Laryngeal stenosis in children is a disease characterized by narrowing of the lumen, as a result of which breathing becomes qualitatively difficult for a certain period of time.
The mortality rate among young children with developed stenosis is too high and at the very first symptoms, the countdown begins on the hours and minutes of the child’s life.
Laryngeal stenosis in children always begins the same way: with signs of a common cold. At first, the child becomes very anxious and restless, the first cough appears, and the temperature rises. The complete appearance of a viral infection may remain for several days and nothing more. But the clinical picture changes quite quickly; sometimes it takes several hours for the baby to begin to develop suffocation.
Causes
The cause of stenosis can be not only viruses or bacteria, but also allergic reactions to home treatment: honey, raspberries, inhalations with herbs, pine buds, fir oil. Very often, children suffocate to the smell of Vietnamese balsam “Star”, flowering plants, cosmetics, perfumes, gasoline and other chemicals. Food allergens are also unsafe in this regard: citrus fruits, red vegetables and fruits, chicken eggs, sea fish, seafood, nuts, chocolate and other sweets.
Kinds
Depending on the location, there are several types of stenosis:
- narrowing of the spinal canal is spinal stenosis. It develops equally in both children and adults. Spinal stenosis is divided into congenital and acquired. Based on anatomical characteristics, they are divided into lateral and central. Lateral stenosis is a narrowing of the opening between the vertebra and the radicular canal, central stenosis is a narrowing of the distance between the vertebral body and the vertebra in the area of the spinous process. Spinal stenosis can have a secondary form, when the disease develops as a concomitant deformation of articular, bone tissue and ligaments with the formation of bone growths;
- Vascular stenosis develops due to high cholesterol levels, disorders of lipid-protein metabolism and deposition of lipoprotein particles on the walls of blood vessels. Blockage of blood vessels is accompanied by dizziness, vomiting, tinnitus, hallucinations, and general weakness of the body. The first degree of vascular stenosis, as a rule, does not have symptoms that would force you to immediately consult a doctor;
- Stenosis of the larynx (trachea) often affects children. This is a decrease in airway patency. The pathology is more often found as congenital. The main symptom is shortness of breath or suffocation;
- A stomach ulcer provokes the development of gastric stenosis. As a result of narrowing of the lumen between the gastric walls, spasms occur. Without treatment, gastric stenosis leads to an imbalance in the internal environment.
Symptoms
The first signs of illness in a baby may not be noticed even by the most attentive parents. This is explained by the fact that the symptoms of stenosis are very similar to the clinical manifestations of a common acute respiratory infection. The baby may have a slight increase in body temperature and a runny nose.
The next stage of development of stenosis is characterized by a strong paroxysmal cough, hoarse voice and rapid noisy breathing. Parents should also be concerned that the child’s condition is rapidly deteriorating, he becomes lethargic and irritable, which indicates the onset of hypoxia.
STRIDOR in newborns and children of the first year of life
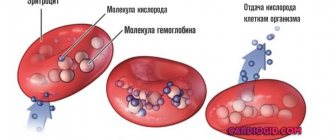
Stridor is a rough, variable-pitched sound caused by turbulent air flow as it passes through a narrowed area of the airway [36]. Stridor in newborns and infants is a pathology that is a symptom of respiratory obstruction [7]. Stridor can be a symptom of life-threatening illnesses. The most important characteristics of stridor are its volume, pitch, and the breathing phase at which it occurs.
Loud stridor is usually a symptom of severe airway narrowing. In the case of progressively worsening stridor, a sudden weakening of the sound may be a sign of increased obstruction, weakening of respiratory movements and the occurrence of airway collapse [28].
High-sounding stridor is usually caused by obstruction at the level of the vocal folds [26], while low-sounding stridor is usually caused by pathology above the vocal folds (the laryngeal part of the pharynx, the upper part of the larynx). Mid-range stridor is most often a symptom of obstruction below the vocal folds [41].
The most important sign to suspect the level of damage is the respiratory phase in which stridor is best heard. On this basis, stridor can be divided into three types: inspiratory, expiratory and biphasic. Inspiratory stridor is usually caused by a lesion located above the vocal folds and is produced by the collapse of soft tissue under negative pressure during inspiration [22]. Biphasic stridor is usually high-pitched. It is caused by a lesion at the level of the vocal folds or subglottic region [16, 18]. Expiratory stridor occurs more often with damage to the lower respiratory tract [42].
