Thus, treating migraine is a complex, complex task that requires erudition, sensitivity to the patient, good communication skills and patience from the doctor. Currently, not only modern drugs have been developed, but also new approaches to treatment that allow its selection based on objective criteria. However, a doctor faced with the treatment of migraine cannot be a simple executor of the proposed algorithms. In order for therapy to be effective and safe, it is necessary to creatively approach the choice of methods, taking into account the individual characteristics of patients. Also very important is the creation of a trusting and at the same time business relationship with the patient, his education and active involvement in the treatment process. If the doctor manages to cope with all of the above tasks, treatment will not only relieve the symptoms of the disease, but also improve the patient’s quality of life by eliminating or mitigating his social and work maladjustment, that is, achieving exactly what the patient comes to the doctor for.
For questions about literature, please contact the editor
A. B. Danilov , Doctor of Medical Sciences, MMA named after. I. M. Sechenova , Moscow
Prevention
Prevention of migraine attacks is not only properly selected drug therapy, but also correction of the patient’s lifestyle. Doctors recommend:
- normalize sleep: for the normal functioning of the body, at least 8 hours of night sleep every day are required;
- minimize the consumption of foods that can cause an attack, especially chocolate, spices, and alcoholic beverages;
- eliminate smoking;
- adhere to a balanced diet with a mandatory breakfast and intervals between meals of no more than 5 hours;
- observe the drinking regime and consume at least 1.5-2 liters of clean water per day; in hot weather this amount can reach 2.5-3 liters;
- establish a work and rest schedule, avoid mental and physical fatigue;
- reduce stress levels as much as possible;
- make a habit of light or moderate physical activity: swimming, walking, cycling, yoga, Pilates;
- promptly identify and treat chronic diseases, especially osteochondrosis of the cervical spine, atherosclerosis and other pathologies that contribute to the deterioration of blood flow in the brain.
Regular health resort treatment of a restorative nature and tourist trips without extreme changes in climate and time zones have a good effect.
Treatment at the Energy of Health clinic
Neurologists at the Health Energy clinic are ready to help with migraines of any severity. We offer each patient:
- individual selection of drugs for the relief and prevention of attacks;
- training in relaxation and self-help techniques;
- sessions of restorative massage and physical therapy in the absence of contraindications.
Treatment is selected according to the individual characteristics of the body. Before prescribing a specific regimen, a complete examination of the patient is carried out to exclude other causes of headache.
Advantages of the clinic
Medical facilities are equipped in accordance with modern standards of diagnosis and treatment of diseases. We try to make every patient feel comfortable within the walls of the clinic and offer:
- consultations with doctors of various specialties;
- informative methods of instrumental, functional and laboratory diagnostics;
- individual selection of treatment regimen;
- complex effect on the body using not only drugs, but also additional methods: physiotherapy, massage, exercise therapy, manual therapy, etc.
Reception is by appointment, without queues or long waits. The location of the centers allows both motorists and those traveling by public transport to reach us comfortably.
If migraine attacks are making your life miserable, do not endure the pain. Contact the neurologists at Health Energy. Together we will find a way to relieve you of this disease.
Risk factors
Statistics show that most often women of reproductive age from 15 to 45 years suffer from migraine attacks. The most dangerous age in this sense is from 35 to 40 years. Among men, only 6% of the country's total population suffer from the disease.
The mechanism of attack development has been sufficiently studied, but the exact causes of migraine are unknown. The main predisposing factor is heredity. If you carefully collect your family history, it turns out that there were already people in your family with such attacks. As a rule, women and men of the same kind are affected, and the degree of relationship may be different. The disease can develop both in direct relatives - sisters or daughters, and in granddaughters, cousins and second cousins. The pathological gene is transmitted through the maternal line. This is confirmed by statistical data: if the mother has seizures, then the probability of the disease in the child reaches 90%, and if the father has seizures, then only 20%.
If a patient experiences a headache, and there is no mention of such patients in the family history, then with a high degree of probability it is a tension headache or other diseases.