25.10.2019
Stroke in childhood: features of the disease in children and treatment
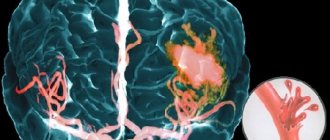
Stroke occurs less frequently in children than in adults and the elderly, but its consequences are no less dangerous. Untimely diagnosed hemorrhagic and ischemic strokes in childhood can cause disability and death, which makes the issue of identifying them at an early stage important for every parent.
Statistics
Stroke is considered to be a disease of older people: according to statistics, 7.3%-10.5% of men and women aged 70-80 years suffer from this disease. Children are less likely to receive this diagnosis because they are less exposed to the risk factors associated with its occurrence.
Most often, a stroke in a child occurs in the prenatal or early neonatal period: 1 case in 4000 newborns. Children under 3 years of age have an increased risk of developing pathology, accounting for 38% of the total number of diagnosed strokes.
Boys are more likely to suffer from this problem; in girls, the risk of developing the disease increases during adolescence. Preschoolers and adolescents have fewer strokes than infants: 1-2 per 100,000 people.
Treatment and rehabilitation after stroke
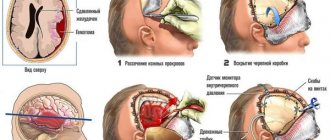
Treatment of children who have suffered a hemorrhagic stroke concentrates on stabilizing the condition and eliminating the consequences of cerebral hemorrhage. The same children, but who have suffered an ischemic stroke, will most likely have to take a course of blood thinning medications.
Post-stroke recovery measures for such children will be aimed at restoring physical functions. Recovery must begin as soon as possible. Recovery will last on average from six months to two years or longer.
Causes
Perinatal and fetal strokes may depend on the mother's lifestyle, her health status and the course of pregnancy.
Among the main risk factors in this case are:
- smoking, maternal use of drugs and alcohol;
- chronic hypertension, frequent crises;
- placental abruption at different stages, due to which the fetus felt a lack of oxygen;
- diabetes;
- infectious diseases of various types;
- rupture of the membranes before the onset of labor, which resulted in earlier rupture of amniotic fluid.
Newborns often suffer as a result of birth injuries, manifestations of congenital and acquired diseases in the first days of life. In adolescents, the causes of strokes include traumatic brain injuries, high psycho-emotional stress and drug use.
Risk factors in newborns
The causes of stroke in infants are often associated with congenital pathologies and the course of labor. This group accounts for more than 30% of all childhood strokes.
Among the main causes of the disease in children are:
- injuries to the brain, skull, and cervical vertebrae received during childbirth;
- intrauterine infections and fetal hypoxia, pathologies of various origins during pregnancy;
- difficult and long labor that caused hypoxia;
- neoblastic processes;
- early or late birth;
- compression of the spinal artery;
- bacterial endocarditis;
- Wergolf's disease, diseases associated with blood clotting processes and leading to the formation of blood clots;
- genetically transmitted diseases, including Moya-Moya disease, which manifests itself in narrowing of the intracranial arteries;
- sickle cell anemia, which is more common in children with dark skin color;
- cerebral ischemia;
- meningitis, neuroinfections, chickenpox, which increases the risk of stroke by 3 times.
Risk factors in preschoolers
In preschool children, the disease is less common. In children over 3 years of age, one of the main causes of ischemic stroke is blood diseases, which, according to various sources, affect from 15% to 50% of children. Increased activity of a child at this age causes head and neck injuries, which can cause a stroke.
Other reasons include:
- TBI, often after a fall;
- acute poisoning;
- vitamin deficiency, deficiency of iron and vitamin C;
- first manifestations of arterial hypertension;
- blood diseases, including aplastic anemia and leukemia;
- endocarditis;
- vasculitis;
- aneurysms.