History is very important for diagnosing the disease. Key historical data are the reasons and duration of intubation (if previously performed) in the neonatal period. Other anamnestic features include age at onset of stridor, duration of stridor, association with crying or feeding, and position of the child; the presence of other associated symptoms, such as coughing paroxysms, aspiration or regurgitation [40, 41].
When examining a child, you should evaluate his general condition, respiratory and heart rate, and skin color. In addition, you should pay attention to possible anomalies in the structure of the head, the participation of additional muscles in the act of breathing, retraction of the compliant areas of the chest and other signs, and exclude a possible infectious disease [36].
If the child’s condition does not require immediate intervention, an x-ray of the larynx and soft tissues of the neck in the anterior and lateral projection, chest, as well as x-ray of the esophagus with a water-soluble radiopaque substance should be performed. In addition, ultrasound examination of the larynx, computed tomography, and nuclear magnetic resonance may be useful [12, 30].
The most informative method for diagnosing a disease manifested by congenital stridor is endoscopic examination: fiberoscopy; direct laryngoscopy under anesthesia, preferably using a microscope; tracheobroncho- and esophagoscopy [11, 36]. In this case, it is necessary to take into account the possibility of an abnormal structure of several parts of the respiratory tract [23, 25].
- The most common causes of stridor in newborns and infants
| Figure 1. Endophotograph of the larynx. Soft epiglottis extending into the airway |
Laryngomalacia is the most common cause of stridor [16, 30]. Anatomically, the following forms of laryngomalacia can be distinguished: due to the retraction of the soft epiglottis into the lumen of the larynx (Fig. 1); due to the arytenoid cartilages, when inhaling, they are pulled up or pulled up initially, due to the shortened aryepiglottic fold (Fig. 2); mixed form, when both the epiglottis and arytenoid cartilages fall into the lumen of the respiratory tract. Laryngomalacia usually occurs
| Figure 2. Endophotograph of the larynx. Arytenoid cartilages extending into the lumen of the larynx |
“benign” and disappears spontaneously, usually by 1.5 - 2 years of life.
Boys are affected twice as often as girls. Stridor usually appears from birth, but in some cases it does not occur until the second month of life. Symptoms may be transient and worsen when the child lies on his back or during crying and agitation. The severity of the disease may vary. Most children experience only noisy, sonorous breathing, but in some cases laryngomalacia causes laryngeal stenosis, requiring intubation and even tracheotomy. In severe cases, surgical treatment is resorted to, usually using a laser - making incisions on the epiglottis, dissecting the aryepiglottic folds or removing part of the arytenoid cartilages. Vocal fold paralysis is the second most common cause of congenital stridor [39, 41]. It is usually found in children with other congenital anomalies or central nervous system involvement [29]. Often the cause of paralysis remains unclear, and this type of paralysis is considered idiopathic. In cases of idiopathic paralysis (possibly caused by birth trauma), it is often
| Figure 3. Endophotograph of the larynx. Right arytenoid fold paralysis |
spontaneous healing occurs.
In other cases, the cause may be hemorrhages in the ventricles of the brain, meningoencephalocele, hydrocephalus, perinatal encephalopathy and other diseases [29]. In addition, iatrogenicity (for example, when the recurrent laryngeal nerve is damaged) can be identified as the cause of the development of vocal fold paralysis. Bilateral paralysis causes high-pitched stridor and aphonia. About half of children with bilateral paralysis require tracheotomy [22, 26, 39].
With unilateral paralysis (Fig. 3), a weak cry is usually noted, the voice gradually improves with age. Respiratory function is usually not affected by unilateral paralysis [28].
| Figure 4. Endophotograph of the larynx. Congenital scar membrane of the larynx |
Congenital cicatricial membrane (Fig. 4) and subglottic stenosis develop as a result of incomplete separation of the germinal mesenchyme between the two walls of the developing larynx [33]. Acquired cicatricial stenoses are found much more often (Fig. 5), usually developing as a result of prolonged transglottic nasotracheal intubation. The severity of the disease depends on the degree of damage: a small scar membrane, localized only in the area of the anterior commissure, is clinically manifested only by a change in voice (“cock crow”); complete laryngeal atresia is compatible with life only theoretically [30].
| Figure 5. Endophotograph of the larynx. Acquired subglottic stenosis (pinpoint airway lumen) |
The leading clinical symptoms of the disease are obstruction of the upper respiratory tract, such as biphasic stridor, tachypnea, cyanosis, anxiety, flaring of the wings of the nose when breathing, participation of auxiliary muscles in the act of breathing, etc. When the membrane is localized in the area of the vocal folds, voice disorders up to aphonia are noted .
