© Author: A. Olesya Valerievna, candidate of medical sciences, practicing physician, teacher at a medical university, especially for SosudInfo.ru (about the authors)
Sinoatrial block (sinoauricular, SA block) is considered one of the variants of sick sinus syndrome (SU). This type of arrhythmia can be diagnosed at any age; it is recorded somewhat more often in males; it is relatively rare in the general population.
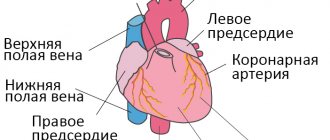
In a healthy heart, the electrical charge is generated in the sinus node, which is located deep in the right atrium. From there it spreads to the atrioventricular node and the bundle branches. Due to the sequential passage of the impulse through the conductive fibers of the heart, the correct contraction of its chambers is achieved. If an obstacle arises in any of the areas, then the reduction will also be disrupted, then we are talking about a blockade.
With sinoatrial blockade, the reproduction or propagation of the impulse to the underlying parts of the conduction system from the main, sinus node is disrupted, therefore the contraction of both the atria and ventricles is disrupted. At a certain moment, the heart “misses” the impulse it needs and does not contract at all.
Different degrees of sinoatrial block require different therapeutic approaches. This disorder may not manifest itself at all, or may cause fainting and even death of the patient. In some cases, sinoatrial blockade is permanent, in others it is transient. In the absence of a clinic, you can limit yourself to observation; a 2-3 degree blockade requires appropriate treatment.
Causes of sinoatrial block
Among the main mechanisms of sinoauricular blockade are damage to the node itself, disruption of the propagation of impulses through the heart muscle, and changes in the tone of the vagus nerve.
In some cases, the impulse is not formed at all, in others it is there, but too weak to cause contraction of cardiomyocytes. In patients with organic damage to the myocardium, the impulse encounters a mechanical obstacle in its path and cannot pass further along the conducting fibers. Insufficient sensitivity of cardiomyocytes to electrical impulses is also possible.
Factors leading to sinoauricular block are considered:
- Heart defects;
- Inflammatory changes in the heart (myocarditis);
- Cardiovascular form of rheumatism;
- Secondary damage to heart tissue due to leukemia and other neoplasms, injuries;
- Coronary heart disease (cardiosclerosis, post-infarction scar);
- Myocardial necrosis (infarction);
- Cardiomyopathy;
- Vagotonia;
- Intoxication with drugs when the permissible dose is exceeded or individual intolerance - cardiac glycosides, verapamil, amiodarone, quinidine, beta-blockers;
- Organophosphorus poisoning.
The operation of the SA is influenced by the activity of the vagus nerve, therefore, when it is activated, impulse generation may be disrupted and SA blockade may occur. Usually in this case they talk about transient SA blockade, which appears on its own and goes away in the same way. This phenomenon is possible in practically healthy people, without anatomical changes in the heart itself. In isolated cases, idiopathic sinoauricular block is diagnosed when the exact cause of the pathology cannot be determined.
In children, conduction disturbances from the sinoatrial node are also possible. Typically, such arrhythmia is detected after 7 years of age, and a common cause is autonomic dysfunction, that is, the blockade is more likely to be transient, against the background of increased tone of the vagus nerve. Among the organic changes in the myocardium that can cause this type of blockade in a child are myocarditis, myocardial dystrophy, in which, along with SA blockade, other types of arrhythmias can be detected.
Stage 1 symptoms
At an early stage, there are no manifestations at all or they are scanty. The clinical picture consists of two signs:
- Severe shortness of breath. But only after intense physical activity. The average person is not active enough to notice a deviation from the norm. In part, problems can be suspected based on the results of specialized tests (bicycle ergometry), but such a test is prescribed only when indicated.
- Tachycardia. Acceleration of the heart rate due to excessive generation of an electrical impulse, against the background of incomplete conduction of the signal to the ventricles. The compensatory mechanism is activated. But he is initially flawed, unable to influence the state of things. Both signs are revealed only after intense physical exertion. An ordinary person does not notice the problem, so diagnosis at stage 1 is almost impossible.
Types (types and degrees) of sinoatrial blockade
Depending on the severity of the arrhythmia, there are several degrees of it:
- SA blockade 1st degree (incomplete), when changes are minimal.
- SA blockade 2nd degree (incomplete).
- SA blockade 3rd degree (complete) is the most severe, the contraction of both the ventricles and atria is impaired.
