Officials from the UK's National Health System (NHS) have issued a warning to the country's doctors about a rise in the number of cases of children being admitted to intensive care with multisystem inflammatory symptoms associated with coronavirus.
The number of such cases has increased sharply over the past three weeks, it said. Patients require intensive care and this is seen across London as well as other areas of the UK. As experts note, in all cases there are signs of toxic shock syndrome and an atypical form of Kawasaki syndrome.
Doctors say the exact nature of the syndrome has not yet been determined. Doctors believe that it may be caused by an as yet unidentified infection that has gained momentum amid the coronavirus. Earlier, 20 such cases over the past month were reported in Bergamo, Italy, the region in northern Italy that has been hardest hit by the coronavirus. Local doctors said cases of severe Kawasaki syndrome have been identified in children under the age of nine.
Article on the topic
“I went through all the circles of hell.” Doctors saved a patient with coronavirus infection
Causes
The exact causes of Kawasaki syndrome have not been established. In 10% of cases the disease is inherited. Provoking factors:
- streptococcal infections;
- diseases caused by staphylococci;
- herpes virus, Epstein-Barr;
- parvoviruses, retroviruses.
These pathogens are not causative agents of the disease, but can cause infection.
Etiopathogenesis
The etiology and pathogenesis of the syndrome are currently not fully understood. There are several theories about the origin of the pathology - hereditary, autoimmune, infectious.
- The hereditary nature of the disease is supported by the fact that people who have ancestors with Kawasaki syndrome also develop it in 10% of cases. It has been proven that the pathology affects close relatives.
- Cyclicity and seasonality are signs confirming the infectious etiology of the disease. The number of cases reaches its maximum in spring and winter.
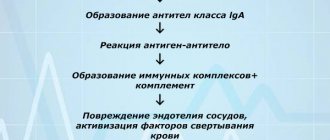
- Autoimmune theory: the body responds to exposure to toxins by producing antibodies to its own vascular endothelial cells.
Modern rheumatologists recognize the hypothesis that the disease develops in individuals with a genetic predisposition under the influence of exogenous factors: bacteria and viruses. The most dangerous in relation to the syndrome are streptococcal, staphylococcal, rickettsial, cytomegalovirus and herpesvirus infections.
Pathogenetic links of the syndrome:
- Impact on the body of infectious biological agents,
- Activation of T lymphocytes,
- Production of antibodies to microbes and endothelial cells,
- Development of immunological reactions against endothelial cells,
- Inflammation of the muscular layer of the arteries,
- Necrosis of smooth muscle cells,
- Endothelial destruction
- Splitting and stratification of elastic membranes of blood vessels,
- Pathological dilatation of arteries and formation of aneurysm,
- Fibrosis of the walls of blood vessels,
- Proliferation and thickening of the intima,
- The appearance of general symptoms of the disease,
- Narrowing of the lumen of the vessel,
- Thrombosis and occlusion of the affected artery.
In the absence of timely and correct treatment of the syndrome, the prognosis becomes unfavorable. As a result of stenosis and blockage of the coronary arteries by a thrombus, myocardial infarction occurs, which often causes death in patients.
Video: mechanism of arterial damage in Kawasaki syndrome
What are the dangers of the syndrome and complications?
Pathology negatively affects the functioning of the cardiovascular system.
Due to the dilation of coronary vessels, the risk of developing myocardial infarction increases several times. Other complications of Kawasaki infection are acute cardiac, aortic, mitral insufficiency, aneurysms in large arteries. Less commonly diagnosed are cholecystitis, pancreatitis, urethritis, and pleurisy.
Death occurs due to rupture of blood vessels.
Prognosis for recovery
In the vast majority of cases, the prognosis is positive. The general course of treatment lasts on average 3 months. The mortality rate from Kawasaki disease is about 1-3%, mainly from vascular thrombosis and subsequent rupture or myocardial infarction.
About 20% of patients who have suffered from the disease acquire irreversible changes in the walls of the coronary vessels, which in the future becomes the cause of atherosclerosis, cardiac ischemia and an increased risk of myocardial infarction.
Smoking and hypertension contribute to this . All patients must be under constant supervision of a cardiologist throughout their lives and undergo a complete examination of the heart and coronary system at least once every 5 years.
Is it possible to correct facial asymmetry in a baby? Find out the answer right now.