The leading diagnostic method is endoscopy [30], although radiography of the larynx and trachea in anterior and lateral projections indirectly helps.
| Figure 6. Endophotograph of the larynx. Cyst of the lingual surface of the epiglottis |
Treatment is determined by the severity of symptoms. Only children with small anterior commissural synechiae can be kept under observation without surgical treatment; patients with a medium-sized membrane that causes breathing problems require surgical treatment (usually laser destruction) during the neonatal period. Children with severe membrane usually require tracheotomy in the neonatal period followed by surgery (using a laser or external approach) at an older age [17, 38].
| Figure 7. Endophotograph of the larynx. Right vocal fold cyst |
In some cases, congenital subglottic stenosis is accompanied by other congenital lesions [34]. When choosing treatment tactics, it is necessary to take into account that breathing can improve with the growth of the larynx.
Laryngeal cysts. Stridor occurs when a cyst grows into the lumen of the respiratory tract or compression of the soft tissues of the larynx. In addition, when localized on the laryngeal and especially on the lingual surface of the epiglottis (Fig. 6), they can cause dysphagic phenomena [20, 30].
The localization of cysts can be varied - epiglottis, supraglottic region, aryepiglottic folds, subglottic region. Often cysts develop in children with a history of intubation, and in such cases they can be multiple. Small cysts of the vocal folds (Fig. 7) are clinically manifested only by hoarseness. With mirror laryngoscopy, especially if the submucosal cyst is localized at the border of the anterior and middle third of the vocal fold, it is mistakenly diagnosed as a “singing” nodule. In this case, the correct diagnosis can only be established by examining the larynx under anesthesia using optics.
| Figure 8. Endophotograph of the larynx. Subglottic hemangioma under the left vocal fold |
For treatment, aspiration of the cyst contents is used, followed by excision of its walls with microinstruments or a CO2 laser [6, 8, 30].
Cysts often recur. In some cases, external surgery is required to excise large multiple recurrent cysts [31].
Subglottic hemangioma (Fig. threatens the life of the child. According to foreign literature, the average mortality from this disease is 8.5% [43]. In most cases, subglottic hemangioma is present from birth and undergoes growth during the first months of life. Stridor usually appears at 2 -3 months of life, the first symptoms of the disease are usually mistakenly diagnosed as croup [27]. In three of our cases, respiratory stenosis developed on the first day after cryodestruction of skin hemangiomas. Stridor is usually biphasic, the voice may not be changed. More than half of the children have skin hemangiomas. How and with skin hemangiomas, girls suffer three times more often than boys [9].The severity of the disease depends on the size of the hemangioma, in the case of acute respiratory viral infection or anxiety, breathing may worsen.
threatens the life of the child. According to foreign literature, the average mortality from this disease is 8.5% [43]. In most cases, subglottic hemangioma is present from birth and undergoes growth during the first months of life. Stridor usually appears at 2 -3 months of life, the first symptoms of the disease are usually mistakenly diagnosed as croup [27]. In three of our cases, respiratory stenosis developed on the first day after cryodestruction of skin hemangiomas. Stridor is usually biphasic, the voice may not be changed. More than half of the children have skin hemangiomas. How and with skin hemangiomas, girls suffer three times more often than boys [9].The severity of the disease depends on the size of the hemangioma, in the case of acute respiratory viral infection or anxiety, breathing may worsen.
The leading diagnostic method is endoscopy. Usually a pink or red soft tissue protrusion is found under the vocal fold (usually under the left) [5]. If the child has been previously intubated due to respiratory stenosis, the hemangioma may not be diagnosed when examining the airway immediately after extubation.
Treatment uses CO2 laser destruction of hemangioma followed by hormonal therapy [6, 24]. In case of hemangioma of the anterior surface of the neck that grows into the larynx, tracheotomy is necessary, followed by close-focus radiotherapy or treatment with corticosteroids [2].
| Figure 9. Endophotograph of the larynx. Juvenile respiratory papillomatosis |
Juvenile respiratory papillomatosis (JRP) (Fig. 9) is the most common tumor of the upper respiratory tract in children. The etiological factor of papillomatosis is the human papillomavirus, most often types 6 and 11 [3]. Although in the vast majority of patients the first symptoms of the disease develop at 2–3 years of life, in some cases we can talk about congenital laryngeal papillomatosis, when the first symptoms of the disease are noted from the moment of birth [1].
