Heart failure - symptoms and treatment
The following forms of heart failure are distinguished:
- left- and right-handed;
- systolic and diastolic (heart failure with reduced and preserved ejection fraction);
- acute and chronic.
Left ventricular failure
Left-sided heart failure can be left ventricular or left atrial. It is characterized by a decrease in left ventricular output and/or stagnation of blood on the way to the left parts of the heart, that is, in the veins of the pulmonary circulation.
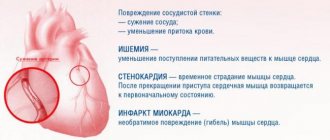
Left ventricular failure usually develops with coronary heart disease (CHD), hypertension, cardiomyopathy, congenital heart defects, heart valve insufficiency, and left atrial failure - with narrowing of the mitral valve opening and, in rare cases, with left atrial myxoma - a benign heart tumor [14].
Symptoms of left-sided heart failure (HF): weakness, dizziness, pale skin, shortness of breath and fatigue.
Right ventricular failure
Right ventricular failure is characterized by a decrease in right ventricular output and stagnation of blood in the veins of the systemic circulation. The condition is usually caused by pre-existing left ventricular failure or severe pulmonary disease [14].
Symptoms of right-sided heart failure: peripheral edema, cyanosis and fluid accumulation in the abdominal cavity.
Isolated heart failure is rare and short-lived. Subsequently, the disorder affects all chambers of the heart and typical symptoms of the disease develop.
Some sources use the term “global heart failure” to describe heart failure of both ventricles. This formulation is incorrect and is not used by doctors. In the literature, the term “total heart failure” is used to describe this condition [17].
Systolic and dystolic heart failure
Impaired pumping function of the left ventricle can be caused by systolic and diastolic dysfunction. Systolic dysfunction is more common and is associated with decreased contractility of the myocardium, the muscle tissue of the heart. In most cases, the cause of systolic chronic heart failure is coronary artery disease, combined with arterial hypertension and diabetes mellitus.
Diastolic dysfunction is caused by impaired active relaxation or increased myocardial stiffness. Patients with this form of the disease are less likely to suffer from coronary artery disease, and more often from arterial hypertension and atrial fibrillation. Among them there are more elderly people, women and obese patients[16].
In addition to the familiar terms “diastolic heart failure” and “systolic heart failure,” the names “ heart failure with preserved LV ejection fraction (HFpEF) ” and “heart failure with reduced ejection fraction (HFrEF)” .
We are talking about the same conditions, but the use of the terms diastolic and systolic HF requires objective evidence obtained using echocardiography, magnetic resonance imaging and isotope studies of the heart. In some sources, these terms are used as synonyms [14][18].
Symptoms for systolic and diastolic HF are similar [13]. These forms of the disease can only be distinguished using instrumental diagnostic methods. Many patients experience both types of dysfunction simultaneously [17].
Acute and chronic heart failure
Symptoms of chronic and acute heart failure differ only in intensity and timing of development.
Stages of development of heart failure
The modern classification of chronic heart failure combines the modified classification of the Russian School of Cardiology according to stages that can only worsen (V. Kh. Vasilenko, M. D. Strazhesko, 1935), and the international classification according to functional classes, which are determined by the patient’s ability to tolerate physical activity (6-minute walk test) and may worsen or improve (New York Cardiology Classification).[2]
Classification of CHF by the Russian Society of Heart Failure Specialists
| FC | FC of CHF (may change during treatment) | NK | Stages of CHF (do not change during treatment) |
| 1FC | There are no restrictions on physical activity; increased workload is accompanied by shortness of breath and/or slow recovery | 1 tbsp | Hidden heart failure |
| 11FC | Minor limitation of physical activity: fatigue, shortness of breath, palpitations | 11a st | Moderately severe hemodynamic disturbances in one of the circulation circles |
| 111FC | Noticeable limitation of physical activity: compared with usual activities, accompanied by symptoms | 11b st | Severe hemodynamic disturbances in both circulation circles |
| 1U FC | Symptoms of heart failure are present at rest and worsen with minimal physical activity. | 111st | Severe hemodynamic disturbances and irreversible structural changes in target organs. The final stage of damage to the heart and other organs |
New York Heart Association classification of heart failure
Class I: Heart disease does not limit physical activity. Normal exercise does not cause fatigue, palpitations or shortness of breath.
Class II. The disease slightly limits physical activity. There are no symptoms at rest. Normal physical activity causes fatigue, palpitations, or shortness of breath.
Class III. Physical activity is significantly limited. There are no symptoms at rest. Little physical activity causes fatigue, palpitations, or shortness of breath.
Class IV. Marked limitation of any physical activity. Symptoms of heart failure appear at rest and worsen with any activity [15].
What is shortness of breath (lack of air)?
Shortness of breath is not an independent disease, but evidence of disturbances in the functioning of the heart, respiratory organs, endocrine and nervous systems, and the presence of anemia. Severe shortness of breath is not always a symptom of a serious illness - its degree does not depend on the stage or degree of development of the underlying pathology.
Shortness of breath, indicating illness, should be distinguished from the usual lack of air, which occurs in any person, for example, when walking at a fast pace or under stress. If the feeling of lack of air occurs in a calm state and for no apparent reason, this is a good reason to visit a doctor as soon as possible. Now you can undergo a consultation and a set of preparatory examinations when registering for a course of enhanced external counterpulsation or shock wave therapy of the heart absolutely free of charge!