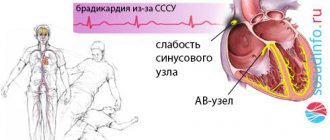
With 1st degree block of the sinus node, the node functions, and all impulses cause contraction of the atrial myocardium, but this happens less frequently than normal. The impulse through the node passes more slowly, and therefore the heart contracts less often. It is impossible to record this degree of blockade on an ECG, but it is indirectly indicated by rarer, as expected, heart contractions – bradycardia.
With sinoatrial blockade of the 2nd degree, the impulse is no longer always formed, resulting in a periodic absence of contraction of the atria and ventricles of the heart. It, in turn, comes in two types:
- SA blockade 2nd degree, type 1 - the conduction of the electrical signal through the sinus node gradually slows down, as a result of which the next contraction of the heart does not occur. The periods of increase in the pulse conduction time are called Samoilov-Wenckebach periods;
- SA blockade of the 2nd degree, type 2 – contraction of all parts of the heart occurs after a certain number of normal contractions, that is, without periodic slowing down the movement of the impulse along the SA node;
Sinoauricular block of the 3rd degree is complete, when the next heart contraction does not occur due to the lack of impulses from the sinus node.
The first two degrees of blockade are called incomplete, since the sinus node, although abnormal, continues to function. The third degree is complete, when impulses do not reach the atria.
The essence of the violation
In the normal state of affairs, the muscular organ works autonomously and does not need external stimulation. Uninterrupted functioning is ensured by the presence of a special accumulation of active cardiomyocyte cells - the sinus node. It is located in the right atrium.
The job of this anatomical structure is to generate an electrical impulse that causes the other chambers to contract.
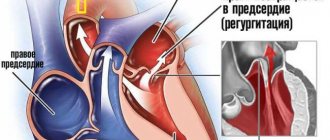
With sinoatrial (SA) blockade, the generation or propagation of an impulse into the underlying chambers of the heart is disrupted. The result is the impossibility of proper stimulation of the ventricles.
Since they do not receive the necessary command, a full reduction does not occur either. The body strives to compensate for this situation. The cameras begin to produce a signal themselves and become spontaneously excited.
But on the one hand, the intensity is not enough for a high-quality release of blood, on the other, the ventricles stop coordinating actions.
The contractions turn out to be chaotic and disorderly. Fibrillation develops, which most likely leads to cardiac arrest.
Another point is the excessive activity of the sinus node itself. This is another compensatory mechanism. The organ begins to produce impulses more often in order to somehow reach the ventricles.
As a result, a patient with advanced sinoatrial block has a history of two dangerous processes: tachycardia as a result of excessive work of the natural pacemaker and fibrillation.
It is difficult not to notice these signs, so diagnosis is prescribed in relatively early stages. Although the situation described is not always so critical. A patient can live with the pathology for years without even suspecting any problems.
Features of ECG with SA blockade
Electrocardiography is the main way to detect heart blocks, through which uncoordinated activity of the sinus node is detected.
SA blockade of the 1st degree does not have characteristic ECG signs; it can be suspected by bradycardia, which often accompanies such blockade, or shortening of the PQ interval (not a constant sign).
The presence of SA blockade can be reliably confirmed by ECG starting from the second degree of disorder, in which full cardiac contraction does not occur, including the atria and ventricles.
On the ECG at stage 2 the following are recorded:
- Lengthening the interval between atrial contractions (A-P), and during the loss of one of the next contractions this interval will be two or more normal;
- Gradual decrease in R-R time after pauses;
- Absence of one of the next PQRST complexes;
- During long periods of absence of impulses, contractions may occur generated from other sources of rhythm (atrioventricular node, bundle branches);
- If not one, but several contractions occur at once, the duration of the pause will be equal to several R-R, as if they were occurring normally.
Complete blockade of the sinoatrial node (3rd degree), is considered when an isoline is recorded on the ECG, that is, there are no signs of electrical activity of the heart and its contraction, and is considered one of the most dangerous types of arrhythmia, when there is a high probability of death of the patient during asystole.
Manifestations and diagnostic methods of SA blockade
The symptoms of sinoatrial block are determined by the severity of disorders in the conductive fibers of the heart. In the first degree, there are no signs of blockade, as well as the patient’s complaints. With bradycardia, the body “gets used” to a rare pulse, so most patients do not experience any worries.
SA blockades of 2 and 3 degrees are accompanied by tinnitus, dizziness, discomfort in the chest, and shortness of breath. Against the background of a slower rhythm, general weakness is possible. If SA blockade has developed due to a structural change in the heart muscle (cardiosclerosis, inflammation), then an increase in heart failure is possible with the appearance of edema, cyanosis of the skin, shortness of breath, decreased performance, and enlarged liver.