The initial symptom of the disease is usually hoarseness, gradually turning into aphonia. Subsequently, as papillomas grow and the lumen of the glottis narrows (obstructive form), progressive laryngeal stenosis occurs, manifesting itself as inspiratory or biphasic stridor [10].
The most common primary localization of laryngeal papillomas is the area of the commissure and the anterior third of the vocal folds. At later stages of the disease, papillomas can affect all parts of the larynx, as well as extend beyond its limits. Papillomas usually have a wide base, but the growth of conglomerates of papillomas on a small stalk is possible. In appearance, papillomas resemble a mulberry or a bunch of grapes. During microlaryngoscopy, the surface of papillomas is usually uneven, fine-grained or finely lobed, the color is often pale pink, sometimes with a grayish tint. The severity of the disease is determined by the growth rate of papillomas and the frequency of recurrence [15].
The main method of eliminating stenosis in children with JRP is surgical removal of papillomas using microinstruments and/or a CO2 laser. However, surgical treatment alone does not prevent relapse of the disease in most patients. Currently, the most pathogenetically justified and promising is long-term continuous administration of interferon drugs [13, 19, 21].
Tracheomalacia. There are diffuse and local forms of tracheomalacia, i.e. weakness of the tracheal wall associated with the pathological softness of its cartilaginous frame. Clinically, the disease manifests itself as expiratory stridor. During endoscopy, a sharp narrowing of the tracheal lumen is detected during exhalation, which can take various shapes. Symptoms of the disease often disappear spontaneously by 2–3 years of life [32]. Severe respiratory distress may require tracheotomy [41].
| Figure 10. Endophotograph of the trachea. Congenital cicatricial stenosis |
Congenital tracheal stenosis (Fig. 10) can have a different nature. Organic stenoses are associated with a local defect in the cartilaginous half-rings of the trachea (lack or absence of cartilage) or excessive formation of cartilage tissue, leading to the formation of a hard cartilaginous protrusion into the tracheal lumen [42].
Functional stenoses are associated with excessive softness of the cartilage and in this case are a local form of tracheomalacia. Expiratory stridor is usually detected immediately after birth. Stridor gets worse when the baby is restless or feeding. The patient's condition usually worsens sharply during ARVI; in some cases, attacks of suffocation are noted, which are mistakenly diagnosed as croup. To exclude external compression of the trachea, an X-ray contrast examination of the esophagus is necessary. The main diagnostic method is endoscopic. Tracheal stenosis, especially due to tracheomalacia, has a favorable prognosis and, in most cases, heals spontaneously.
| Figure 11. Chest X-ray. Compression of the esophagus by an abnormally located vessel |
Vascular ring. The abnormal configuration of large vessels can cause compression of the trachea, usually its distal parts.
In addition, the esophagus may also be compressed. Stridor gets worse when crying or feeding, or when the baby is lying on his back. Regurgitation is often noted. The diagnosis is established using radiography of the esophagus with a radiopaque agent (Fig. 11) and aortography. The most common type of aortic arch duplication is the accessory left pulmonary artery [14, 37]. During endoscopy, bulging and, in some cases, pulsation of the anterior wall of the trachea can be detected. Treatment is surgical.
Laryngotracheoesophageal hiatus is a rare congenital developmental defect. Over a long distance, the respiratory tract communicates with the esophagus. The cause of this defect is non-fusion of the dorsal part of the cricoid cartilage. This disease is clinically manifested by moderately loud biphasic stridor and episodes of aspiration. Children with this defect often experience repeated pneumonia. Paroxysms of cough and cyanosis are typical. The voice is quiet. Approximately 20% of children also have a tracheoesophageal fistula, typically located in the distal trachea [35]. To establish a diagnosis, in addition to endoscopy, chest X-ray with contrast is required. Treatment requires not only a tracheotomy, but also a gastrostomy tube to feed the child.
| Figure 12. Chest X-ray. Flow of radiopaque substance through the tracheoesophageal fistula from the esophagus into the tracheobronchial tree |
Tracheoesophageal fistula (Fig. 12) manifests itself during the first feeding of the child with severe attacks of suffocation, coughing and cyanosis [41]. The defect is based on incomplete development of the tracheoesophageal wall. Often this defect is combined with esophageal atresia. Subsequently, severe aspiration pneumonia quickly follows. Treatment is surgical only, the results often depend on the timing of the operation. The prognosis is more favorable the earlier the intervention is undertaken.