- The causes of ischemic circulatory disorders are called:
- diabetes;
- viruses affecting blood vessels, inflammation of the meninges and brain;
- congenital heart disease or its valves, cerebral vascular pathologies, arteriovenous malformation;
- oncological diseases;
- autoimmune and metabolic diseases.
severe dehydration leading to blood thickening;
Teenagers are the most protected category of children. The causes of problems with impaired blood supply to the brain described above occur less frequently in them. Risk factors at this age include high rates of injury, use of illegal and harmful drugs, high emotional stress and nervous strain.
results
During the perinatal period (from the moment of birth to the 28th day of life), 16 (11.43%) children with G.I. Over 28 days of life, 124 (88.57%) children were hospitalized. Children of the 2nd and 3rd months of life predominated - 117 (83.57%): 2nd month - 101 (72.14%) children, 3rd month - 16 (11.43%). At the age of 4 months to 1 year, 7 (5.0%) patients with HI were hospitalized.
Among the complaints (parents) indicated lethargy in 101 (72.14%) patients, which in 16 (11.42%) children turned into drowsiness, and in 1 child into loss of consciousness. In 39 (27.86%) children, the disease began with anxiety, in 19 (13.57%) monotonous crying appeared, 89 (63.57%) children at the onset of HI refused breastfeeding, in 20 (14.28%) regurgitation occurred, and 66 (47.14%) had vomiting. 21 (15.0%) children had seizures. In 7 (5%) patients, tilting of the head was detected. 101 (72.14%) patients had pale skin, 2 (1.42%) had icteric skin discoloration. 10 (7.14%) children had skin rashes, 1 had mucous membranes, 1 had bruises on the face, and 1 patient had nosebleeds. In 4 (2.85%) children, the absence of movements in the right or left upper limb, as well as the right or left lower limb, was recorded. 29 (20.71%) children had a cough, 11 (7.85%) had groaning breathing, and 3 (0.80%) had respiratory arrest. Diarrhea and loose stools were noted in 7 (5.0%) children, and 3 (2.14%) had blood in the stool. In 3 (2.14%) patients, parents noted purulent discharge from the eyes. Parents recorded an increase in body temperature up to 37-37.9 °C in 29 (20.71%) children, within 38-38.9 °C - in 49 (35.0%), above 39 °C - in 8 ( 5.71%) patients.
Neuroimaging examination at the time of admission to the hospital revealed a high frequency of SAH - in 32 (22.85%) children, as well as such clinical and anatomical forms of SAH as combined subarachnoid-parenchymal hemorrhage - in 24 (17.14%) patients, SAH in combination with non-traumatic subdural hematoma - in 15 (10.71%) cases, SAH and ventricular hemorrhage - in 6 (4.28%) children. Mixed subarachnoid-parenchymal and non-traumatic subdural hemorrhage was observed in 18 (12.85%) patients, subarachnoid-parenchymal and ventricular hemorrhage - in 13 (9.28%) patients, subarachnoid-parenchymal, ventricular, subdural hemorrhage - in 2 (1, 42%). Much less frequently, 1 child had mixed subarachnoid-ventricular and subdural hemorrhage. In 8 (5.71%) children, the reason for hospitalization was non-traumatic subdural hematoma, in 8 (5.71%) - non-traumatic subdural hematoma and parenchymal hemorrhage, in 7 (5.0%) - isolated parenchymal hemorrhage. In 2 (1.42%) patients, HI was represented by parenchymal and ventricular hemorrhage, in 4 (2.85%) - isolated ventricular hemorrhage.
A neurological examination of children upon admission to the hospital revealed the presence of both meningeal and focal neurological symptoms, as well as signs of increasing intracranial hypertension and the formation of cerebral edema.
The GCS score in 3 (2.14%) cases was 15 points, in 29 (20.71%) - 12 points, in 39 (27.86%) - 9 points, in 29 (20.71%) - 7 points, in 37 (26.43%) - 5 points, in 3 (2.14%) cases - 4 points.
102 (72.85%) patients had a meningeal symptom complex, represented by stiffness of the neck muscles. 38 (27.14%) children had convulsions, 7 (5.0%) had hyperesthesia. Impaired thermoregulation manifested itself in the form of hyperthermia, which was detected in 91 (65.0%) patients on the day of hospitalization. An increase in body temperature up to 37-37.9 °C was recorded in 31 (22.14%) children, within 38-38.9 °C - in 56 (40.0%) children, above 39 °C - in 4 ( 2.85%) of patients, which was probably due to concomitant infectious pathology [29].