Promotion
Just until the end of autumn, undergo a free consultation and a set of preparatory examinations* when registering for a course of enhanced external counterpulsation or shock wave therapy of the heart.**
Send a request
* Check the details of the Promotion by phone. **Has contraindications; consultation with a doctor is required.
Enhanced external counterpulsation (EECP) Cardiac shock wave therapy (SWTS)
Hurry up to apply, the promotion period is limited.
What diagnostics do you need to undergo?
If the patient notices the appearance of tachycardia and shortness of breath at rest or accompanied by other symptoms, you should consult a doctor as soon as possible.
The first thing the doctor will do is take a thorough history. It is important to find out under what circumstances the patient notices symptoms (physical activity, stress, rest), whether there is heart pain, cough, general weakness, whether the person is taking any medications. Next, the doctor examines the patient in detail, including a visual examination of the mucous membranes and skin, measures pulse, blood pressure, palpation and auscultation.
Laboratory tests include a general blood and urine test, blood biochemistry; from instrumental - ECG, X-ray of the lungs. If necessary, an additional ultrasound of internal organs is performed and a consultation with specialists is prescribed. A carefully collected anamnesis and a properly selected examination are the main conditions for making a diagnosis.
What to do if you have shortness of breath?
Various types and types of shortness of breath (including shortness of breath after eating) are indicators of the presence of certain diseases. At the same time, lack of air in itself is not a disease and cannot be treated separately. We are talking about complex treatment of the cause of shortness of breath. To identify it, you need to contact a qualified specialist and undergo an examination using modern equipment. Only after this can we pinpoint exactly what is causing the breathing difficulty and create an individual treatment program for the patient.
Do not delay in seeing a doctor. In certain diseases, shortness of breath can develop into suffocation, which has a sharply negative effect on brain function. Every time you put off going to the clinic after an attack of shortness of breath, your condition only gets worse.
Treatment of cardiac dyspnea (lack of air) at the CBCP clinic
If there is a suspicion of cardiac pathology causing symptoms of shortness of breath, contact the International Center for Pathology of the Circulatory Organs. We offer high-quality diagnostics using expert-class equipment. You will be able to obtain objective and detailed information about the condition of your body.
At CBCP, you have at your disposal experienced high-level cardiologists and cardiac surgeons (including pediatric ones), certified specialists in functional and ultrasound diagnostics. You will be offered non-surgical treatment of cardiovascular diseases using modern methods used in Europe, Israel and the USA.
2. Drug treatment of the disease
To treat COPD, medications are also used that can perform different functions. Yes, bronchodilators
help open the bronchi, which in turn makes breathing easier. These medications may be short-acting (to quickly relieve symptoms of the disease) or long-acting to help prevent them.
Anti-inflammatory drugs
to treat COPD symptoms (such as corticosteroids) may come in the form of tablets or inhalers that help the medicine go directly to the lungs.
Visit our Pulmonology page
Causes of paroxysmal tachycardia
In addition to sinus tachycardia, paroxysmal tachycardia is distinguished. It differs in that the impulse causing heart contractions does not come from the sinus node, but from other, pathological pacemakers. With this type of tachycardia, the heart rate reaches 180 - 240 beats per minute. This condition can occur against the background of various heart lesions, so it is best to consult a cardiologist. The symptoms of paroxysmal tachycardia are very specific:
- rapid heartbeat,
- dyspnea,
- weakness,
- feeling of tightness in the chest,
- pale skin,
- pulsation of the neck veins.
Shortness of breath when walking, exertion
In older people, shortness of breath most often occurs when walking, quite often severe. The reasons for this lie in the natural aging of the body. With age, the heart muscles and coronary vessels lose tone and are no longer able to maintain blood circulation at the same volume. Depending on the degree of thinning of the vascular walls, damage to the myocardium, certain physical activities are sufficient for a person to experience a feeling of lack of air. Some patients experience shortness of breath after climbing stairs to the upper floors. For others, for the same effect, it is enough to walk about 100 meters.
Types of shortness of breath
- expiratory,
- inspiratory,
- mixed.
Medicine knows 3 main types of shortness of breath:
- Inspiratory dyspnea causes difficulty breathing.
- Expiratory shortness of breath is, on the contrary, problems with exhalation.
- The mixed type is characterized by respiratory failure during inhalation and exhalation.
Based on the reasons for development, there are:
- cardiac;
- central;
- pulmonary;
- hematogenous dyspnea.
Types of shortness of breath are determined according to how deep and often the breath is taken:
- rapid (tachypnea);
- rare (bradypnea);
- rare and superficial (oligopnea);
- rapid and deep (hyperpnea and polypnea).
Respiratory failure as a cause of tachycardia
Decreased function of the respiratory system affects the functioning of the heart. The mechanism of tachycardia is approximately the same as with anemia, because if lung function deteriorates, a lack of oxygen occurs. There are many diseases that lead to respiratory failure, and they all have their own symptoms. Their most common signs, along with rapid heartbeat, are:
- difficulty inhaling or exhaling,
- feeling of suffocation
- the need to strain additional muscles during breathing (abdominal muscles, shoulder girdle),
- sleep and memory disturbances,
- headache,
- cough.
If palpitations are accompanied by such symptoms, you should definitely consult a pulmonologist, and if this is not possible, then consult a therapist.