- Medical genetic counseling
Considering that malformations of the larynx and trachea are a manifestation of embryopathies, in patients with congenital pathologies of these organs, manifestations of embryopathies from other organs and systems are very likely. In clinical practice, the greatest difficulty in establishing the nosological form of the disease is its syndromic forms. The syndromic examination method is based on the fact that most developmental defects can be isolated or be part of known syndromes or unspecified complexes of multiple congenital defects. Establishing a syndromic diagnosis influences the following factors: 1) conducting a thorough diagnosis of hidden developmental defects and functional abnormalities within the established syndrome; 2) performing specific preoperative preparation of the patient to prevent possible complications during surgery or in the postoperative period; 3) tactics and results of treatment, which in some cases is expressed in the refusal of surgical interventions, including changes in the surgical technique for correcting certain developmental defects.
According to our data, a syndromic diagnosis can be established in approximately 25% of patients [4]. Only 8-10% of children have an isolated form of congenital pathology of the larynx and trachea. The remaining patients with congenital diseases of the larynx and trachea have other developmental defects - the central nervous, musculoskeletal, cardiovascular systems, developmental anomalies of the auricles, facial developmental defects, connective tissue abnormalities, congenital tumor-like formations of the skin, etc. A combination of developmental defects of several organs systems that are not induced by each other in this group of patients can be regarded as multiple unspecified congenital malformations.
Literature
1. Bogomilsky M. R., Soldatsky Yu. L., Maslova I. V., Nurmukhametov R. Kh. Congenital juvenile respiratory papillomatosis of the larynx // Bulletin of Otorhinolaryngology. 1998. No. 6. P. 28 - 29. 2. Vodolazov S. Yu., Pospelov N. V. Combined treatment of children with widespread hemangiomatosis of the head, neck, face in combination with subglottic hemangioma of the larynx. In the book: Materials of the XV All-Russian Congress of Otorhinolaryngologists, September 25-29, 1995, Volume II. St. Petersburg, 1995. P. 273 - 275. 3. Gerain V., Chireshkin D. G. Molecular biological aspects of juvenile respiratory papillomatosis and its combined treatment // Bulletin of Otorhinolaryngology. 1996. No. 4. P. 3 - 8. 4. Maslova I.V., Solonichenko V.G., Soldatsky Yu.L., Onufrieva E.K. Genetic aspects of congenital pathology of the larynx and trachea // Bulletin of Otorhinolaryngology. 1999. No. 2. P. 30 - 33. 5. Soldatsky Yu. L., Onufrieva E. K. Subglottic hemangioma as a cause of laryngeal stenosis in young children // Bulletin of Otorhinolaryngology. 1997. No. 6. P. 19 - 21. 6. Soldatsky Yu. L., Maslova I. V., Onufrieva E. K. Laser endoscopic surgery of congenital diseases of the larynx in children // Laser medicine. 1998. T. 2. No. 2 - 3. P. 36 - 38. 7. Soldatsky Yu. L., Onufrieva E. K., Maslova I. V. Stridor in newborns and infants. In the book: Materials of the V Congress of Pediatricians of Russia “Healthy Child”, 02.16-18.1999. Moscow, 1999. P. 430 - 431. 8. Tsvetkov E. A., Fadeeva I. A. Surgical treatment of congenital laryngeal cysts // Bulletin of Otorhinolaryngology. 1999. No. 3. P. 42 - 45. 9. Chireshkin D. G., Onufrieva E. K., Soldatsky Yu. L. Vascular tumors of the larynx, pharynx and oral cavity in children // Bulletin of Otorhinolaryngology. 1994. No. 4. P. 29 - 32. 10. Chireshkin D. G. Chronic obstruction of the laryngeal part of the pharynx, larynx and trachea in children. M.: Rapid-Print, 1994. P. 144. 