Common clinical manifestations of HI in infants were: increase in intracranial pressure, formation of cerebral edema. At the same time, 125 (89.28%) children had bulging and tension of the large fontanel. In 3 (2.14%) cases, the large fontanelle, on the contrary, sunk. Only 12 (8.57%) children had a satisfactory condition of the large fontanel.
The diffuse nature of brain damage due to progressive intracranial hypertension and cerebral edema was accompanied by floating movements of the eyeballs in 29 (20.71%) children.
The syndrome of motor disorders was manifested by hemiparesis in 17 (12.14%) and tetraparesis in 1 child. Impaired motor reactions in the form of limited movements in the limbs on the right were observed in 6 (4.29%) patients, on the left - in 11 (7.85%), which indicated a predominant lesion of the right hemisphere of the brain. Extrapyramidal movement disorders were manifested by changes in muscle tone in the form of hypertension in 98 (70.0%) patients, and in the form of hypotension in 35 (25.0%) children. Muscle atony was observed in 4 (2.86%) children. Only 3 (2.14%) patients had satisfactory muscle tone. In 103 (73.57%) cases, high tendon reflexes with expansion of reflexogenic zones were noted. Decreased tendon reflexes were observed in 29 (20.74%) patients, areflexia - in 3 (2.14%). Tongue deviation to the right was detected in 3 (2.14%) patients.
The results of the study of the pupils showed the same size in 73 (52.14%) children, right-sided pupil dilation was observed in 36 (25.72%), left-side dilation - in 31 (22.14%) patients. Optic nerve palsy was manifested by a decrease in the reaction of the pupils to light in 54 (38.57%) children, and the absence of a reaction of the pupils to light in 12 (8.57%). The photoreaction of the pupils was determined in 74 (52.85%) cases.
41 (29.28%) children had horizontal, 3 (2.14%) children had vertical nystagmus. 101 (72.14%) patients had a positive Babinski reflex.
Paralysis of the facial nerve was manifested by flattening of the nasolabial fold on the left in 23 (16.42%) children, on the right - in 2 (1.42%). Lagophthalmos was observed in 2 (1.42%) cases.
Damage to the upper parts of the brainstem and oculomotor nerve palsy manifested as strobism in 26 (18.57%) patients. Oculomotor disorders were also accompanied by ptosis on the right in 9 (6.42%) cases, on the left - in 3 (2.14%) cases. A negative corneal reflex was found in 16 (11.42%) children.
Paresis of upward gaze was detected in 1 child, paresis of gaze to the left - in 6 (4.28%), paresis of gaze to the right - in 2 (1.42%).
One child was diagnosed with aphonia. Bulbar disorders with dysfunction of swallowing, sucking and a negative pharyngeal reflex were registered in 44 (31.42%) children. Assessment of vital functions revealed bradycardia (less than 70 beats/min) in 42 (30.0%) patients, moderate and severe tachycardia with a heart rate over 120 beats/min in 95 (67.85%) children. Age-appropriate heart rhythm was observed in 3 (2.14%) patients. In most cases, 102 (72.85%) children had hyperventilation disorders in the form of tachypnea (40 respiratory movements in 1 minute or more) with the participation of auxiliary muscles. Bradypnea with a respiratory rate of less than 30 respiratory movements per minute or apnea (breathing cessation for more than 15 seconds) was recorded in 38 (27.15%) children. Vegetative signs were pale skin in 31 (22.14%) patients. However, 59 (42.14%) patients had icteric discoloration of the skin. Petechial rashes on the skin were detected in 1 (0.71%) child, petechial hemorrhage on the palate - in 10 (7.14%) children. An increase in liver size was found in 61 (43.57%) children. Gastrointestinal bleeding was observed in 3 (2.14%) cases, frequent bowel movements - in 5 (3.57%) children, decreased urination - in 5 (3.57%) patients, purulent discharge from the eyes - in 4 (2 .85%) patients.
How does the disease manifest itself?
Symptoms of problems with blood supply to the brain are the same in children and adults. The difficulty of timely diagnosis lies in the fact that infants are not capable of full communication. Unlike adults, whose symptoms are immediately visible, children cannot explain their feelings, which makes it difficult to make a diagnosis.