Stages of the disease
Most often, the first manifestations of Kawasaki disease in children occur at the age of 1-5 years, less often - up to 8 years. The disease very rarely affects babies under six months of age.
The pathological process occurs in 3 stages:
- Acute – lasts about 7 days.
- Subacute – duration 2 weeks or more;
- Recovery will take up to 2 years.
Sometimes the disease becomes chronic.
If coronary aneurysms are present, they may persist into adulthood. This can trigger the development of serious cardiovascular diseases in the future.
Risk factors
Risk factors for developing Kawasaki disease include:
- Age
: from 1 year to 5 years - Gender
: boys get sick more often than girls - Ethnicity
: Children of Asian descent, especially Japanese or Chinese, and African Americans are more susceptible to Kawasaki disease - Genetics
: If parents had Kawasaki disease, their children are more prone to it, which may be due to an inherited gene - Environment
: in the northern hemisphere, from January to March this figure is 40% higher than in August-October.
Some speculate that it may be a reaction to certain toxins or drugs, but clinical evidence is lacking.
Symptoms
One of the main symptoms of Kawasaki disease is fever.
An increase in temperature to 39 degrees or more is observed within 12-14 days. The longer this period, the worse the prognosis for recovery. Kawasaki disease - symptoms:
- Rashes in the form of flat spots, blisters, are similar to the rash of measles and scarlet fever. Locations: body, limbs, groin area. The rash may appear within 5 weeks of the onset of illness.
- After 15-20 days, the rash disappears, leaving peeling.
- The skin on the feet and palms turns red and becomes dense.
- Conjunctivitis - inflammation appears in the first week, affects both eyes at the same time, there is no purulent discharge. Sometimes anterior uveitis develops.
- Cracks appear on the lips, the surface of the tongue has a crimson tint, and the mucous membrane in the oral cavity dries out.
- Cervical lymph nodes and tonsils become enlarged.
- Arthralgia, arthritis of the knee and ankle joints.
- Increased irritability, convulsions, paralysis of the limbs and facial nerve.
- Rarely – abdominal pain, vomiting, diarrhea, meningitis, urethritis.
The disease affects the heart and blood vessels. This manifests itself in the form of shortness of breath, arrhythmia, and tachycardia.
One of the features of the pathology is the rapid development of coronary artery aneurysm; the pathological process occurs within 1-4 weeks.
Development mechanism
The violation was and remains quite mysterious. Scientists have not come to a consensus about the etiology of this process or its origin. However, there is some progress in terms of research.
There is a group of theories regarding the pathogenesis of Kawasaki syndrome.
Hereditary factor
The vast majority of experts adhere to the version that the disorder has genetically determined features. This is supported by, among other things, racial, point and very selective preferences of the state. The Japanese suffer, more often than other Asians.
Why is that? Apparently, the predisposition is transmitted with certain genes, with a whole group. Which leads to an increase in morbidity in the population.
It has not yet been possible to say exactly how likely the disease is in a person with a complicated medical history. Research continues.
Infectious mechanism
This theory is based on the assumption that viruses (herpes, in particular Epstein-Barr) or bacteria such as staphylococci are to blame.
Here the opinions of experts are divided:
- Some suggest that the disorder is purely septic in nature. That is, it begins with damage to the arterial walls by the abnormal agents themselves.
- Others believe that any infectious focus can become a trigger. Trigger mechanism. And it is not necessary for a virus or bacteria to infect blood vessels.
And here comes the final perspective on Kawasaki disease.
Autoimmune mechanism
Proponents of this theory believe that septic agents do not directly provoke the syndrome. We are talking about increasing the sensitivity of the body.
If a bacterium or virus lasts long enough, the defenses fail. Weakening positions. The risk of their malfunction increases.
Ultimately, the immune system attacks its own cells and tissues. Causes inflammation. In this case, Kawasaki disease becomes even closer to vasculitis.
Most researchers adhere to some kind of synthetic theory. All three mechanisms play a role in etiology. Heredity and exposure to infection are the main culprits. They provoke disorder in the system.
Diagnosis of Kawasaki syndrome
Kawasaki disease is diagnosed if the fever lasts more than 5 days and at least 4 symptoms of the disease are observed.