11. Chireshkin D. G., Maslova I. V., Onufrieva E. K., Soldatsky Yu. L. Structure and early symptoms of congenital diseases of the larynx and trachea // Bulletin otorhinolaryngology. 1996, No. 5. P. 13 - 18. 12. Shanturov A. G., Subbotina M. V. Ultrasound diagnostics in pediatric laryngology. Irkutsk: Papyrus, 1994. P. 140. 13. Avidano MA, Singleton GT Adjuvant drug strategies in the treatment of reccurrent respiratory papillomatosis // Otolaryngology - Head and Neck Surgery. 1995. Vol. 112. P. 197 - 202. 14. Backer CL, Ilbawi MN, Idriss FS Vascular anomalies causing tracheoesophageal compression // J. Thorac Cardiovasc. Surg. 1989. Vol. 97. P. 725 - 731. 15. Bauman NM, Smith RJ Recurrent respiratory papillomatosis // Pediatr. Clin. North. Am. 1996. Vol. 43. P. 1385 - 1401. 16. Belmont JR, Grundfast KM Congenital laryngeal stridor (laryngomalacia): etiologic factors and associated disorders // Ann. Otol. Rhinol. Laryngol. 1984. Vol. 93. P. 430 - 436. 17. Benjamin B., Jacobson I., Eckstein R. Idiopathic subglottic stenoses: diagnosis and endoscopic laser treatment // Ann. Otol. Rhinol. Laryngol. 1997. Vol. 106. P. 770 - 774. 18. Benjamin B., Mair EA Congenital interarytenoid web // Arch. Otolaryngol. Head Neck Surg. 1991. Vol. 117. P. 1118 - 1122. 19. Chmielik M., Piekarniak P., Snieg B. Microsurgical treatment of laryngeal papillomatosis // Otolaryngol. Pol. 1997. Vol. 51. P. 26 - 30. 20. Civantos FJ, Holinger LD Laryngoceles and saccular cysts in infants and children // Arch. Otolaryngol. Head Neck Surg. 1992. Vol. 118. P. 296 - 300. 21. Deunas L., Alcantud V., Alvarez F. et al. Use of interferon-alpha in laryngeal papillomatosis: eight years of the Cuban national program // J. Laryngol. Otol. 1997. Vol. 111. P. 134 - 140. 22. Ferguson CF Congenital abnormalities of the infant larynx // Ann. Otol. Rhinol. Laryngol. 1967. Vol. 76. P. 744 - 752. 23. Friedman EM, Vastola AP, McGill TJ, Healy GB Chronic pediatric stridor: etiology and outcome // Laryngoscope. 1990, Vol. 100. P. 277 - 280. 24. Froehlich P., Seid AB, Morgon A. Contrasting strategic approaches to the management of subglottic hemangiomas // Int. J. Pediatr. Otorhinolaryngol. 1996. Vol. 36. P. 137 - 146. 25. Gonzales C., Reilly JS, Bluestone CD Synchronous airway lessions in infants // Ann. Otol. Rhinol. Laryngol. 1987. Vol. 96. P. 77 - 80. 26. Grundfast KM, Harley EH Vocal cord paralysis // Otolaryngol. Clin. North. Am. 1989. Vol. 22. P. 569 - 597. 27. Healy GB, McGill T., Friedman EM Carbon Dioxide Laser in Subglottic Hemangioma. An update. //Ann. Otol. Rhinol. Laryngol. 1984. Vol. 93. P. 370 - 373. 28. Holinger LD Etiology of stridor in the neonatal, infant and child // Ann. Otol. Rhinol Laryngol. 1980. Vol. 89. P. 397 - 400. 29. Holinger LD, Holinger PC, Holinger PH Etiology of bilateral abductor vocal cord paralysis: A review of 389 cases // Ann. Otol. Rhinol. Laryngol. 1976. Vol. 85. P. 428 - 436. 30. Holinger LD, Lusk RP, Green CG Pediatric laryngology and bronchoesophagology. Philadelphia - NY: Lippincott - Raven, 1997. R. 402. 31. Holinger PH, Brown WT Congenital webs, cysts, laryngoceles and other anomalies of the larynx // Ann. Otol. Rhinol. Laryngol. 1967. Vol. 76. P. 744 - 752. 32. Jacobs I., Welmore R., Tom L. et al. Tracheobronchomalacia in children // Arch. Otolaryngol. Head Neck Surg. 1994, Vol. 120. P. 154 - 158. 33. McGill T. Congenital diseases of the larynx // Otolaryngol. Clin. North. Am. 1984. Vol. 17. P. 57 - 62. 34. Miller R., Gray SD, Cotton RT, Myer CM, Netterville J. Subglottic stenosis and Down syndrome // Am. J. Otolaryngol. 1990. Vol. 11. P. 274 - 277. 35. Myer CM, Cotton RT, Holmes D. Laryngeal and laryngotracheoesophageal clefts: The role of early surgical repair // Ann. Otol. Rhinol. Laryngol. 1990. Vol. 99. P. 98 - 104. 36. Nowlin JH, Zalzal G. The stridorous infant // ENT J. 1989. V. 70. P. 84 - 88. 37. Park SC Vascular abnormalites // Pediatr. Clin. North. Am. 1981. Vol. 28. P. 949 - 955. 