The problem becomes more complex in newborns, whose response to stroke is similar to that of external stimuli. It is important for parents to carefully monitor the behavior of a child of any age and, at the first suspicion of a stroke, call an ambulance, since delay can have consequences for the baby’s health.
When to suspect a child is having a stroke
Often, signs of vascular pathologies in young children go unnoticed because they pass without symptomatic manifestations.
In order not to miss the onset of the disease, you should pay close attention to the appearance of the following signs in the child’s behavior:
- severe headache, dizziness, visual and hearing impairment, loss of consciousness;
- causeless nausea and vomiting;
- when smiling, the corners of the lips rise only on one part of the face;
- coordination of movements is impaired: when you try to raise both hands in front of you, one will not obey;
- speech becomes inarticulate, reactions become inhibited, consciousness becomes confused;
- one of the eyes may begin to squint, and a sharp deterioration in vision is detected.
4 main symptoms
Among the mass of accompanying manifestations, 4 main symptoms of childhood stroke can be distinguished:
- Complete or partial paralysis of the limbs, in most cases the inability to move an arm or leg on one side, sagging of the right or left half of the body, impaired coordination.
- Signs of fog and confusion, stupor, and in severe cases - coma.
- In older children - speech impairment, distortion of words, inability to repeat entire sentences, slurred and inhibited speech.
- Sharp and repeated cramps in the limbs, muscle tension in the back of the head and neck.
“You, mom, actually found something to tell!”
“I first searched for rehabilitation for Ilya on the Internet,” says Anna. – The free rehabilitation center offers five minutes of massage, that’s all. And we constantly need a massage therapist, a physical therapy teacher, and a speech therapist. After all, Ilya not only has to develop new skills, but he also has to maintain what he has.”
“I lift a stick, squat and can climb onto a step,” Ilya intervenes in a serious conversation with a journalist and pulls out a step platform from under the bed, as if for aerobics. - No problem!" But he immediately collapses: “That’s it, I can’t take it anymore, I’m tired.”
Anna says that Ilya started talking at the age of three, and started walking when he was three and a half. And yet, only recently have I started walking up the stairs like an adult, rather than putting both feet on each step like a toddler. But my left hand still doesn’t work at all.
There was a period when Ilya walked on his toes all the time.
The orthopedist even advised cutting his Achilles tendon, but in the end, mother and son strained his leg through training. They just deliberately stood with their legs supported and cried.
“On what other toes? You, mom, actually found something to tell, that’s when it happened!” – Ilya drawls, clearly repeating his father’s intonation. And then he pulls out a guitar and begins to sing, plucking the strings with one right hand.
“Okay, we have now found rehabilitation, which we have in Noginsk - “Development without barriers,” continues the mother. – What I like about them is that as a child, they finally began to study comprehensively. There was a period when it was actively growing. At this time we were developing the leg. Then the massage therapist worked on the hand, and at the same time the speech therapist gave us a letter. Ilya, of course, is lagging behind, but now he has begun to maintain his balance.”
Now the mother closely monitors her son’s activities. She also provides him with motivation. He may say, for example: “If you don’t do the exercises, you won’t watch the cartoon.” And Ilya tries, he does.
The fight for knowledge
It’s still not easy for Ilya to study. At nine years old, he is in first grade, mastering the eighth grade program. True, from home.
“The correctional school is located fifteen kilometers from home. There are fifteen people in the class. When we started studying, Ilya could sit quietly for about twenty minutes. Now, according to the teacher, he can endure a lesson for forty minutes. But there are three lessons at school. That's why I haven't decided to send him to class yet. The teacher comes to our house,” Anna clarifies.
“Teacher Anastasia Alexandrovna,” Ilya adds busily. – We read and write with her. Have you seen the series “Dog”?”
Ilya masters the educational material unevenly. Mathematics goes back and forth, writing and reading are worse, but he can’t even see a textbook on the world around him, he doesn’t like this subject so much. The seasons are difficult for him, he doesn’t recognize animals well – maybe that’s why he doesn’t like this subject.
The family's plans for Ilya's future are modest.
“I certainly don’t hope that he will graduate from college. I would be able to read, count and look after myself. But you can’t imagine how responsive and grateful he is.”