Diagnostic methods:
- general blood test - anemia, leukocytosis, thrombocytosis, increased ESR are observed;
- urine test - there are signs of leukocyturia, proteinuria;
- biochemical blood test - reveals an increase in the level of transaminase, immunoglobulins, seromucoid, the presence of CEC;
- immunological tests - show the level of C-reactive protein;
- ECG, EchoCG, ultrasound of the heart;
- chest x-ray;
- coronary angiography.
Rarely, if indicated, a lumbar puncture, cerebrospinal fluid examination, and ultrasound of the gallbladder are performed.
What is a hemorrhagic rash?
When the capillaries are damaged, some of the red blood cells come out of the vessel, which leads to the appearance of a rash with red spots - this is a hemorrhagic rash.
Initially, the rash is painless, but if you ignore the rash, it may become painful. When you press on the rash, its color does not change in any way, and the rash does not become smaller. This is the hallmark of hemorrhagic rashes.
Depending on the lesion that caused the rash, the types of rashes can be different - small dots, stripes or spots, the color of which can also be varied - blue, red, purple. The size of the spots may vary. In medical practice, medium-sized spots are usually called liver purpura, and small spots are called petechiae.
The most common area of localization of the rash is the lower extremities. If a hemorrhagic type rash develops, you should immediately consult a doctor, as this is a direct indication for hospitalization, even in the absence of other symptoms.
Features of hemorrhagic rash in children
A hemorrhagic rash in children usually accompanies hemorrhagic vasculitis, hemophilia, meningococcemia, and thrombocytopenic purpura. But hemorrhagic vasculitis is the most common disease, the manifestation of which is a rash.
As already mentioned, the most common manifestation of the rash occurs on the front surfaces of the legs. However, it can also be localized on the torso, buttocks, and thighs. The rash is located symmetrically, does not disappear when pressed and does not change its color. The disease usually affects children under six years of age.
In addition to hemorrhagic rashes, other types of rashes also occur in children. In the article on the website you can see a photo of a rash on a child’s body with explanations.
Treatment of the disease
Therapy is not aimed at preventing the development of an aneurysm. When treating the syndrome, the following may be prescribed:
- acetylsalicylic acid - prescribed to eliminate the inflammatory process and prevent the formation of blood clots;
- anticoagulants - Warfarin, Clopidogrel, prescribed when an aneurysm is detected;
- immunoglobulins - administered intravenously, it is advisable to start treatment in the first 10 days of development of the pathology.
During treatment, the functioning of the heart and the condition of blood vessels are constantly monitored using angiography and ultrasound. If drug therapy does not help, surgical intervention is prescribed - stenting, bypass surgery.
Treatment process
Treatment of patients with Kawasaki syndrome is carried out in a hospital under the supervision of medical staff. There is no etiotropic therapy for the disease. Symptomatic treatment is aimed at relieving unpleasant symptoms and improving the general well-being of patients. Typically, doctors limit themselves to the use of conservative methods. To reduce mortality, it is necessary to prevent the development of coronary artery aneurysms. Surgical intervention is indicated in advanced cases in the presence of severe cardiovascular dysfunction.
Medicines used to treat the syndrome:
Immunoglobulin is administered parenterally immediately after the patient is admitted to the hospital. It reduces the severity of inflammation in blood vessels, has an antipyretic effect, and prevents the formation of aneurysms.- NSAIDs have anti-inflammatory and antipyretic effects, relieve joint pain, reduce swelling and severity of skin rashes - Piroxicam, Ortofen.
- Antiplatelet drugs prevent platelet aggregation, promote blood thinning, reduce blood clotting, and prevent thrombus formation - “Aspirin”, “Curantil”.
- Anticoagulant drugs slow down blood clotting, the conversion of fibrinogen into fibrin and the formation of blood clots - Clopidogrel, Warfarin.
- Glucocorticosteroids eliminate signs of inflammation, but do not affect the formation of coronary aneurysms. Their effectiveness in general is questioned by experts, since steroid hormones have a side effect in the form of blood thickening and the formation of blood clots.
When conservative therapy does not produce positive results, and pathological processes in the coronary vessels progress, they proceed to surgical treatment. To get rid of an aneurysm, patients undergo angioplasty and coronary artery bypass surgery. In the presence of coronary artery stenosis, stenting, catheterization and rotational ablation are performed.