38. Park SS, Streitz JM Jr., Rebeiz EE, Shapshay SM Idiopathic subglottic stenosis // Arch. Otolaryngol. Head Neck Surg. 1995. Vol. 121. P. 894 - 897. 39. Parnell FW, Brandenberg JH Vocal cord paralysis: A review of 100 cases // Laryngoscope. 1970. Vol. 70. P. 1036 - 1045. 40. Pransky SM, Grundfast KM Differentiating upper from lower airway compromise in neonates // Ann. Otol. Rhinol. Laryngol. 1985. Vol. 94. P. 509 - 515. 41. Richardson MA, Cotton RT Anatomic abnormalities of the pediatric airway // Pediatr. Clinic. North. Am. 1995. Vol. 31. P. 821 - 834. 42. Rimmell FL, Stool SE Diagnosis and management of pediatric tracheal stenosis // Otolaryngol. Clin. North. Am. 1995. Vol. 28. P.809 - 827. 43. Shikhani AH, Marsh BR, Jones MM, Holliday MJ Infantile subglottic hemangiomas. An update // Ann. Otol. Rhinol. Laryngol. 1986. Vol. 95. P. 336 - 347.
Note!
- Stridor in newborns is a symptom of partial obstruction of the large diameter airways
- To diagnose the disease, a thorough history and clinical examination of the child is necessary to assess the severity of his condition.
- The level of damage can be suspected by the stridor phase and associated symptoms, such as cough, regurgitation, cyanosis
- The main method of diagnosis is endoscopy, although radiographic and ultrasound examinations can be very useful in some cases
- All patients with congenital pathology of the larynx and trachea need to be examined in a medical genetic consultation
Diagnostics
Laryngeal stenosis in children is diagnosed by a differential method, as a result of which it is possible to identify the causes and distinguish laryngeal stenosis from laryngospasm, tracheal stenosis, and an attack of bronchial asthma. Stenosis is detected by examination and palpation against a background of severe symptoms.
To qualitatively identify the cause of stenosis, the following examinations are carried out: tomography, laryngoscopy, radiography of the larynx and the entire esophagus, ultrasound examination of the thyroid gland, bacteriological examinations of the pharynx, tracheobronchoscopy.
Laryngeal stenosis in children
Conservative therapy
In case of acute stenosis, medicinal measures are of an auxiliary nature and are included in the emergency care package.
The child is administered corticosteroids in age-appropriate dosages and anticholinergic drugs. To compensate for hypoxia, after eliminating the stenosis, breathing with humidified oxygen mixtures is carried out. After stabilization of well-being, treatment is selected according to the etiopathogenetic principle. Mild forms of the disease are subject to outpatient therapy; for others, hospitalization is recommended. If symptoms of laryngitis are detected, non-steroidal anti-inflammatory drugs and antihistamines are prescribed. To eliminate viscous sputum, which clogs the lumen of the respiratory tract, mucolytics and alkaline inhalations are used (for children after 4-5 years). Antibacterial therapy is selected if necessary.
According to the cause of stenosis, antiviral, antimicrobial, and antifungal drugs can be used in the hospital. When symptoms are caused by neuromuscular disorders, muscle relaxants are indicated. In case of intense edema, adrenergic agonists are effective in the form of solutions and inhalations, which have a powerful vasoconstrictor effect. Physiotherapy includes ultraviolet irradiation and electrophoresis on the neck area.
Surgery
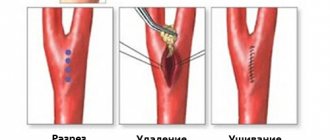
In case of acute development of severe stenosis and asphyxia, surgical intervention is performed as quickly as possible. In emergency cases, a conicotomy is indicated - a dissection of the larynx between the cartilages to ensure air flow into the respiratory tract. In children over 8 years of age, a less traumatic puncture conicotomy is performed, during which a catheter with a needle is installed.