In a child, the signs of SA blockade differ little from those in adults. Parents often pay attention to decreased performance and fatigue, blue discoloration of the nasolabial triangle, and fainting in children. This is the reason to contact a cardiologist.
If the interval between heart contractions is too long, then Morgagni-Adams-Stokes (MAS) paroxysms may occur, when the flow of arterial blood to the brain is sharply reduced. This phenomenon is accompanied by dizziness, loss of consciousness, noise, ringing in the ears, possible convulsive muscle contractions, involuntary emptying of the bladder and rectum as a result of severe brain hypoxia.
syncope with MAS syndrome due to sinus node blockade
Suspicion of the presence of a blockade in the heart arises already during auscultation, during which the cardiologist records bradycardia or loss of the next contraction . To confirm the diagnosis of sinoauricular block, the main methods are electrocardiography and 24-hour monitoring.
Holter monitoring can be performed for 72 hours. Long-term ECG monitoring is important in those patients in whom, if the presence of arrhythmia is suspected, no changes could be detected in a regular cardiogram. During the study, a transient blockade, an episode of SA blockade at night or during physical activity may be recorded.
Children also undergo Holter monitoring. The detection of pauses lasting more than 3 seconds and bradycardia of less than 40 beats per minute is considered diagnostically significant.
A test with atropine is indicative. The introduction of this substance to a healthy person will cause an increase in the frequency of heart contractions, and with SA blockade, the pulse will first double, and then just as rapidly decrease - a blockade will occur.
To exclude other cardiac pathologies or search for the cause of the blockage, an ultrasound of the heart can be performed, which will show the defect, structural changes in the myocardium, scarring area, etc.
Forecast
Relatively favorable against the background of systematic drug treatment.
If a pacemaker is implanted and the operation is successful, survival rate increases dramatically to 90-95% over a period of 10 years or more.
Lack of therapy is associated with an almost 100% chance of death within a short period of time.
The pathological process cannot always be cured surgically. For some patients, with severe heart defects, severe concomitant conditions, or old age, surgery may be contraindicated.
However, the chance cannot be neglected. First they try to stabilize the patient, then they still consider radical intervention. Otherwise there is no chance of recovery.
Treatment
1st degree SA blockade does not require specific therapy. Usually, to normalize the rhythm, it is enough to treat the underlying disease that caused the blockade, normalize the daily routine and lifestyle, or discontinue medications that could disrupt the automatism of the sinus node.
Transient SA blockade against the background of increased activity of the vagus nerve is well treated by prescribing atropine and its drugs - bellataminal, amizil. The same medications are used in pediatric practice for vagotonia, which causes transient blockade of the sinus node.
Attacks of SA blockade can be treated medicinally with atropine, platyphylline, nitrates, nifedipine, but, as practice shows, the effect of conservative treatment is only temporary.
Patients with sinus node blockade are prescribed metabolic therapy aimed at improving myocardial trophism - riboxin, mildronate, cocarboxylase, vitamin and mineral complexes.
If SA blockade is recorded, you should not take beta blockers, cardiac glycosides, cordarone, amiodarone, or potassium supplements, as they can cause even greater difficulty in the automaticity of the SA and worsen bradycardia.
If blockade of the SA node leads to pronounced changes in well-being, causes an increase in heart failure, and is often accompanied by fainting with a high risk of cardiac arrest, then the patient is offered to have a pacemaker implanted. Indications may also include Morgagni-Adams-Stokes attacks and bradycardia below 40 beats every minute.
In case of sudden severe blockade with Mroganyi-Adams-Stokes attacks, temporary cardiac stimulation is necessary, chest compressions and artificial ventilation are indicated, atropine and adrenaline are administered. In other words, a patient with such attacks may require full resuscitation measures.
If the exact reasons for the development of sinoatrial block have not been established, there are no effective measures to prevent this phenomenon. Patients who have already recorded changes in the ECG should correct them with the help of medications prescribed by the cardiologist, normalize their lifestyle, and also regularly visit the doctor and have an ECG taken.
Children with arrhythmias are often advised to reduce the overall level of exercise and reduce participation in sports sections and clubs. Visiting children's institutions is not contraindicated, although there are experts who advise limiting the child in this too. If there is no risk to life, and episodes of SA blockade are rather isolated and transient, then there is no point in isolating the child from school or going to kindergarten, but observation at the clinic and regular examination are necessary.