For chronic cicatricial stenoses, surgical correction is performed routinely. Endoscopic operations are more often used: balloon dilatation, laser microsurgery, intervention using a microdebrider. In children, surgical treatment with external access is also used: laryngoplasty using an autograft, resection of the larynx, laterofixation of the vocal folds.
Rehabilitation
For successful recovery after surgical treatment, the child is prescribed a gentle regimen. Observation by an ENT doctor is carried out for 2-3 months, once every 2 weeks. Experts advise maintaining a voice mode (quiet conversation, avoiding screaming and loud laughter), eliminating hot and spicy foods so as not to irritate the mucous membranes and not provoke symptoms of suffocation.
Treatment
Laryngeal stenosis in children develops too quickly and there is no point wasting time here. If choking is evident, a prednisone injection can be given to help the child breathe easier. You just need to know for sure that there is no other choice and judge, if possible, sensibly: if the doctors are already on the way, and hot steam and rubbing the legs help, the child is breathing, then there is no need to inject the drug.
Calling an ambulance followed by a visit to the local pediatrician is vital for recovery. Firstly, the attack may recur, but you cannot inject the drug every time. The child is in dire need of good and comprehensive treatment, a course of physiotherapy, treatment with antibiotics and elimination of swelling of the larynx.
At the time of an attack, a critical situation often occurs, then specialists have to perform surgery on the spot. A section is made in the trachea area to allow air to enter, and a special tube is inserted.
During a crisis, constant monitoring is necessary and can only be provided in a hospital setting.
Coarctation of the aorta in children
For coarctation of the aorta in children, treatment may involve surgery. The indication for this method is the difference in systolic pressure measured in the arms and legs exceeding 50 mmHg. Art. For infants, the indication for surgery will be severe arterial hypertension and cardiac decompensation.
If the disease is detected several months after birth, but the course is favorable, then the operation is postponed until the child is five or six years old. The operation can be performed on a patient at an older age, but the results will not be as good due to the possibility of persistent arterial hypertension.
Today, several methods of surgical treatment of coarctation of the aorta - resection and reconstruction of the aorta:
1. Aortic plastic surgery using vascular prostheses
This treatment method is used if the aorta is narrowed over a large area, which makes it impossible to compare the ends of the normal areas.
2. Resection of coarctation of the aorta with anastomosis (anastomosis) end to end
This treatment method is relevant if the area is narrowed over a small extent
3. Bypass surgery of a pathologically narrowed area of the aorta
A vascular prosthesis is made from a special material. Its edges are sutured below and above the narrowed area to create a path for blood to flow.
4. Aortoplasty using the left subclavian artery of the operated child
5. Balloon angioplasty and stenting of aortic coarctation
The method is relevant if the child has had surgery before, but re-narrowing has occurred. A balloon is inserted into the aorta and inflated, eliminating the narrowing. In some cases, it may be necessary to install stents to maintain the required aortic diameter.
Prognosis for coarctation of the aorta in children
The prognosis varies depending on the degree of narrowing of the child's aorta. If coarctation of the aorta is insignificant, then the child has no obstacles to a normal lifestyle, and life expectancy is not shortened - on average, it is the same as for people without the diagnosis in question.
If coarctation of the aorta is significant, then life expectancy, if surgery is not performed, will average 30 to 35 years. Patients die from bacterial endocarditis and severe heart failure. Sudden death may occur due to aortic rupture or aneurysm and stroke.
Degrees of stenosis
The degree of stenosis is determined by changes occurring in the body:
- 1st degree: no serious disorders are observed, although plaques are already forming on the walls of blood vessels, shortness of breath appears during physical activity. With gastric stenosis at this stage, a sour taste in the mouth and belching appears; with spinal stenosis – fatigue increases, the back gets tired and the legs become heavier; with laryngeal stenosis – shortness of breath appears;
- 2nd degree: symptoms of any type of stenosis become more acute and already cause significant discomfort, forcing you to seek help from a doctor;
- 3rd degree: if treatment has not been prescribed so far, the patient puts his life at risk. Because at this stage, patency in the affected tissues and organs is approaching minimal.
Chronic forms of the disease progress slowly, gradually reducing the patient's quality of life. Acute forms are characterized by sudden attacks.